Table of contents will be automatically generated here...
Key points
- Children
are particularly vulnerable to ocular trauma.
- Serious
eye injuries can be under appreciated in the child who has a painful eye,
blurred vision or extensive subconjunctival haemorrhage.
- Ensure
prompt and adequate analgesia.
- If
a ruptured globe is suspected or identified: stop examination, place an eye
shield over the eye to avoid extrusion of ocular contents, obtain a CT Orbit
(if there is a history of a possible foreign body), keep nil by mouth and refer
urgently to ophthalmology.
Introduction
Paediatric ocular trauma is a cause of significant
morbidity, with up to 280,000 hospital admissions worldwide per year. [1]
However, hospital admissions only account for around 5% of total eye injuries –
so it has been estimated that worldwide there are around 6 million episodes of
eye injury in children.[2] Open globe injury (ruptured globe due to
blunt trauma, or laceration due to a penetrating injury) is a severe form,
which, in children, is most commonly caused secondary to penetration with a
sharp object whilst at home.[3]
Children account for between 20 and 59% of all eye injuries[4]. They are more predisposed to eye injury due
to their developing physical coordination, limited ability to detect
environmental risks and a more vulnerable facial morphology.[5] The outcome of paediatric eye injuries is
worse than that of adults due to their visual immaturity, increased years of
visual loss and potential for amblyopia.[5] Most paediatric eye
injuries (66.2%) occur during play – predominantly whilst at home under
supervision of parents / caregivers (47.7%), but often whilst at school /
nursery (24.4%).[2] Sharp
instruments are the most common cause of injury, followed by plants, animals,
toys or sports equipment.[2] In the Australian context, it has been
estimated that sports-related eye injuries make up 11% of all paediatric eye
injuries. [6] Boys are twice as likely to sustain a significant eye
injury compared to girls.[2]
Features of ocular trauma history and examination (see also RCH Clinical Practice Guideline: Acute eye
injuries in children and RCH Clinical Practice Guideline: Penetrating eye injury)
Serious eye injuries can be under-appreciated when children
present with a painful, blurred vision or an extensive subconjunctival
haemorrhage. In all traumatic eye
injuries consider the following principles: [7]
- Manage (other) life threatening injuries
- Ensure the structural integrity of the globe
- Assess vision in the injured AND the uninjured
eye
- Seek ophthalmology consultation where required
Where an open globe injury is suspected it is important to
minimise child distress – as crying can raise ocular pressure leading to
extrusion of intraocular contents.
The key diagnoses to seek and identify are:
- Open globe injury – ruptured globe or
penetrating laceration
- Foreign body – corneal or intra-ocular
- Large hyphaema
- Retinal detachment
- Corneal burns – chemical or thermal
History
Symptoms
- Pain – at rest or with movement
- Vision - loss (ongoing or temporary, global or
central) or blurring or other disturbances such as flashes (associated with
retinal detachment) or floaters (associated with intra-ocular injury)
- Foreign body sensation – pain with blinking or
moving eye
- Discharge from the eye
- Photophobia
Mechanism
of Injury
- Risk of high velocity penetrating injury – small
projectiles at high velocity have a higher risk of penetration - eg playing
with air-rifle, near lawn-mowers, using metal grinders or other power tools,
hammering
- Risk of low velocity penetrating injury – eg
running with sharp object, catching eye on sharp thorn or plant material
- Risk of blunt injury -eg sports injury such as squash ball to
orbit, motor vehicle accident (be aware an airbag ocular injury to a front seat
passenger can be a combination of a blunt or penetrating injury with a chemical
burn)
- Risk of chemical or burn injury to eye – eg
flash burn to face, playing with detergent pods. Alkali burns are generally more dangerous
causing liquefactive necrosis.
Other
- Any
first aid already provided?
- Glasses
or eye protection worn?
- Presentation
maybe delayed so ask for history over the previous few weeks.
- History
of previous trauma to eye(s).
- Associated
trauma/injuries.
