Introduction
Regular measurement and documentation of clinical observations (i.e. vital signs and other physiological observations) are essential requirements for patient assessment and the recognition of clinical deterioration.
Parents/ carers have an important role in the detection of clinical deterioration. They know their child best and are well-placed to notice changes in their child’s condition, changes that may be missed by clinicians. Bedside nurses are expected to ask parents/carers about any concerns with each set of observations.
The Victorian Children’s Tool for Observation and Response (ViCTOR) charts are age-specific ‘track and trigger’ paediatric observation charts for use in Victorian hospitals and are designed to assist in recognising and responding to clinical deterioration in children. Thresholds for each physiological parameter
indicate when escalation of care should occur. Initially developed as paper charts, these thresholds have been integrated into the Electronic Medical Record (EMR). The observations are graphically displayed on the ViCTOR graph so that trends can be tracked over time.
These ViCTOR graphs, also known as ‘track and trigger’ charts indicate the response by the clinician once the patient’s observations reach a designated ‘zone’. Concerning changes in any one observation are indicated by two coloured zones (Orange and Red). If a child’s observation transgresses the Orange or Red
zone, an Escalation of Care response should be triggered. The type and urgency of the Escalation of Care response depends on the degree of clinical abnormality.
The ViCTOR graphs are standardised for the following 5 age groups: less than 3 months, 3 to 12 months, 1 to 4 years, 5 to 11 years and 12 to 18 years. At RCH the 12-18 years graph is used for young people older than 18 years.
Aim
To provide guidance to clinical staff regarding the:
- Measurement of clinical observations;
- Use of the Victorian Children’s Tool for Observation and Response; and
- Role of continuous cardio-respiratory monitoring and pulse oximetry monitoring.
Definition of terms (abbreviations and acronyms)
- AUM- Associate Unit Manager
- CPMS – Children’s Pain Management Service
- ECG - Electrocardiograph
- EMR- Electronic Medical Record
- ICP - Intracranial Pressure
- MET - Medical Emergency Team
- NICU - Neonatal Intensive Care Unit
- OneTEAM - is a four-step process where parents/carers can speak up and feel heard when they are concerned about their child’s condition. The process acknowledges that parents/carers and staff are working together, as one team.
- PACU - Post Anaesthetic Care Unit
- PCA - Patient Controlled Analgesia
- PICU - Paediatric Intensive Care Unit
- Rapid Review– priority review of patient by Bed-card doctor within 30 minutes of request.
Guideline details
Clinical Observations
Clinical observations may include;
- estimation of haemoglobin-oxygen saturation (SpO2, pulse oximetry)
- oxygen delivery
- respiratory rate (RR)
- respiratory distress
- heart/pulse rate (HR/PR)
- blood pressure (BP) (systolic, diastolic and mean)
- temperature
- level of consciousness OR level of sedation
- pain score
- in certain clinical circumstances further observations (for example, neurological observations or neurovascular observations)
Parent/Carer Clinical Concern
Parents/Carers should routinely be asked about any clinical concerns with each set of observations. “Do you have any concerns about (insert patient name) at the moment?”
- The question should be asked whilst undertaking observations.
- Asked at a frequency of four hourly, except for the following areas.
| Recovery – Stage 1 |
Once – with last set of observations prior to transfer of patient |
| Recovery – Stage 2 |
Twice –on arrival with first set of observations and with last set of observations prior to discharge/transfer (4/24 for longer stay patients) |
| Banksia |
Once daily between 5pm and 6pm (automated tasks on nursing hub) |
| Specialist clinics including day oncology reception |
With routine observations |
| Day Medical and Day Oncology |
Twice –on arrival with first set of observations and with last set of observations prior to discharge/transfer (4/24 for longer stay patients) |
If the patient is on less frequent observations (eg BD) it is important that the parent knows how to escalate concerns via the OneTEAM process independent of the nurse asking the question.
OneTEAM
On admission, the bedside nurse informs parents/carers and patients (as appropriate) of the four-stepped oneTEAM pathway.
1. Talk to your bedside nurse
2. Escalate to the nurse in charge
3. Ask for a rapid review
4. Medical Emergency Team
See OneTEAM Parents/carers Escalation of Care flow chart and the RCH Policies and Procedure: Medical Emergency Response Procedure.
Frequency of Observations
Clinical observations are recorded by the nurse as part of an admission assessment (
Nursing Assessment), at the commencement of each shift and at a frequency determined by the child’s clinical status and/or current treatment. For example, required observations during blood product transfusions and all fresh blood products can be found here RCH Policies and Procedures: Blood Transfusion - Fresh Blood Products and routine post anaesthetic observations can be found here
https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Routine_post_anaesthetic_observation/.
