See also
Pertussis/Whooping cough
Asthma
Foreign body
Croup
Key points
- The most common cause of cough is an upper respiratory tract infection (usually viral in nature)
- Investigations and treatment are rarely required for well children with a short history of cough
- Children who have a persistent daily cough lasting >4 weeks should be assessed and investigated with a CXR and spirometry (if able), with consideration given to further investigations and management
Background
- Cough is a common symptom and for most children is self-limiting
- Young children develop 6-12 respiratory tract infections per year, usually accompanied by cough. In most children, the cough is self-limiting, most resolve without treatment in 1-3 weeks
- For healthy children with a short history of cough (
<4 weeks) and no red flags, further investigation and management is not required
- Key definitions
- Acute cough: lasting up to 2 weeks
- Protracted acute cough: daily cough lasting 2-4 weeks
- Chronic cough: daily cough lasting >4 weeks
- Specific cough: cough occurring with condition known to be cause of chronic cough
- Non-specific cough: chronic cough without a defined cause (in children this will usually undergo spontaneous resolution)
- Chronic cough warrants further assessment
The most common cause of cough in children is a viral upper respiratory tract infection or post-infectious cough. The likelihood of other causes depends on clinical findings, cough duration and whether the cough is wet or dry.
The table below outlines common causes of cough.
|
Dry |
Wet |
| Acute |
- Respiratory infections (most commonly viral)
- Foreign body inhalation
- Exposures (eg smoking, vaping, irritants, medications)
|
- Respiratory infections (most commonly viral)
|
| Chronic |
- Respiratory infection (post-infectious cough, including pertussis)
- Asthma
- Habit cough and somatic cough disorder
- Congenital airway abnormalities (eg tracheo/bronchomalacia, vascular rings, tracheo-oesophageal fistula)
- Interstitial lung disease
|
- Protracted bacterial bronchitis (PBB)
- Recurrent aspiration (can be associated with neurodevelopmental disabilities, congenital airway abnormalities)
- Chronic infection (tuberculosis, lung abscess, etc)
- Foreign body inhalation
- Bronchiectasis/chronic suppurative lung disease (due to post-infectious, CF, immunodeficiency, primary ciliary dyskinesia)
- Chronic atelectasis (intrinsic or extrinsic airway obstruction)
|
Assessment
Initial assessment
- determine duration of cough and whether wet or dry
- elicit red flag symptoms or findings that may indicate serious underlying disease
- identify causes of specific cough or recent respiratory infections
History
| Feature on history |
Description (including specific conditions not to be missed in assessment of chronic cough) |
| Quality |
Wet or dry (listen to sound of wet cough here) |
| Duration |
Distinguish chronic cough from recurrent acute viral infections (fevers, coryza, daycare attendance) |
| Onset/triggers |
Sudden onset without viral prodrome (or after choking episode) may suggest foreign body inhalation
Onset in early infancy may suggest aspiration, congenital airway abnormality or cystic fibrosis
Choking or coughing with feeding may suggest aspiration
Association with exercise, environment changes, smoke/pets/dust exposures may suggest asthma (and/or allergic rhinitis)
|
| Frequency |
Determine whether cough episodes occur occasionally or frequently through the day and/or night
Number of episodes of chronic wet cough in a year is important to identify children who may need further investigation for chronic suppurative lung disease (>3 episodes of PBB in 12-month period warrants referral/further
investigation)
|
| Timing |
