Causes of AOM are often multifactorial. Exposure to cigarette smoke from household contacts is a known modifiable risk factor
- Systemically unwell
- Ear examination:
- signs of acute inflammation of the tympanic membrane (TM): bulging, red, opaque TM
- a red TM alone is not AOM. The most common cause is a viral upper respiratory tract infection (URTI)
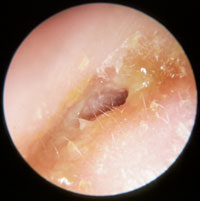
Otoscopic images of tympanic membranes (TM):
|
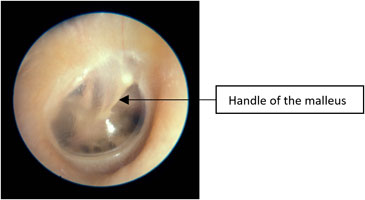 |
Normal tympanic membrane
- TM is translucent
- The handle of the malleus is vertical
- No erythema
|
|

|
Injected tympanic membrane
- Pink/red TM
- Often seen with fever, eustachian tube obstruction or viral URTI
- TM is transparent (there is no middle ear effusion)
- The handle of the malleus is well seen and is more horizontal
|
|

|
Bulging and red tympanic membrane in AOM
- Loss of the TM landmarks, especially the handle of the malleus
- TM is opaque, may be red from inflammation or white from pus in the middle ear
|
.jpg)
|
Otitis media with effusion (OME) “glue ear”
- TM is retracted with prominence of the handle of the malleus, which is also drawn in/more horizontal
- TM may be bulging or have an air-fluid level behind the TM
- Yellow/amber appearance is consistent with fluid
- Light reflex on otoscopic examination
|
|
.jpg)
|
Perforated tympanic membrane with otorrhoea
|
|
|
Otitis externa
- Ear is tender to examine
- Skin of the external ear canal is swollen and there can be thin pus
|
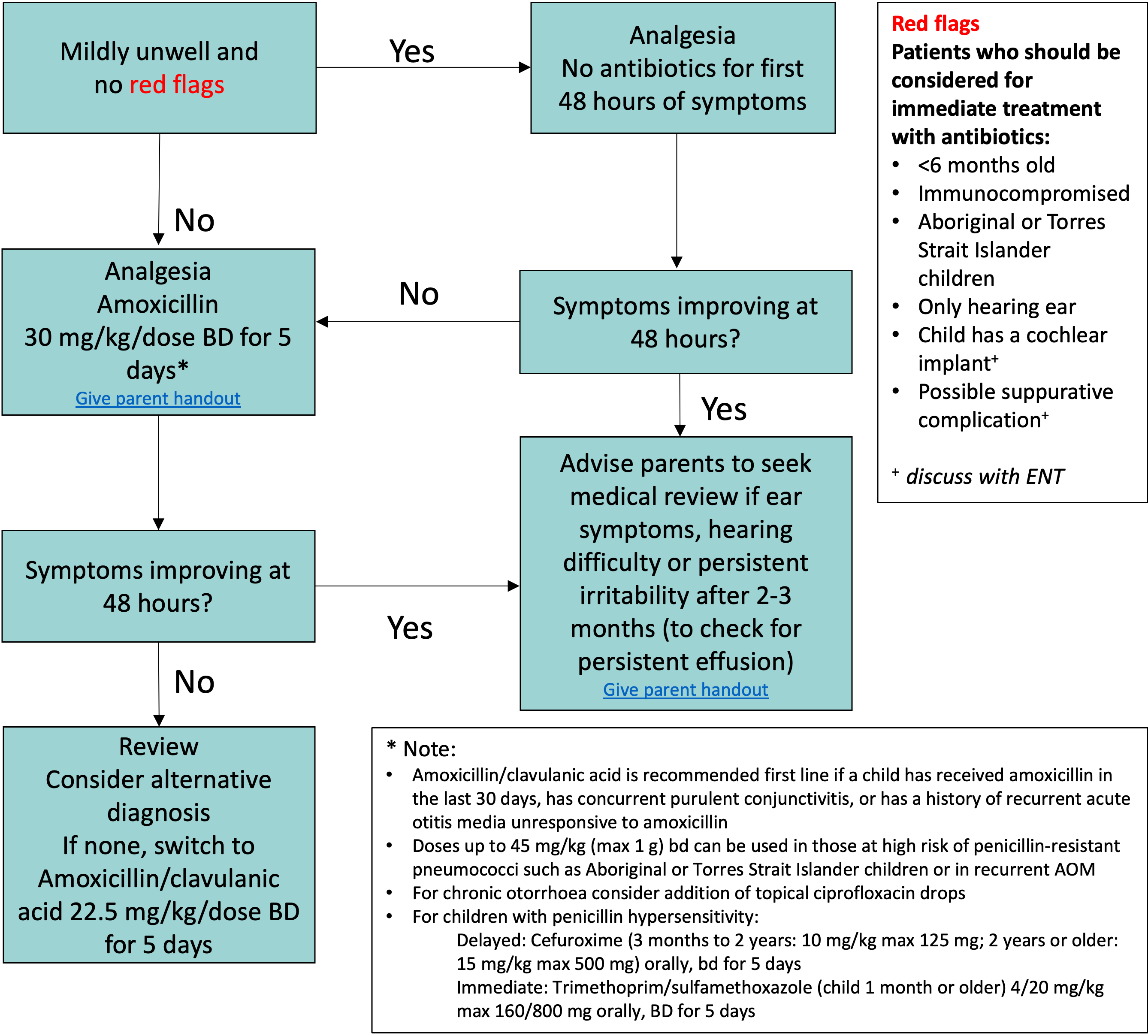
Management
In Infants, especially
<6 months old, the diagnosis of AOM and OME can be inaccurate. Other diagnoses should be fully considered (see Febrile child)
Management may also differ for children from higher
risk groups, such as those living in Aboriginal or Torres Strait Islander
communities (see additional resources below)
Investigations
- There is no role for routine diagnostic investigation for AOM
- Diagnostic imaging such as CT and MRI is usually only required in children with suspected intracranial complications
Treatment
- Most cases of AOM in children resolve spontaneously and antibiotics are not recommended
- Treat pain with adequate and regular simple analgesia. See
Acute pain management
- As an adjunct, short-term use of topical analgesia eg 2% lignocaine (for injection), 1-2 drops or Benzocaine + Phenazone (Auralgan®) applied to an intact tympanic membrane, may be effective for severe acute ear pain
