Children become overweight due to a combination of different factors. The most common reason is a chronic imbalance between energy intake (food and drink) and energy use (physical activity). Family eating habits have changed considerably with greater consumption of take-away, lower consumption of homemade meals and larger portion sizes. In addition, it has become much easier to access higher energy snack-foods and sugary drinks (juice, soft drink, flavoured milk) which provide your child with unnecessary additional calories contributing to excess weight gain.
Children are spending a lot more time watching television and playing computer games than participating in sports and active play. Australian children watch, on average 2½ hours of television per day, in addition to other screen based activities (computer, electronic games). This is well above the current recommendations.
It is important to recognise, however, that there are also some rare medical problems that can cause children to gain weight excessively. Part of the healthcare professional's assessment in an overweight child will be to look for and rule out these rare medical conditions
Causes of obesity in children
Environmental
- Excess energy intake
- Decreased activity levels
Hormone problems
- Under functioning thyroid
- Problems with the production of growth hormone
- High steroid levels
- Other hormonal problems
Medications
- Behaviour-related medications (such as antidepressants
- Medications for fits and seizures
- Steroids
Genetic syndromes
- Prader-Willi syndrome
- Other genetic syndromes
The majority of children and adolescents who are overweight are physically healthy. If you have concerns regarding your child's weight, these should be discussed with your local doctor. The doctor will assess your child's weight, height, family background, dietary intake and activity levels and may request specific tests to assess for weight-related problems.
Talking to families and children about their weight: a guide for parents and carers
Discussing a weight problem is as important as discussing any other health concern. However, the focus of the conversation should be related back to healthy lifestyle behaviours and good health rather than overweight or obesity itself.
Tips
- Focus on behaviour and dietary change related to healthy lifestyle rather than losing weight
- Instead of using negative words like 'fat', 'heavy' or 'obese', use phrases like 'above his/her healthiest weight'
- Don't compare your child to other children and don't allow them to do the same
- Get the whole family involved in the conversation – what is good for one child is good for the entire family
- Explain to your child why you/the doctor are concerned, e.g. maintaining a healthy weight/lifestyle now will help prevent getting sick as an adult
- Try not to label food/activities as 'good' and 'bad', uses words like 'healthy', 'healthier option/choice', 'sometimes/occasional food'
- Be careful not to make negative comments about your own weight/body shape as children/adolescents pick up on these and can potentially relate the comments to themselves
- NO DIETS! Diets often encourage unhealthy and, at times, unsafe eating behaviours. When considering making a dietary change you should consider whether your child will be able to incorporate this change into their regular meal pattern for the rest of their life. If you are unsure you can seek advice from a healthcare professional, e.g. dietitian.
Weight management: Why the whole family needs to be involved
Parents are often seen as the key motivator of change for younger school-age children, whereas adolescents can, and should, have the chance to make goals and changes separately from (but with the support of) their parents. It is important that the goals are realistic and appropriately targeted towards achieving a healthy weight. The emphasis is on improving health, fitness and social functioning. Reducing the risk of weight-related problems is much more preferable than goals that are aimed at achieving an ideal body weight. Young people often report that temptation is everywhere. Removing temptations from the household is often a good way to start. Choose short term goals that help your child/adolescent feel like they achieving their goals. If they know the effort they are putting in is helping them meet their goals they will be much more likely to achieve long term successful weight management.
Where can I go for advice and support?
Medical
GP/Paediatrician – your primary medical carer is often the best place to start. They will be able to complete a comprehensive assessment of your child's health and weight status. They can offer continued support with regular reviews during your family's weight management journey as well as referring you to local allied health services for additional support.
**Don't forget to ask your GP if your child qualifies for a Medicare Benefits Schedule Chronic Disease Management Plan which will enable them to have regular subsidised visits with an allied health team.
Allied health
- Dietitian
- Psychologist
- Social worker
- Exercise physiologist/physiotherapist
Primary care is generally the first point of contact for people seeking medical advice. It is also a well-supported environment for families seeking advice around overweight and obesity.
As overweight and obesity is often the result of exogenous dietary and lifestyle factors it is important to create a support network of allied health practitioners to assist the family in addressing these contributors to excess weight gain. This may include a nurse, dietitian, social worker, counsellor/psychologist and/or exercise physiologist.
