See also
Urinary tract infection
Recognition of the seriously unwell neonate and young infant
Key points
- Dilation of the fetal renal collecting system is often benign, but may be caused by serious underlying pathology
- The goal of assessment is to identify babies with significant renal or urinary tract abnormalities, while limiting unnecessary radiographic studies
- A child with moderate to severe dilation (anterior posterior renal pelvic diameter >10 mm) requires further investigation and early referral to avert long-term complications
Background
- Antenatal urinary tract dilation (UTD) is a common abnormality detected on prenatal ultrasound, reported in up to 5% of pregnancies
- The term UTD encompasses any dilation of the kidney, renal pelvis, ureter and/or bladder, replacing ambiguous terms such as hydronephrosis and pyelectasis
- UTD encompasses a wide spectrum of conditions, ranging from transient and benign dilation of the renal pelvis to significant congenital anomalies of the kidney and urinary tract
- The severity of UTD is determined by anterior-posterior renal pelvic diameter (APD or APRD) and/or degree of calyceal dilation via ultrasound
- Urinary tract obstruction and vesicoureteric reflux (VUR) are important causes that may result in severe and chronic renal impairment. Early diagnosis and management may dramatically improve long-term outcomes
Assessment
The finding of UTD on antenatal ultrasound should prompt the clinician to look for the following on history and examination
Antenatal findings
- Degree of UTD (refer to table below)
- Presence of calyceal dilation, ureteric dilation, cortical thinning, reduced corticomedullary differentiation or abnormal bladder
- Unexplained oligohydramnios (do not attribute oligohydramnios to premature rupture of membranes where there is significant, and especially bilateral, urinary tract dilation)
- Single kidney or other renal tract abnormalities
Postnatal findings
- Poor urinary stream (note: a normal urinary stream does not exclude bladder outlet obstruction)
- Has not passed urine within first 24 hours of life
- Palpable bladder
- Palpable kidney
- Urinary tract infection (Children with UTI in the absence of urinary tract dilation on antenatal ultrasound, see
Urinary tract infection)
Assessment of severity
Degree of UTD |
Anterior Posterior Diameter (APD) of the renal pelvis