Specific patterns (worsening or improving at certain times of the day) may suggest conditions such as GORD, post-nasal drip/sinusitis (worse when lying flat), asthma (tends to exacerbate at night, with exercise), somatic cough disorder (absent during sleep) or chronic suppurative lung disease (worse on waking) |
| Sputum |
Presence of haemoptysis, colour, consistency and volume |
| Type |
Daily, persistent, wet, often in morning: protracted bacterial bronchitis (PBB), chronic suppurative lung disease, bronchiectasis
Paroxysmal: pertussis or foreign body
Staccato: suggestive of chlamydia (in infants)
Barking or seal-like (+/- stridor): croup
Dry +/- wheeze: asthma
Dry, honking, barking, distractible, suggestible: tic or somatic cough disorder
|
| Underlying medical conditions |
Neurodevelopmental disorders, dysphagia, neuromuscular disorders, immunodeficiency, congenital cardiac disease |
| Family and social history |
Infectious contacts
Travel history
Exposure to smoking or vaping (personal or passive)
Immunisation status
Family history of chronic lung disease, atopy, cystic fibrosis, tuberculosis
|
Examination
- Fever, coryza or other signs of acute infection
- Increased work of breathing, hypoxia, stridor, chest signs (wheeze, crackles, crepitations)
- Faltering growth (or growth failure)
- Signs of cardiac failure (oedema, hepatomegaly, heart murmur)
- Signs of chronic suppurative lung disease/bronchiectasis (clubbing, poor growth, chest wall deformity)
- ENT examination for signs of rhinosinusitis
Red flags in chronic cough
- Shortness of breath (at rest or exertional)
- Recurrent episodes of chronic or wet or productive cough
- Recurrent pneumonia
- Chest pain
- Haemoptysis
- Systemic symptoms (fever, weight loss, growth failure)
- Neurodevelopmental abnormality
- Feeding difficulties (including choking/vomiting)
- Stridor and other respiratory noises
- Abnormal clinical respiratory examination (eg crackles, digital clubbing)
- Abnormal systemic examination (eg growth failure)
- Abnormal chest x-ray
- Abnormal lung function
- Co-existing chronic disease (eg immunodeficiency, syndromes)
Management
Investigations and treatment are rarely needed in otherwise well children who have a short history (
<4 weeks) of non-specific cough
- Over the counter cough medicines and decongestants are not recommended due to lack of proven efficacy and potential safety risks
- Empiric use of antibiotics, steroids, proton pump inhibitors and antihistamines are not recommended
- Honey is often proposed as a treatment for cough, but there is no strong evidence supporting its effectiveness, and it carries risks such as infant botulism (in infants
<12 months), dental caries and aspiration
All children presenting with cough should have
- education around avoidance of airway irritants eg cigarette smoking, vaping, e-cigarettes and wood-fire heaters
- understanding of when to seek repeat assessment (transition to chronic cough)
- acknowledgement of parental concerns and reassurance
Further assessment (including investigations and/or treatment) is required for:
| Cause of chronic cough |
Management |
|
Protracted bacterial bronchitis (PBB)
Most common cause of chronic wet cough in children. Children are otherwise well, with no alternative cause evident on history or examination and investigations (including chest x-ray, apart from perihilar thickening) are normal
|
Extended course of antibiotics. Start with 2-week course of
- Amoxicillin/clavulanic acid 22.5 mg/kg of amoxicillin component (max dose 875 mg) bd
- Penicillin hypersensitivity: trimethoprim/sulfamethoxazole 4 mg/kg of trimethoprim component (max dose 160 mg) bd
If wet cough persists after 2 weeks, continue same antibiotic for a further 2 weeks
If wet cough persists after 4 weeks or child has had >3 PBB episodes/year, consider further investigations (as per suppurative lung disease) and referral to paediatrician and/or paediatric respiratory physician
|
|
Chronic suppurative lung disease, bronchiectasis