For a general practitioner or paediatrician performing an initial consult and examination for childhood obesity the following is recommended as a baseline:
Talking to families and children about their weight: a guide for healthcare professionals
As with any other health issue, concern about a child’s weight should be discussed with the child and their family/carers. Healthcare professionals are at time reluctant to raise concerns about obesity with patients and families, having concerns about their own discomfort or family discomfort, particularly if other family member are also overweight or obese. It is important to remember that parents expect healthcare professionals to raise and address all of their concerns about a child’s health.
Things to remember
- Use the appropriate growth charts as a reference for assessing a child’s weight. This will reassure the child/parent that you are making a standardised assessment rather than giving your own opinion of their child’s weight
- Focus on:
- health - the aim of weight management is to diminish risk of morbidity and mortality with an emphasis on improving health and fitness
- improving social functioning rather than aesthetic ideals
- Use an encouraging and empowering approach that is age appropriate. Avoid using negative language such as ‘fat’, ‘chunky’ or ‘obese’. Use phrases like ‘above his/her healthiest weight’ or ‘the healthiest weight for your child is…’
- Explore the family’s:
- motivation for making healthy lifestyle changes
- barriers to being able to make changes – consider referrals to other healthcare professionals, e.g. social work or psychologist, to assist with overcoming these hurdles.
- Get the whole family involved in the conversation – what is good for one child is good for the entire family
- Try not to label food/activities as ‘good’ and ‘bad’, uses words like ‘healthy’, ‘healthier option/choice’, ‘sometimes/occasional food’
- NO DIETS! Diets often encourage unhealthy and, at times, unsafe eating behaviours. When considering suggesting a dietary change you should consider whether the child/family will be able to incorporate this change into their regular meal pattern for the rest of their life. If you are unsure you can seek advice from a healthcare professional, e.g. dietitian.
GP/Paediatrician assessment of the overweight child
- Pubertal stage (e.g. using Tanner staging)
- Acne and hirsutism
- Blood pressure (with appropriate cuff size)
- Morning headache and visual disturbance (potential benign intracranial hypertension)
- Abnormal gait, problems with feet, hips and knees, difficulties with balance and coordination
- Gastrointestinal symptoms (vomiting, abdominal pain, constipation, gastrointestinal reflux)