The frequency of observations and type of observations is ordered within EMR and should be documented in flowsheets
Observations should be performed at least once per hour if the patient:
- Has previous observations within the shaded orange or red zone (unless modified)
- Was transferred from PICU/NICU (as clinically indicated)
- Is receiving PCA, Epidural, or Opioid infusion
- Is receiving an Insulin infusion
- has ICP monitoring
- is receiving oxygen therapy
(Note, some children will require continuous monitoring as described later in this guideline).
A set of observations must be recorded within the hour before transfer from one area to another, for example from ED to ward, PICU to ward, PACU to ward, or ward to ward. If a child's observations are transgressing the Orange or Red zone, this must be addressed prior to transfer.
Each set of observations should be documented in EMR flowsheets and then trends should be viewed on the VICTOR graph, to better enable analysis and interpretation of the data. Link:
flowsheet learning resources. For observations entered via Spectralink device the trending of observations on the ViCTOR graph should be viewed as soon as practicable.
In the event of a “down time” of EMR all treating areas at RCH have a supply of the paper ViCTOR charts for all age groups. This information will later be uploaded to the EMR. On the paper charts the Red Zone is colored purple.
Coloured zones
Age-specific ViCTOR parameters are automatically set by the child's age in the EMR and when breached a notification for Escalation of Care is triggered. There are 3 distinct coloured ‘zones’ within the ViCTOR graph.
The White zone is considered the ‘acceptable zone’. That is, most patients trending in this area are considered to have acceptable age-related vital signs (
Acceptable Ranges for Physiological Variables.) Nevertheless, it is important to be vigilant – for example, a heart rate that is steadily rising in this White zone should trigger attention before crossing into the Orange zone.
The Orange zone is the first zone to signal that the patient may be deteriorating. It triggers the clinician to escalate care to the AUM (at a minimum) to decide if a medical review or other emergency response is required.
The Red zone is the second and more concerning trigger and signals that the patient may be deteriorating or is seriously ill. If the patient is in the Red zone, an emergency call must be initiated, that is, a Rapid Review or MET call. If the child’s observations transgress into the Orange or Red zone, then further details must be documented, including the Escalation of Care plan and response.
Appropriate escalation of care must occur as per the Deteriorating Patient: Escalation of Care flow chart and the RCH Policies and Procedure: Medical Emergency Response Procedure.
Remember, regardless of what zone the patient is in, if a staff member or parent is very worried about the child’s clinical state, initiate an emergency response.
Modification of the Orange or Red zone
Modification of the Emergency Response criteria may be ordered by medical staff, in accordance with the RCH Policies and Procedure: Medical Emergency Response Procedure. Please note that MET modifications are only valid for 2 hours for patients who are transferred from ED, Theatre or PICU. Thereafter any modifications should be made by the treating medical team.
O2 Saturation and oxygen delivery
Haemoglobin-oxygen saturations (SpO2) are entered numerically in the flowsheet.
Oxygen delivery refers to the flow (L/min) or percentage (%) of oxygen that the patient is receiving. If no oxygen is given, document 'RA' (room air).
Oxygen delivery guidelines.
The device used to deliver oxygen should be noted as follows:
- Nasal prongs (NP)
- Hudson Mask (HM)
- Humidified Nasal Prongs (HNP)
- High Flow Nasal Prongs (HFNP)
- Non-rebreather mask (NRM)
- Tracheostomy (T)
Standing medical orders for nurse-initiated oxygen therapy for PICU patients can be found here
PICU standing orders.
Heart rate
The HR is checked by palpation of the pulse or auscultation of the heart at least once per shift and whenever there is concern about the child’s physiological condition, a change in heart rhythm or when there is doubt about the accuracy of the monitoring technology. The pulse volume and regularity of HR should also be assessed at this time.
Bradycardia during sleep is common in children and may reflect a normal physiological response due to increased vagal tone. Assessment and management are outlined in (
https://www.rch.org.au/clinicalguide/guideline_index/Bradycardia_during_sleep/).