Chronic wet cough, which is unresponsive to PBB treatment, or frequently recurs when antibiotics ceased. Can also have recurrent pneumonia, abnormal chest x-ray, and suggestive examination findings (clubbing, growth failure, chest
wall deformity)
|
FBE, serum immunoglobulins (IgM, A, G), chest x-ray, spirometry (if able), sweat test, sputum culture
Refer to paediatric respiratory physician for further assessment (including consideration of CT chest, bronchoscopy and bronchoalveolar lavage)
Specific treatment depends on underlying cause
|
|
Interstitial lung disease
Chronic (typically) dry cough. Diffuse inspiratory crepitations, tachypnoea, growth failure, hypoxia
|
Specific treatment depends on underlying cause
Referral to paediatric respiratory physician for further assessment
|
|
Somatic cough or tic disorder
Often honking, disappears when asleep or distracted. Repetitive throat clearing
|
Education and reassurance
Consider referral for distraction therapies, psychological support, hypnosis
|
| Asthma |
See Asthma |
| Retained inhaled foreign body |
See Foreign body |
| Pertussis |
See Pertussis |
| Sinusitis |
See Sinusitis |
Consider consultation with local paediatric team when
Chronic cough requiring further assessment and management
Findings suggestive of an underlying condition associated with chronic cough
Consider referral to paediatric respiratory physician when
- Chronic wet cough and failure to respond to 4 weeks of appropriate antibiotics
- Recurrent episodes of chronic wet cough (>3 episodes of PBB/year)
- Chronic dry cough persisting >6 months and failure to respond to appropriate treatment (eg empiric trial of asthma treatment)
- Assessment is suggestive of specific cough, or red flags are present
Consider transfer when
Children requiring care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Child is stable
- Investigations and follow up arranged if needed
Additional resources
Sound of wet cough (audio file)
History Taking as a Diagnostic Tool in Children With Chronic Cough (Frontiers in Pediatrics publication)
Chronic cough resources (Lung Foundation Australia)
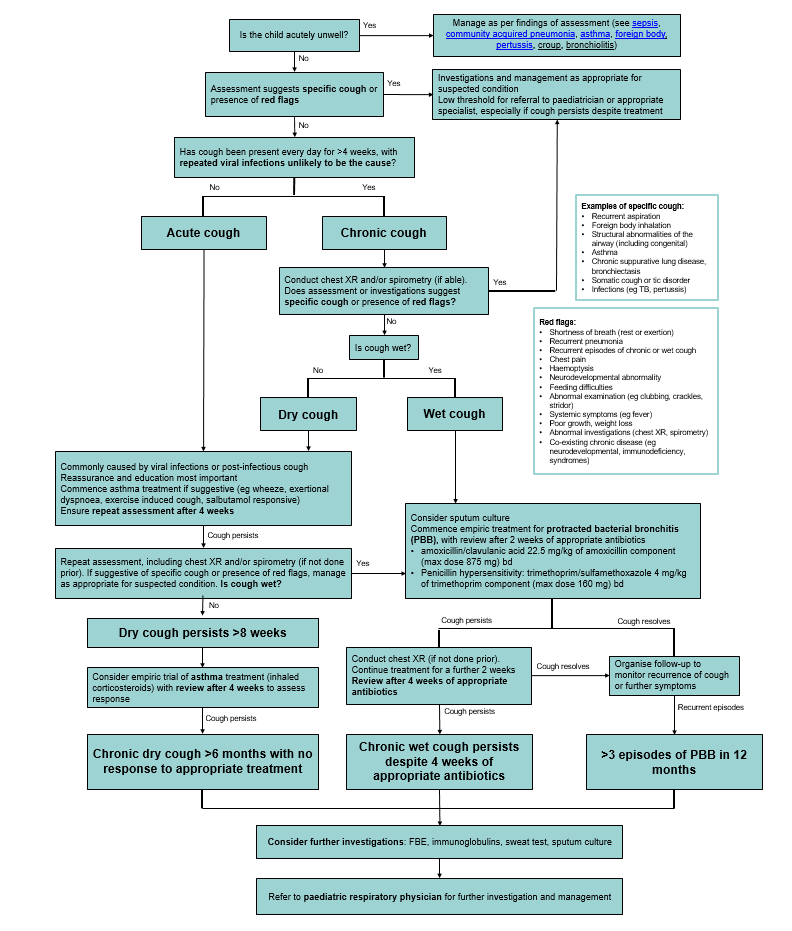
Diagnosis and assessment of chronic cough in children - clinical algorithm (Lung Foundation Australia)
Parent information
Cough (RCH Patient Handout)
Protracted Bacterial Bronchitis (PBB) in Children (American Thoracic Society)
Chronic cough in children (Lung Foundation Australia)
Interactive lung health education tool for Indigenous children/families (Menzies)
* Last updated March 2025
Reference List
- Brodie, M. Childhood cough. BMJ. 2012. 344 (e1177). Retrieved from https://doi.org/10.1136/bmj.e1177
- Chang, A et al. Management of children with chronic wet cough and protracted bacterial bronchitis: CHEST guideline and expert panel report. CHEST. 2017. 151 (4), p884-890. Retrieved from https://journal.chestnet.org/article/S0012-3692(17)30075-2/fulltext
- Chang, A et al. Managing chronic cough as a symptom in children and management algorithms: CHEST guideline and expert panel report. CHEST. 2020. 158 (1), p303-329. Retrieved from https://journal.chestnet.org/article/S0012-3692(20)30325-1/fulltext
- Gill, P. Treatments for cough and common cold in children. BMJ. 2024. 384 (e075306). Retrieved from https://www.bmj.com/content/384/bmj-2023-075306
- Kasai, A et al. Cough. Pediatrics in Review. 2019. 40 (4), p157-167. Retrieved from https://pedsinreview.aappublications.org/content/40/4/157
- Kuitunen, I et al. Honey for acute cough in children -- a systematic review. Eur J Pediatr. 2023. 182 (9). Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10570220/
- Marchant, J et al. Cough in Children and Adults: Diagnosis, Assessment and Management (CICADA) Australian Chronic Cough Position Statement Update. Lung Foundation Australia. 2022. Retrieved from https://lungfoundation.com.au/wp-content/uploads/2023/05/CICADA_FULL_Position_statement_updated.pdf