Goals of care can be viewed on a continuum. At one end is the prolongation of life, at the other comfort is the only concern. In between lies a zone where patients and families try to find a balance between prolonging life and optimising comfort.
The natural tendency in the face of an ill child is to want to save the child's life. Modern medicine has seemingly limitless options for different treatments but none are perfect. They come with side effects, have indeterminate outcomes and can increase suffering. For each of us there is a tipping point at which
the benefits of treatment are insufficient to outweigh the burdens we are willing to tolerate. This point is different for all of us, and it's particularly difficult deciding where this point is for a child.
This ambiguity can lead to tension between the treating team and the family, and even between members of the treating team. Having agreement on the goals of care is crucial to minimising conflict and distress for all involved. The goals can be quite nuanced, for example the primary goal may be to prioritise comfort, but some efforts to prolong life, such as antibiotics, could be considered tolerable.
The shared understanding of the goals of care between the family and treating team can guide future interventions and ease decision making by focusing everyone's efforts on a common purpose.
For example, cardiopulmonary resuscitation would be appropriate if the agreed goal was to prolong life (and the intervention was likely to achieve that goal), but not where the primary goal was to optimise comfort.
Some interventions (for example, mechanical ventilation) sustain life but come with burdens that may outweigh the benefits for a child who is approaching the end of their life. In this situation consideration needs to be given as to whether the intervention aligns with the goals of care.
It is accepted ethically and legally that life-sustaining treatments can be withheld or withdrawn if they do not provide a net benefit to the child (Larcher 2015; Canadian Paediatric Society 2008; American Academy of Pediatrics Committee on Bioethics 1994; Royal Australasian College of Physicians; British Medical Association 2007). This does not constitute euthanasia.
To withdraw an intervention is to cease treatment that has already been commenced. To withhold an intervention is to not start the treatment in the first place. In its recently published framework for practice in this area, the Royal College of Paediatrics and Child Health outlines circumstances in which it would be
ethically permissible to withhold or withdraw life-sustaining treatment (Figure 1, page 14) (Larcher et al. 2015). The College is careful to say, however, that it is not obligatory to withhold or withdraw treatment under these circumstances.
It is generally accepted that no ethical or legal distinction can be made between withdrawing and withholding life-sustaining treatment. This is important, as it means there is no legal or ethical obligation to continue an intervention just because it has been started.
It is acknowledged however, that withdrawal of treatment may be more emotionally and psychologically challenging for parents and health professionals than withholding treatment (Larcher et al. 2015; American Academy of Pediatrics Committee on Bioethics 1994; British Medical Association 2007).
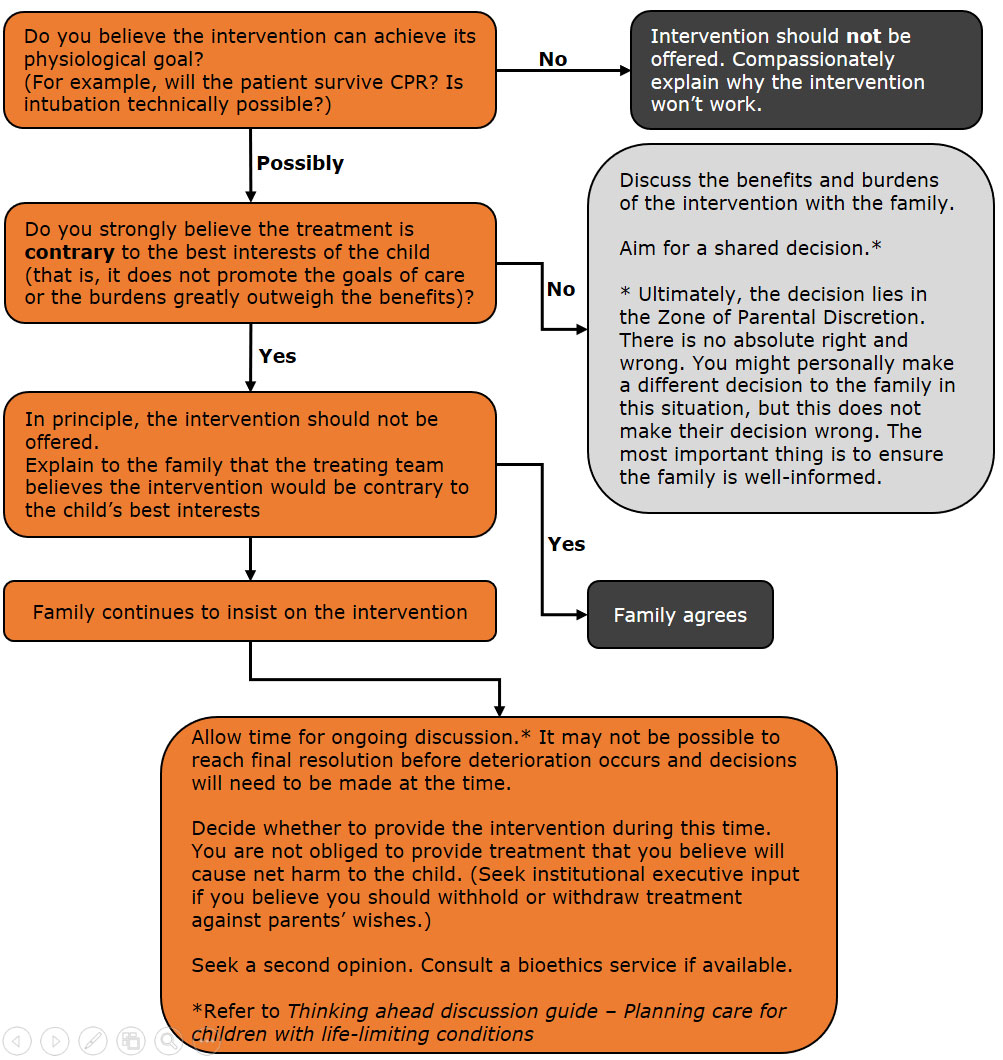
Figure 1: Circumstances under which life-sustaining treatment could be withheld
or withdrawn.
When life is limited in quantity
This includes conditions in which treatment is unable or unlikely to prolong life significantly, or reflect the values of the child and family. These comprise:
- brain stem death, as determined by agreed professional criteria appropriately applied
- imminent death, where physiological deterioration is occurring irrespective of treatment