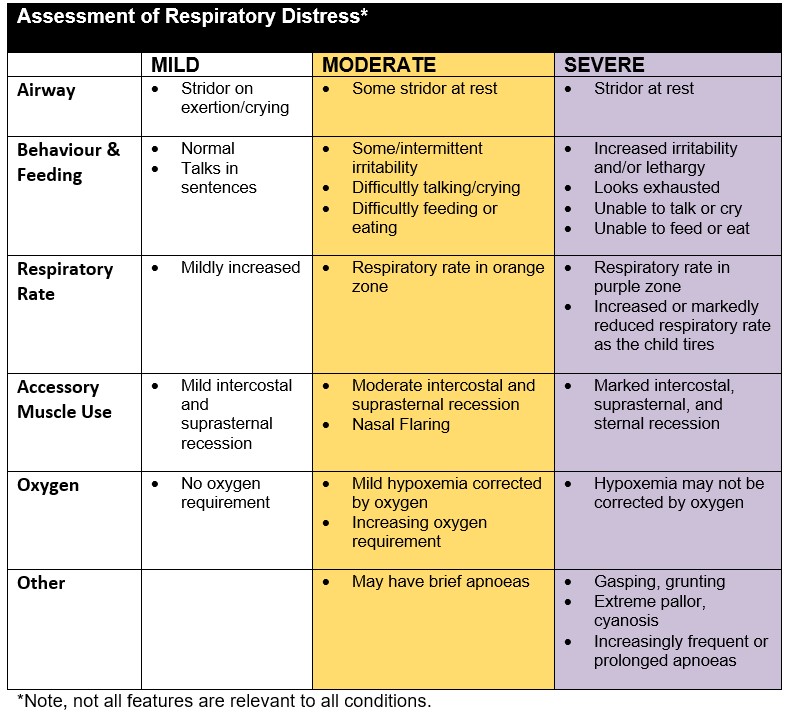
Respiratory rate
The RR is checked at least once per shift established by counting the patient’s breaths over 60 seconds. Further respiratory assessment including the pattern and effort of breathing should also be evaluated at this time. Respiratory distress should be recorded as Nil,
Mild, Moderate or Severe based on the assessment.
Blood Pressure
Blood pressure (BP) must be recorded as systolic, diastolic and mean BP. Only systolic BP triggers an escalation of care response. A measurement in the Orange zone reflects hypertension (upper zone) and in the Red zone, hypotension (lower zone).
BP should be assessed at least once on admission, and thereafter at a frequency appropriate for the child’s clinical state. If a child's pulse/heart rate falls in the Orange or Red zone, BP must be measured and documented. An assessment of BP, along with other clinical observations, may be necessary prior to mobilising a child in the early postoperative period. The limb used to measure BP should be documented as should the type of measurement (eg lying or standing).
Temperature
See
Temperature Management for guidance regarding temperature assessment and management . See the
Febrile child for management of the child with fever. NB: For infants under 3 months a low temperature, or temperature instability, can be signs of bacterial infection or serious illness
Alterations in temperature (Orange zone) should be reported to medical staff. Adjustments of temperature thresholds can be modified by medical staff using the VICTOR threshold modifications.
Level of Consciousness
Level of Consciousness assessment should be made by using the AVPU scale:
A = child is Alert (opens eyes spontaneously when approached).
V = child responds to Voice.
P = child responds to a Painful stimulus.
U = the child is Unresponsive to any stimulus.
A deterioration in the level of consciousness should trigger an Escalation of Care response.
The AVPU score may be difficult to determine for infants. Some infants may respond to the voice of a parent, but not a clinician.
Children should be woken before scoring AVPU. Conversely, in an otherwise clinically stable patient, it may not be appropriate to wake a sleeping child to assess the level of consciousness, with every set of observations (e.g. an infant with bronchiolitis who is on hourly observations for ongoing evaluation of respiratory distress and has just settled to sleep).
A more comprehensive neurological assessment must be performed for any patient who has, or has the potential, to have an altered neurological state. Neurological observations should ordered for children with:
Level of Sedation
Level of Sedation should be assessed ONLY for patients receiving sedation (e.g. chloral hydrate, midazolam, nitrous oxide, and opiates at higher doses) and the Level of Sedation score is to be used instead of the AVPU score.
The University of Michigan Sedation Score (UMSS) is used;
| 0 |
Awake and alert |
| 1 |
Minimally sedated: may appear tired/sleepy, responds to verbal conversation +/- sound |
| 2 |
Moderately sedated: somnolent/sleeping, easily roused with tactile stimulation or verbal command |
| 3 |
Deep sedation: deep sleep, rousable only with deep or physical stimulation |
| 4 |
Unrousable |
Guidelines for
procedural sedation.
Pain scores
Pain scores should be calculated by using a Pain Assessment tool appropriate for the age, developmental level and clinical state of the child. Nursing Clinical Guideline
Pain Assessment and Measurement. Suggested pain scales include
- FLACC scale for infants and toddlers and non-verbal children
- Wong-Baker Faces Scale for children 5 -17 years (may be used for some children from 3 years)
- Numeric rating scale for children over 8 years.
- (mPAT) (Neonatal Pain Assessment)
- COMFORT- B scale (used in PICU).
Additional Observations
Further patient specific observations may be required and ordered.
- Blood sugar level (POCT)
- Capillary refill time
- Non-invasive ventilation parameters
- Ventilation parameters
- Isolette/radiant heater temperature (under 1 year only)
- Nausea
Continuous monitoring
Continuous monitoring includes either cardio-respiratory monitoring or pulse oximetry monitoring.
Continuous monitoring supplements manually performed intermittent clinical observations. If used appropriately it can assist clinicians to identify rapid changes in condition. Some monitors enable the review of trends in physiological parameters over time.