- Decongestants, antihistamines and corticosteroids are not effective in AOM
- Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns; please refer to local guidelines
Complications
Tympanic membrane perforation
- AOM with TM perforation is common and results in otorrhoea and frequently, relief of pain
- Otorrhoea due to TM perforation should be distinguished from Otitis Externa
Acute mastoiditis (AM)
Acute mastoiditis, although rare, is the most common suppurative complication of AOM and may be associated with intracranial complications
- The diagnosis of AM is based on post auricular inflammatory signs (erythema, oedema, tenderness or fluctuance), a protruding auricle often with external auditory canal oedema and signs of AOM (see image below)
- Requires prompt treatment with appropriate
intravenous antibiotics (eg 3rd generation cephalosporin)
- Consult ENT as may require surgical treatment

Acute mastoiditis
Other complications
- Other suppurative complications including intracranial spread of infection are rare
- Facial nerve palsy secondary to AOM should be discussed with ENT
- Long-term non suppurative complications include atelectasis of the TM and cholesteatoma
Otitis media with effusion (OME)
- OME, previously termed serous otitis or glue ear, is fluid in the middle ear without signs and symptoms of infection, other than transient hearing impairment
- The presence of a middle ear effusion is not a diagnostic sign of AOM (an effusion may not resolve for up to 12 weeks following AOM)
- Antibiotics and ENT referral are not routinely required for OME, as the majority of cases occur after an episode of AOM and resolve spontaneously with no long-term effects on language, literacy or cognitive development
- Persistent effusion beyond 3 months should trigger a hearing assessment and ENT involvement/referral
Consider consultation with local paediatric team when
- Children who are systemically unwell
- Neonates
- Children with signs of acute mastoiditis or who have a cochlear implant should be discussed with ENT
Consider transfer when
Children requiring care beyond the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
No signs of complications
Additional resources
Otitis media guidelines for Aboriginal and Torres Strait Islander children
Parent information
Ear Infections and Glue Ear
Last Updated June 2021