See also
Acute asthma
Asthma in adolescents (12 years and over)
Preschool asthma (1-5 years)
Key points
- This guideline provides advice for assessment and ongoing management of primary school aged children with asthma. See Acute asthma for acute management
- Treatment with short-acting beta agonist (SABA) alone should only be used for children who have mild and infrequent symptoms with no risk factors
- First-line preventer treatment for most school-age children is low dose inhaled corticosteroid (ICS)
- Treatment should be stepped up and down according to response. Consider ceasing preventer treatment following a 6 month symptom-free period
- Additional management includes regular asthma education, reviewing inhaler technique, assessment of contributing factors and annual influenza vaccine
Background
Asthma medications and delivery devices include:
- Inhaled corticosteroid (ICS)
- Short-acting β-agonist (SABA)
- Long-acting β-agonist (LABA)
- Metered dose inhaler (MDI)
- Dry powder inhaler (DPI)
Frequent use of SABA alone (>3 MDI canisters per year) and infrequent use of preventer/anti-inflammatory is associated with more severe asthma exacerbation and death
ICS-formoterol MART (ICS-formoterol maintenance and reliever therapy or “SMART”) is worth considering in children nearing 12 years who have poor adherence with preventers or high SABA use. See
Asthma in adolescents (12 years and over)
MDI have a large carbon footprint. The best way to decrease the impact is to achieve good asthma control to reduce need for SABA and/or switch to DPI when possible. Many children can generate adequate inspiratory pressure to use a DPI (from about age 6). Other measures include:
- prescribing 1 puff of a stronger dose preventer instead of 2 puffs of a weaker dose, particularly if dose is stable and unlikely to be reduced in the short term (also reduces cost)
- using once daily medication (eg ciclesonide)
- dose tracking
- See Additional resources below for more information on green prescribing
Assessment
History
Diagnosis is based on symptoms (wheeze, breathlessness, cough) and treatment response (ie recurrent clusters of symptoms that respond to SABA or chronic symptoms that respond to ICS) in the absence of red flags
Red flags for alternative diagnoses:
- productive cough
- isolated cough
- paraesthesia
- chest pain
- clubbing
Risk of exacerbation
- History of intubation or intensive care unit (ICU) admission for asthma
- 2 or more presentations to hospital that require treatment for asthma
- Using SABA more than twice weekly or >3 MDI canisters per year
- Infrequent use/poor adherence of preventer/anti-inflammatory
- Incorrect inhaler technique
- Exposure to smoke/vaping
- Other comorbidities eg obesity, sleep apnoea, chronic rhinosinusitis, confirmed food allergy
Assessment of asthma control
Good asthma control is defined as:
- Daytime symptoms less than two times per week
- Need for reliever/SABA less than two times per week
- No limitation of activities
- Nighttime waking due to asthma less than two times per month
- No need for systemic corticosteroid, ED presentation or admission
Consider contributing factors:
- Allergic rhinitis
- Obesity
- Obstructive sleep apnoea
- Gastro-oesophageal reflux
- Dysfunctional breathing (including vocal cord dysfunction)
- Depression/anxiety (may present as chest tightness without wheeze)
- Smoking and vaping (passive or active)
- Damp, mouldy, cold or crowded housing
- Aeroallergens,
thunderstorm asthma
- Barriers to accessing healthcare
Examination
- Review inhaler technique
- Look for signs of comorbidity, including allergic rhinitis and eczema
- Measure height and weight
- Respiratory examination
Management
Investigations
No investigations are required unless considering an alternative diagnosis
- Spirometry may have a role in children in whom the diagnosis or severity is uncertain
- Allergy testing (RAST/skin prick testing) should not be performed if there is no history of an immediate reaction to the potential allergen
- A clear relationship between an allergen and asthma symptoms also does not require testing, rather this should be treated as an allergic trigger and avoided where possible
Treatment
Education
- Assess knowledge and understanding and address gaps on
- symptom recognition and management
- when to seek medical attention
- emergency management
- role of reliever and preventer treatment
- inhaler technique
- Recommend annual influenza vaccine
- Check adherence at every visit and address barriers
- Asthma Action Plan: all children should have a written action plan for at home and childcare
Reliever treatment
SABA (salbutamol): all children should be prescribed SABA with spacer, and encouraged to have inhaler and spacer with them at all times