measured at the maximum diameter of the intrarenal pelvis |
|
Second Trimester
16-28/40 |
Third Trimester
≥28/40 |
Postnatal |
|
Normal |
<5 mm |
<7 mm |
<5 mm |
|
Mild |
5.1 – 7 mm |
7.1 – 10 mm |
5.1 – 10 mm
|
|
Moderate |
7.1 – 10 mm |
10.1 – 15 mm |
10.1 – 15 mm
|
|
Severe |
>10 mm |
>15 mm |
>15 mm |
Note: Antenatal or early postnatal calyceal dilation or other abnormal findings, with or without UTD, would increase the level of concern
Management
Management of an infant with UTD diagnosed antenatally
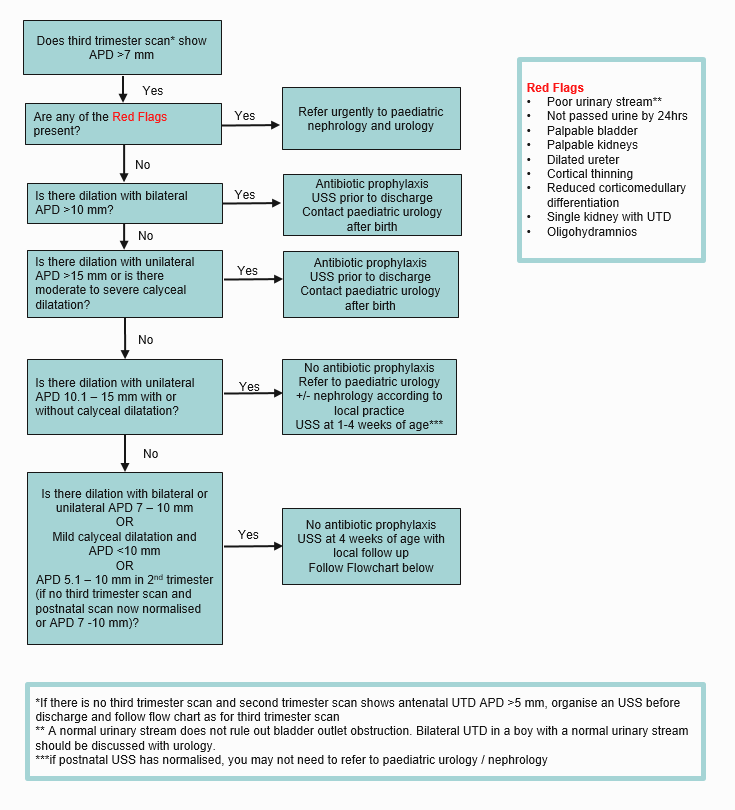
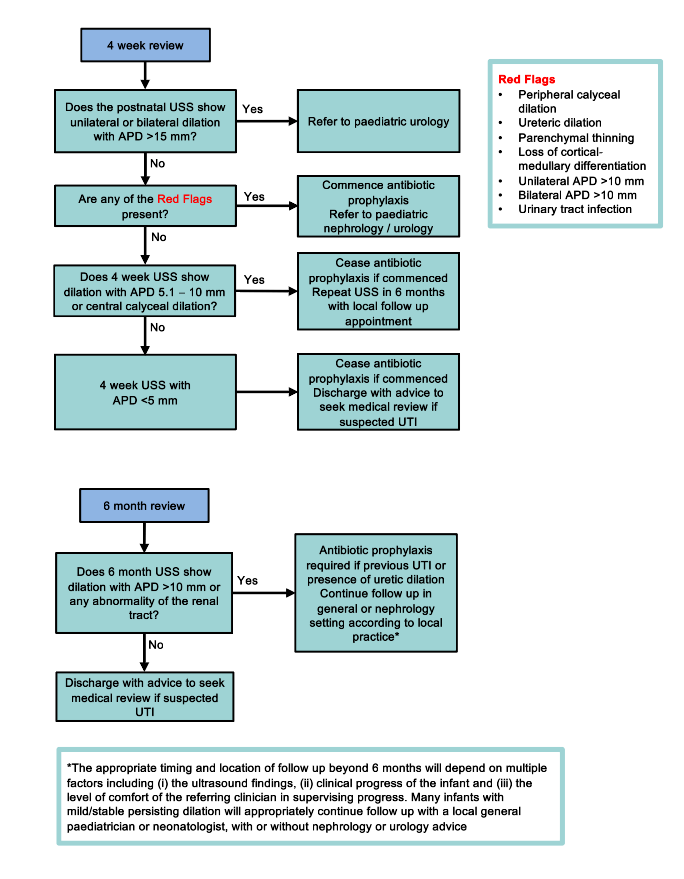
Management at 4 weeks of infant with UTD diagnosed antenatally
Investigations
Timing of postnatal ultrasound
- Indications for an early renal USS (
<48 hours):
- Presence of red flags (to rule out urological emergencies)
- UTD on second trimester scan without repeat scan in third trimester
- An ultrasound performed before the infant is one week of life may not reflect the true extent of urinary tract dilation as neonatal urine output is still increasing
- If normal, a repeat ultrasound should be done at 4-6 weeks to confirm the absence of urinary tract dilation
Other investigations
Other investigations, eg MAG3 scan, are not routinely required. Discuss with senior paediatrician or paediatric nephrologist/urologist
Treatment
Prophylactic antibiotics for UTI prevention may be indicated:
- Trimethoprim – 2 mg/kg once daily
Parent education
Discuss and provide written information to parents on symptoms of urinary tract infection in neonates
Symptoms including fever, vomiting, decreased urine output and irritability suggest the need for
UTI screening
Consider consultation with local paediatric team when
Any pregnancy where there is antenatal UTD or where there is an infant with UTD should be linked with the local paediatric team
Discuss with paediatric nephrology/urology:
- Poor urinary stream
- Palpable bladder
- Palpable kidney
- Dilated ureter
- Cortical thinning
- Abnormal corticomedullary differentiation
- Solitary kidney with urinary tract dilation
- Oligohydramnios with urinary tract dilation (regardless of the cause)
Consider transfer when
Child requiring care beyond the comfort of the local health care facility
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- Diagnosis clear
- Management instituted
- Follow up organised
Parent information
See
parent resources
Last updated December 2021