Cardio-respiratory monitoring
Continuous cardio-respiratory monitoring is the technological measurement of HR/PR, RR and SpO2. Children who are clinically unstable or are at risk of sudden changes in condition should have cardio-respiratory monitoring. Some indications include:
- Potential or actual apnoeic or bradycardic episodes
- Recent unexplained sudden collapse
- Abnormalities of heart rate and rhythm or high risk of arrhythmia (e.g. pericardial effusion, altered electrolytes)
- Temporary pacing
- Prostaglandin infusion, medications that compromise cardiac function including concentrated electrolyte therapy, administration of pro-arrhythmic drugs with potential to cause QT prolongation or ventricular dysrhythmias, therapies associated with a high risk of anaphylaxis, administration of toxic medications)
- High risk of respiratory failure (e.g., infants with severe bronchiolitis)
- Post-operative assessment as ordered by medical staff (e.g. 24-48 hours post spinal surgery)
- In accordance with the
Apnoea Monitoring Postoperatively in Infants
Correct electrode placement when utilitsing ECG monitoring is vital. 3 lead ECG monitoring is most common however 5 lead ECG monitoring can also be used with the bedside monitors.
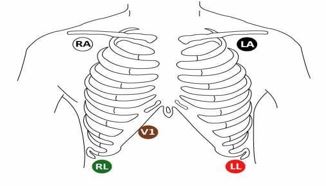
The above image shows the correct lead placement for a 5 lead ECG. When only using 3 leads, place the 3 coloured leads in the appropriate spots as outlined above. Commonly white (RA) , black (LA) and green (RL) are used for 3 lead ECG monitoring.
Skin preparation and regular changing of electrodes (usually daily) is vital to ensure accurate readings. For further information
Cardiac Telemetry Guideline.
Pulse oximetry monitoring
Continuous pulse oximetry monitoring measures oxygenation (SpO2) and pulse rate. Indications for its use include the child who:
- is receiving oxygen therapy and clinically unstable
- is clinically unstable and the need for oxygen therapy is yet to be determined
- has a nasopharyngeal airway or tracheostomy and requiring acute nursing care
- is receiving respiratory support (e.g., invasive or non-invasive ventilation)
- is undergoing a procedure where respiratory depressants are used
- is a high risk patient receiving an opioid infusion
- is in the immediate post-operative period
- has a decreasing conscious status
It is important to neither rely on nor ignore monitors. Whenever continuous monitoring of heart rate, SpO2 or respiratory rate is in use, clinical observations must be documented hourly, at a minimum. The heart rate should be cross checked by palpation of the pulse or auscultation of the heart at least once per shift and whenever there is concern about the child’s physiological condition, a change in heart rhythm or when there is doubt about the accuracy of the monitoring technology.
Alarm settings
Alarm limits should be set at the appropriate age-related profile selected on the monitor, where the default settings reflect the ViCTOR escalation of care parameters. Subsequent adjustment of the alarms may be required as the patient’s clinical status changes. That is, it may be necessary to set the alarm limits within a narrower range for some patients. Widening of the alarm limits must only be done in accordance with the procedure outlining the modification of emergency response criteria.
The patient profile and alarm settings should be checked at the beginning of each shift and as otherwise indicated. The key principle is to provide safe alarm settings for the child and minimise the number of false alarms. A high frequency of false alarms has the potential to desensitise staff and decrease their responsiveness, thereby compromising patient safety.
By turning the monitor into stand-by mode when not being used, all settings will be saved and available for the next set of observations. If the monitor is turned off by the power button displayed on the front of the monitor, all settings will be lost and need to be re-programed.
When commencing cardio-respiratory monitoring, make sure that the patient’s name is correctly entered into the monitor. When new patients are added to the monitor it is important that the correct Profile (age group) is selected otherwise alarm settings will default to the 1-4 year age group.
All alarms must be “enabled” (activated) and audible. When an alarm sounds clinicians should respond immediately, assess the child, determine and apply the appropriate intervention and rectify problems with monitoring devices if necessary. Parents are not permitted to disable or alter alarm settings.
Discontinuation of continuous monitoring
As the condition of the child stabilises and the risk of sudden deterioration lessens, the decision to continuously monitor the child should be reviewed by the nursing and medical staff (usually at least once per shift). When no longer necessary the patient can be transitioned to 1-4 hourly observations.
The need for close observation and monitoring should be balanced against unnecessary dependency on the monitors.
Companion documents
Evidence Table
Click here to view the evidence table.
Please remember to read the
disclaimer.
The revision of this nursing guideline was coordinated by Sharon Kinney, Nurse Consultant, Nursing Research, and Sarah Sly, Improvement Manager: National Standards, approved by the Nursing Clinical Effectiveness Committee. Updated November 2023.