Examination
If adequate examination is not possible due to either the
child’s age or level of cooperation, specialist assistance should be
sought. Where there is significant
concern for an open globe injury, it is prudent not to overly distress the
child through multiple attempts at examination, as crying can lead to an
increase in intraocular pressure, with the resultant extrusion of intraocular
contents. Early referral to ophthalmology
is appropriate in these cases – along with administration of appropriate
systemic and topical analgesia and anti-emetics. Ondansetron is an appropriate option, as it
has a lower risk of causing a dystonic reaction. Opiate analgesia may lead to nausea and
vomiting which can increase intra-ocular pressure – so consider pre-treating
with anti-emetics if you think strong analgesia is required.
Even when open globe injury is not suspected, appropriate
analgesia, oral or intranasal analgesia as well as topical (single drop of
preservative free local anaesthetic – eg amethocaine 1%) should be given to
reduce pain and aid the child’s ability to tolerate examination. However, it is worth noting that local
anaesthetic is itself a direct epithelial toxin, so it shouldn’t be used
repeatedly (and patients should not be discharged with topical local
anaesthetic). A child life specialist
(play therapist) may also assist in helping the child relax during an
examination. Be aware that when a child
has suffered a monocular injury, occluding the good eye may increase their
distress (as they will no longer be able to see).
Where a burn is suspected, first aid should take precedence
over a complete examination. This
consists of copious irrigation (after local anaesthetic and systemic analgesia
given). In some cases the patient may
need to be sedated to facilitate first aid treatment.
A complete examination of the eyes requires examination of:
1.Visual acuity in both the injured and uninjured
eye
- Use age appropriate charts and the patients
normal corrective lenses or pinhole
- Snellen chart from school age
-
“E” chart from about 3 years old
-
Kay picture book – ages 2-3
A difference of more than 2 lines on an eye
chart is likely to be significant. If unable to read a chart, check the patient can
count fingers or confirm light perception
2.Eye movement
- Check the child can look in all directions
- Check for diplopia or pain with eye movement
- In trauma, an orbital floor fracture can lead to
reduced upward gaze (entrapment of inferior rectus)
3.Visual fields
- Four quadrant testing in older children
- Traumatic visual field loss is usually grows,
however, subtle changes may occasionally occur with retinal detachment and
intra-ocular foreign bodies
4.Pupils
- Check size, symmetry, shape and reactivity
- Look for both a direct and indirect pupillary
response
-
A relative afferent pupillary defect may suggest
an increase in retrobulbar pressure (ie a retrobulbar haemorrhage secondary to
trauma), optic neuropathy or severe retinal detachment.
5.Lids, conjunctiva and sclera
- Look for swelling, chemosis, ptosis, ecchymosis
and lacerations
- Evert the lids to look for foreign bodies on the
underside
- If there is a laceration on the eyelid – check
to see if it extends through the tarsal plate – maintain a high level of
suspicion for globe rupture in the presence of any eyelid laceration
- Look for a subconjunctival haemorrhage – whilst
many are benign, a localised haemorrhage may suggest penetrating injury. An
inability to visualise the posterior extent of a subconjunctival haemorrhage
may suggest an orbital or base of skull fracture. In infants, subconjunctival haemorrhage may
be a sign of non-accidental injury.[8]
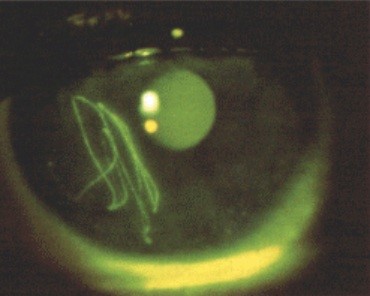
6.Cornea, Anterior Chamber and Iris
- Look for a hyphaema – this is blood in the anterior
chamber – mild cases may only have suspended red blood cells seen in the
anterior chamber.
