See also
Gastrooesophageal reflux in infants
Afebrile seizures
Bronchiolitis
Key Points
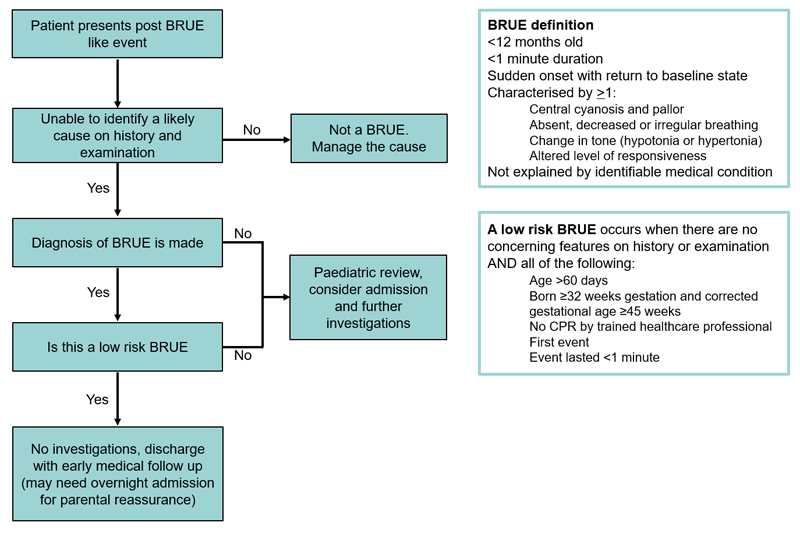
- A BRUE (Brief Resolved Unexplained Event) is an event in an infant that is characterised by a marked change in breathing, tone, colour or level of responsiveness, followed by a complete return to a baseline state, and that cannot be explained by a medical cause
- A BRUE is a diagnosis of exclusion. There are many diagnosable conditions that cause symptoms similar to that of a BRUE
- Infants who have had a BRUE can be stratified into groups of low and high risk of having a repeat event or a serious underlying disorder
- A low risk BRUE may be safely managed in an outpatient setting
Background
The term Apparent Life Threatening Event (ALTE) has been replaced by BRUE
A BRUE refers to an episode in an infant less than 12 months old which is:
- Duration <1 minute (typically 20-30 seconds)
- Sudden onset, accompanied by a return to a baseline state
- Characterised by ≥1 of the following:
- cyanosis or pallor
- absent, decreased or irregular breathing
- marked change in tone (hypertonia or hypotonia)
- altered level of responsiveness
- Not explained by identifiable medical conditions
Assessment
The assessment of the event should be directed at determining if there is a cause for the event and to assess for risk factors for recurrence. The differential diagnoses of these events are broad
Differential diagnoses
- Airway: obstruction, inhaled foreign body, laryngospasm, congenital abnormalities, infection
- Cardiac: congenital heart disease, vascular ring, arrhythmias, prolonged QT
- Abdominal: intussusception, strangulated hernia, testicular torsion
- Infection: pertussis, sepsis, pneumonia, meningitis
- Metabolic: hypoglycaemia, hypocalcaemia, hypokalaemia, other inborn errors of metabolism
- Toxins/Drugs/Ingestions: accidental or non-accidental
- Inflicted injury
History
History should be taken, ideally first-hand, from someone who observed the infant during or immediately after the event. Key features of history should include:
Description of event
- Choking, gagging
- Breathing: struggling to breathe, pause, apnoea
- Colour and colour distribution: normal, cyanosis, pallor, plethora
- Distress
- Conscious state: responsive to voice, touch, or visual stimulus
- Tone: stiff, floppy, or normal
- Movement (including eyes): purposeful, repetitive
Circumstances and environment prior to event
- Awake or asleep
- Relationship of the event to feeding and history of vomiting
- Position (prone/supine/side)
- Environment: sleeping arrangement, co-sleeping, temperature, bedding
- Objects nearby that could be swallowed, cause choking or suffocation
- Illness in preceding days
End of event
- Duration of event
- Circumstances of cessation: self-resolved, repositioned, stimulation, mouth to mouth and/or chest compressions
- Recovery phase: rapid or gradual
Other history
- Past medical history including previous similar events
- Preceding/intercurrent illness
- Sick contacts
- Family history of sudden death or significant childhood illness
- Patient medications, medications or other drugs within the home
- Social history – parental supports, psychosocial assessment
Examination
A detailed general physical examination is required, bearing in mind the differential diagnoses
Risk Stratification
It is common for no specific diagnosis to be made after evaluation and a period of observation. The most common cause of these events is thought to be exaggerated airway reflexes in the setting of feeding, reflux, or increased upper airway secretions
If the infant has fully recovered, has benign examination findings and the event meets the criteria for a BRUE, the event can be risk stratified
A low risk BRUE occurs when there are no concerning features on history or examination AND all of the following:
- age >60 days
- born ≥32 weeks gestation and corrected gestational age ≥45 weeks
- no CPR by trained healthcare professional
- first event
- event lasted <1 minute
A low risk BRUE is unlikely to represent a presentation of a severe underlying disorder and is unlikely to recur
Management
Investigations
A low risk BRUE does not require any investigations
For similar events that fall outside the low risk BRUE criteria, consider performing the following investigations
- ECG (measure QT interval)
- Nasopharyngeal sample for viruses and pertussis
- Blood glucose
- FBE and UEC if clinically indicated
Treatment
If the infant requires ongoing acute treatment, the event is not considered to be a BRUE
It should be acknowledged with the family that these events are highly anxiety provoking and parents often feel that their child has nearly died
Infants who have had a low risk BRUE may be discharged safely if their parents feel reassured and capable of caring for their infant at home
If discharged, it is recommended that these infants have early medical follow up. In practice, many infants with a low risk BRUE are admitted to hospital for observation for parental reassurance
Infants with a high-risk BRUE may still have a benign cause for their symptoms but should be admitted for observation, pulse oximetry (or cardiac telemetry if clinical suspicion of arrhythmia) and paediatric review
Consider consultation with local paediatric team when
The event does not meet low risk BRUE criteria
Consider transfer when
There is a concern of a serious underlying disorder
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services.
Consider discharge when
There is low clinical suspicion of a serious underlying disorder and the parents are reassured
Parent information
BRUE Parent Handout (American Association of Paediatrics)
Last updated July 2020