- Nocturnal enuresis and daytime dribbling
- Hip and knee joint pain
- Presence of intertrigo
- Presence of hepatomegaly
- Signs of dysmorphism
- Thyroid function (e.g. presence of goitre)
- Acanthosis nigricans (velvety, light brown-to-black markings usually on the neck, under the arms or in the groin), which suggests significant insulin resistance
- Short stature, a low growth velocity, or bruising or purple striae (may indicate an endocrine cause for weight gain)
- Dental health
Diet and exercise history
- Average daily food intake (refer to dietitian)
- Activity levels
- Time spent watching TV/computer
Screening investigations
Baseline:
- Blood lipids
- Liver function tests
Consider the following when clinically indicated
- Blood sugar and HbA1c or OGTT
- Hormone function, such as thyroid hormone levels
- Vitamin and nutrient levels (such as Iron, vitamin D, Vitamin B12)
Management
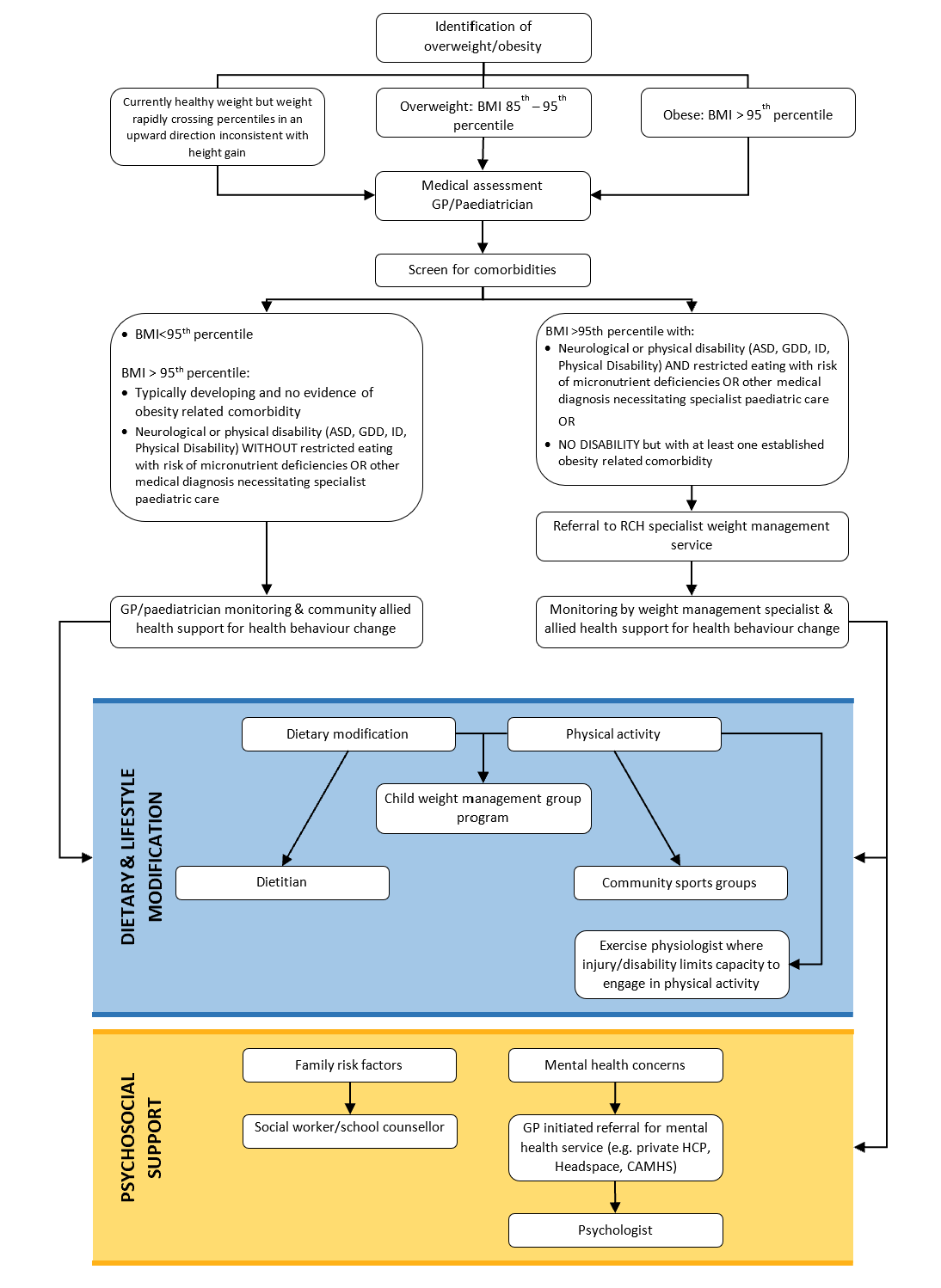
When BMI is above the 95th percentile (US-CDC growth chart) and there are NO comorbidities or other medical or developmental conditions that would require specialist weight management support ongoing management and support should continue in primary care, coordinated by the GP/paediatrician +/- practice nurse.
Consider referral to the appropriate allied health:
- Dietitian
- Psychologist
- Social worker
- Exercise physiologist/physiotherapist
- Occupational therapist
Referral to the RCH specialist weight management clinic is required when:
BMI >95th percentile with:
- Neurological or physical disability (ASD, GDD, ID, Physical Disability)
AND
- restricted eating with risk of micronutrient deficiencies (Iron, Vit A,C,E, B12) OR other medical diagnosis necessitating ongoing specialist paediatric care
BMI >95th percentile with NO DISABILITY but with at least one established obesity related comorbidity:
- LFT abnormality
- Hyperlipidaemia
- Hypertension
- Impaired glucose tolerance
- Obstructive sleep apnoea (please also refer to Respiratory at the time of referral to Weight Management, faxed as separate referral)
- Orthopaedic complication (NB: SUFE must have Endocrinology referral and assessment prior to being referred to Weight Management Service)
Please note
As with many hospital-based services there may be a waiting period to see the RCH Weight Management Service. GP/Paediatrician management of obesity with the support of community/primary care allied health clinicians should continue until a referral to the RCH Weight Management Service has been accepted and the child has been assessed by the Weight Management team to decide whether the child should continue with primary or tertiary care management.