- Check there is no iridodialysis – a disinsertion
of the iris from the sclera
- Look for corneal abrasions and foreign bodies
-
Application of fluroscein dye will help identify
abrasions
-
Vertical scratches on the cornea indicate the
likely presence of a foreign body under the upper eyelid
7.Fundus
- Look for red reflex, assess the optic disc, the
macula and periphery
- A red reflex may be diminished due to vitreous
haemorrhage or lens opacity
- Retinal detachment may be seen as a grey flap
- Check for retinal haemorrhages and papilloedema
8.Palpate the orbital rim
- Assess for bony fractures
- Check for paraesthesia in the infra-orbital
nerve distribution
9.Consider assessing intraocular pressure
- In the context of trauma, and intraocular
pressure of <10 will indicate a potential globe injury
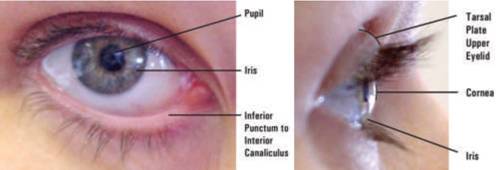
Make sure to document the location of injuries according to the external eye anatomy as shown in Figure 1.
Fig 1: External anatomy of the eye
Ocular Trauma
Blunt
- Intraocular
contents are at risk of considerable damage by blunt force trauma.
- Orbital
bony wall is relatively thin thus susceptible to fracture from transfer of
mechanical energy across globe.
- Potential
Injuries:
- Lid injury
- Orbital blow-out fracture
- Retrobulbar haemorrhage
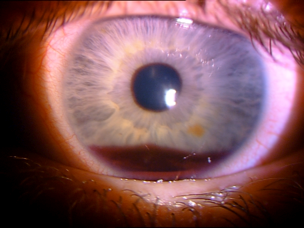
- Hyphaema - this refers to blood in the anterior chamber and is secondary to a tear in the iris and / or ciliary body. (see Fig 2.)
- Traumatic mydriasis – associated with iris
sphincter tears.
- Iridodialysis - this is the detachment of the iris root from its insertion site at the ciliary body. It can lead to a "D-shaped" pupil.
- Lens dislocation
- Cataract
- Vitreous Haemorrhage
- Retinal detachment
- Traumatic Iritis - or inflammation of the anterior chamber post blunt trauma is common in children. Examination reveals anterior chamber cell and flare, there may also be a poorly reactive pupil, with sustained miosis.
- Ruptured
Globe – (see below).
- Consider
CT Orbit +/- brain when concerned about blowout fracture or head injury.
- Immediate
Ophthalmology consultation is indicated in:
- Actual Globe or corneal perforation
- Concern of globe rupture
- Orbital haemorrhage
- Lens dislocation
- Visual changes
- Lid laceration
Fig 2: Hyphaema after blunt trauma
Open globe injury
Open globe injury refers to a full-thickness mechanical
injury to the cornea and/or sclera. The
two broad types are[3]:
- Ruptures – which result from blunt trauma such
as a ball striking the orbit and
- Lacerations – which are caused by a sharp object
entering the globe. Lacerations are
further classified as:
- Penetrating injuries – where there is a single
wound to the globe - for example from point of knife
- Perforating injuries – where there are separate
entrance and exit wounds
- Intra-ocular foreign body – where there is an
entrance wound with a foreign body within the globe – for example from a metal
splinter in a grinding injury
Penetrating injuries are the most common, followed by
intraocular foreign body injuries, then rupture, with perforating injuries
being the least common. The most common
location for injury is at home – especially for pre-school children. Older
children are increasingly likely to sustain an open globe injury outside of the
home.[9] A common cause of injury is
kitchen items, followed by sticks, pencils, metallic and elastic objects. Older children may suffer projectile injuries
through hammering or the use of paintball guns / air rifles.
If
penetrating eye injury is suspected:
- Do NOT force the eyelid open as pressure on the
lids may cause extrusion of ocular contents.
- Do NOT attempt to remove a protruding foreign
body from the globe.
Symptoms
- Pain
- Decreased visual acuity
Signs
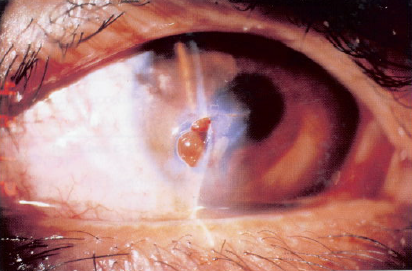
Anterior signs: peaked or irregular pupil, iris
prolapse, corneal laceration, hyphaema, extensive subconjunctival haemorrhage and chemosis (conjunctival swelling).