- inevitable death, where death is not immediately imminent but will follow and where prolongation of life by life-sustaining treatment confers no overall benefit.
When life is limited in quality
This includes situations where treatment may be able to prolong life significantly but will not alleviate the burdens associated with illness or treatment itself. These comprise:
- where the treatments themselves produce sufficient pain and suffering so as to outweigh any potential or actual benefits
- where the severity and impact of the child's underlying condition is in itself sufficient to produce such pain and distress as to overcome any potential or actual benefits in sustaining life
- where the severity of the child's condition is such that it is difficult or impossible for them to derive benefit from continued life.
Informed
competent refusal of treatment
An older child may be assessed as having capacity to competently consent to the withdrawal or withholding of life-sustaining treatment.
In these circumstances, and where the child is supported by his or her parents and by the clinical team, there is no ethical obligation to provide life-sustaining treatment.
A decision that is shared between the treating team, the parents and, where appropriate, the child is the ideal. All have an important contribution to make.
The child
Many children with life-limiting conditions are too young, too disabled or too unwell to communicate, and they depend on their parents and doctors to make decisions on their behalf. There are however, some children who are able to contribute to the decision-making process.
Adolescents and even much younger children may have strong preferences about their care (Weiner et al. 2012; Lyon et al. 2009; Hinds et al. 2005). They know better than anyone what it is like for them to be unwell. They will certainly have something to say about what they enjoy, what
they find difficult or frightening, what goals they have and what they are hoping for.
Their views can be extremely helpful in guiding parents and doctors in advance care planning, and they can be discussed even if the child does not know or understand their prognosis.
More mature children may undertake a greater role in advance care planning, but it is not possible to specify an age at which this should occur. The degree to which a child participates will depend on the individual child.
The United Nations Convention on the Rights of the Child places great emphasis on the child's views. Similarly, The Royal College of Paediatrics and Child Health (UK) believes 'there should be a presumption that children will be involved in decisions about treatment (including
those concerned with limitation of life-sustaining treatment) wherever possible and at a level that reflects their ability, understanding and experience'.
The College outlines four ways in which health professionals can involve children:
- by providing information
- by listening and responding to their concerns
- by using techniques such as play therapy to increase the child's understanding and ability to express their views
- by using the child's views to inform actions.
From an ethical standpoint, older children may demonstrate decision-making ability by showing they understand the nature of their condition, its treatment and the consequences of their decisions. In this case, they should, if they wish, contribute significantly to decisions regarding their medical treatment.
The High Court of Australia has recognised that a young person may provide informed consent to treatment if he or she has achieved 'a sufficient understanding and maturity to fully understand what is proposed'.1
The parents
Parents or a child's legal guardians2 bring a crucial perspective to decision making regarding the health care of their child. They can share the family's values, as well as specific knowledge of the child and which treatments or situations they might
experience as a benefit and a burden.