Dose: salbutamol 100 microg MDI, 6 - 12 puffs (via spacer +/- mask)
- Check number of canisters used between each review (>3 a year is high risk)
- Encourage dose-tracking (eg check dose counter if available) to ensure canisters aren’t prematurely discarded (environmental hazard) nor used once empty
Step 1: SABA only
- Can use SABA only, without regular preventer, in children who have
- not required treatment for exacerbations (systemic corticosteroid or hospital presentation) in the past 12 months
- symptoms occur infrequently (see table below)
- no other contributing factors (smoking in household, obesity, social risk factors etc)
- Most other children require maintenance treatment (preventer)
Maintenance treatment (preventers)
Step 2: Low dose ICS via spacer (and reliever as needed)
- Ciclesonide 80 microg once daily or Fluticasone 50 microg twice daily
- ciclesonide has the advantages of daily dosing, lower side effect profile, PBS subsidised so lower out of pocket costs (NB not all spacer devices are compatible)
Montelukast oral tablet
- Montelukast can be used as an alternative first line preventer (or adjunct to ICS) in children requiring further control
- Montelukast 5 mg once daily
- consider using as ICS alternative if significant parental concern regarding steroids or in children where use of MDI + spacer is particularly difficult
- 1 in 6 children may develop side effects with this medication including agitation, sleep disturbance and altered mood. If this occurs, cease medication to see if symptoms resolve
Step 3: Moderate dose ICS OR low dose ICS + montelukast OR ICS/LABA (and reliever as needed)
- Moderate dose ICS = fluticasone 100 microg twice daily or ciclesonide 160 microg once daily
- ICS/LABA = budesonide/formoterol MDI 100 microg/3 microg, 2 puffs twice daily or DPI 200 microg/6 microg, one inhalation twice daily
Step 4: moderate dose ICS + montelukast OR ICS/LABA + montelukast OR consider referring for expert advice. See Approach to asthma not responding to treatment below
Step approach in maintenance treatment
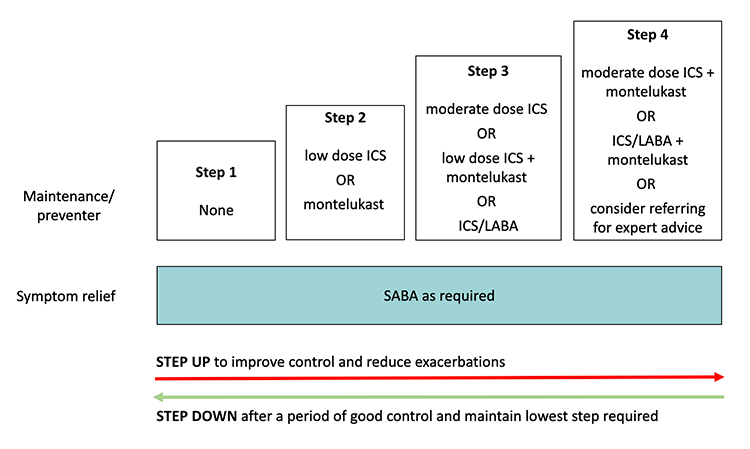
Adapted from Australian Asthma Handbook, GINA and McNamara
Stepping up or down according to response
The degree of symptom control, irrespective of the current regimen, informs whether changes need to be made to the preventer treatment
|
|
Good control
(All of) |
Partial control
(One or two of) |
Poor control
(Three or more of) |
|
Daytime symptoms |
≤2 days per week |
>2 days per week |
>2 days per week |
|
Need for reliever* |
≤2 days per week |
>2 days per week |
>2 days per week |
|
Limitation to activity |
none |
present |
present |
|
Nighttime symptoms (or on waking) |
none |
present |
present |
* Reliever frequency does not include doses taken prophylactically before exercise
- Start at Step 1 and step up after 6 weeks if further control required
- Always check correct technique and adherence prior to stepping up. Consider alternate diagnoses
- Good control for a period of approximately 3 months suggest preventer treatment could be stepped down
- Continue the lowest treatment that controls symptoms
- Only cease treatment after a period of 6 months symptom-free and review 4-6 weeks after stepping down
- Consider ongoing management of triggers and seasonal factors when stepping treatment up or down
Approach to asthma not responding to treatment
- Review if asthma is correct diagnosis
- Review adherence
- Review
inhaler technique
- Consider contributing factors (see above in assessment)
For children who are nearing adolescence (ie 10-11 years old) and having difficulty with their asthma control, it is worth considering ICS-formoterol MART. See
Asthma in adolescents (12 years and over)
- This can be prescribed as either budesonide/formoterol DPI (Turbuhaler®) 200 microg/6 microg or budesonide/formoterol MDI (Rapihaler®) 100 microg/3 microg
- DPI is preferred for those with adequate technique
- This may be prescribed “off label” or via private script
Management of acute exacerbations in the community
- See
Acute asthma
- In children already taking daily ICS, there is no role for increasing the dose of ICS during an exacerbation
Consider consultation with local paediatric team / respiratory or specialist asthma service when
- Inadequate asthma control achieved at Step 4
- Diagnosis of asthma uncertain
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Parent information
RCH Kids Health Info: Asthma videos
Additional resources
Asthma Action Plan
National Asthma Council Symbicort (SMART) Action Plans
Asthma Handbook: Resources
Asthma Handbook: Action plans
Asthma action plan library
Green prescribing
Breathe Green Project
Allergic rhinitis management/referral guidelines
Referral guideline: Allergic rhinoconjunctivities (hay fever)
Last updated June 2023