In thinking about goals of care, many feel torn between promoting survival and avoiding suffering.
'It is a dilemma. Because I don't
want him to suffer, not for one per cent. At the same time, I want to have him
with me for some more time.'
Parent (de Vos et al. 2015)
Parents will vary in the degree to which they wish to be involved and to lead decision making (Sullivan, Monagle and Gillam 2014). Some will seek guidance from or even defer to the treating team. Others feel it is their duty to take a lead role.
Parents bring to the decision making process their own understandings of illness, expected outcomes, trust of western medicine versus desire for alternative therapies, health literacy and religious and cultural beliefs. As a result their views on the best treatment for their child may not be the same as the
views of the treating team.
Ethically, parents are usually recognised as the decision makers for their child, but in some circumstances this role needs to be challenged by the treating team.
This is of particular concern when the parents' decisions will lead to a child enduring significant suffering undergoing treatments that offer no chance of benefit.
The paediatrician
The paediatricians involved in the care of the child are also critical. They bring knowledge of the illness, the prognosis, the available treatments and the likely efficacy of those treatments.
They are able to describe the benefits and burdens of treatment in general terms. Where the paediatrician has come to know the child over time, they also have specific knowledge of the child and their experience of treatment. They may also have had private conversations with the child about goals and values.
In practice
In most cases, decision making is shared between the family and the treating team, each contributing the elements outlined above. The child takes a role in this process to the extent their developmental level, ability and willingness allows.
When there is disagreement, this can usually be resolved through ongoing discussions, however, occasionally parents may insist on an intervention the treating team believes is not in the child's best interests, or request the withdrawal of a treatment the team believes is in the child's best interests.
It is important to first consider whether a decision is actually required. Where there is certainty that the intervention in question will not benefit the child, the treating team should compassionately explain to the family why this treatment will not be provided. In this circumstance, there is no decision for the family
to make (Hayes 2013).
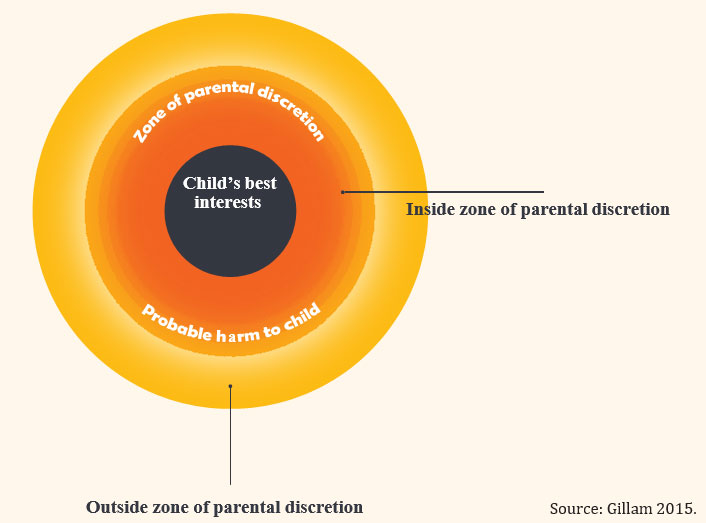
Where there is less certainty, a decision is required and in this situation, the concept of the 'zone of parental discretion' (Gillam 2015) may be useful. In this zone 'lie decisions where [the child's] best interests are uncertain or open to interpretation, as well as
decisions that take into account the interests of siblings, parents and the family as the whole.' (Gillam 2015).
Put another way, there may be a range of different decisions that are reasonable in a given situation: the balance of benefits and burdens will be weighed differently by different individuals even given the same clinical situation. Children and their families will make decisions based on their individual values and experiences.
Health professionals may not always agree with these decisions but they fall within the Zone of Parental Discretion. There may be a point however, beyond which the treating team feels net harm will be done to the child if parents' wishes are followed, for example, because the chance of benefit is so small and the
burdens of treatment so great.
At this point, the parents' decision falls outside the zone of parental discretion, and the treating team should not follow it. A second opinion, clinical ethics consultation or legal opinion may be necessary and institutional executive input should be
sought.
Ultimately, a doctor cannot be compelled by a patient or family to provide treatment that the doctor believes would not serve the child's best interests. The seeking of a second opinion can be helpful in resolving disagreement. If an agreed treatment plan cannot be achieved in an
appropriate timeframe, further discussion and clinical ethics involvement, or legal advice should be sought and it may be appropriate to seek input from the institution's executive team. (Gillam 2015). The decision making process is outlined on Figure 2 (page 18).
Figure 2: Decision-making in practice