Posterior signs: poor red reflex (vitreous
haemorrhage), decreased vision, uveal prolapse,
Treatment
- Keep patient fasted in anticipation of theatre.
- Adequate analgesia with antiemetics as vomiting
may increase intra-ocular pressure.
- Sit patient upright where able (may depend on
ability to clear C-spine)
- Shield the eye, be careful when shielding not to
press on the eye.
- Do Not instil drops or ointments into eye.
- Prompt discussion with ophthalmologist
- CT scan of orbit to investigate for ocular
foreign body.
- Commence ciprofloxacin and check tetanus status.
Fig 3. Corneal laceration with prolapse of iris following penetrating trauma
Orbital blow out fracture
These occur following high
energy blunt traumas (e.g. hit with ball, bat or fist) that create an increase in intra-orbital pressure.
Symptoms
These include pain and diplopia (especially on vertical movement), tenderness, eyelid
swelling. Nausea +/- vomiting and pain on eye movement may occur if there is entrapped
muscle.
Signs
Ptosis, tenderness, restricted eye movements (especially on vertical
movement), crepitus of lower lid. The globe may appear "enopthlamic" (recessed into the orbit) or displaced downwards. There may also have associated ocular injuries secondary to blunt trauma – (see above). Infraorbital nerve involvement leads to reduced sensation
to cheek, upper teeth and gums of affected side.
Fig 4: A 4yo child with right orbital 'blow out' fracture associated with entrapment

Management
- CT scan with coronal cuts is the investigation of choice to assess the integrity of bony orbit.
- Refer to Ophthalmology and Plastic Surgery units.
Fig 5: Isolated right orbital floor fracture

Non accidental injury (NAI)
Non-accidental
causes are a common and significant cause of ocular trauma in paediatrics.
Red
Flags
- Unexplained periorbital haemorrhage, especially
in setting of other injuries.
- Poorly or unexplained mechanism of injury.
- Any burns in a small child.
Detailed
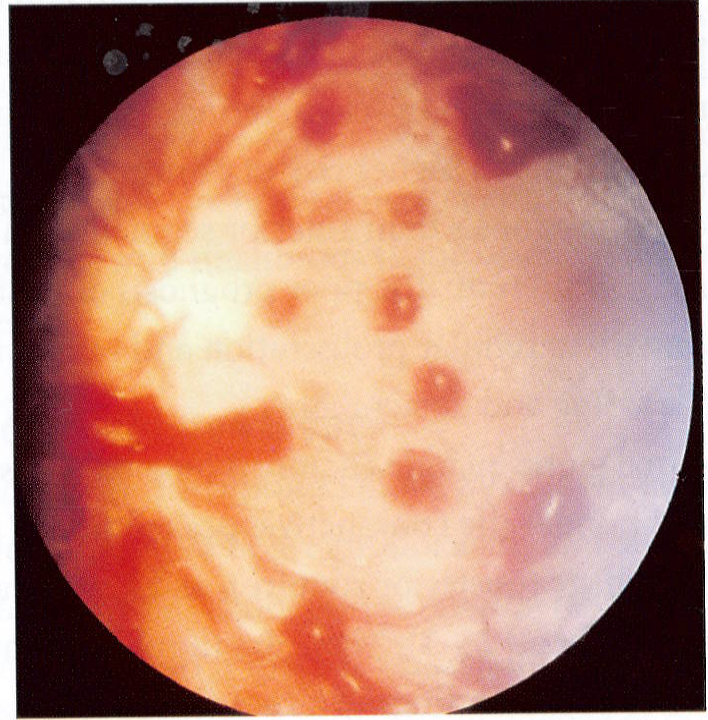
fundoscopy by an ophthalmologist is required in all cases of suspected NAI, and
should be considered in all cases of head injury of infants and young children.
Key
pathological findings include: Extensive multilayered (retinal, pre-retinal and
subretinal) haemorrhages in all four quadrants with possible vitreous
haemorrhage
Fig 6: Retinal haemorrhages following non-accidental injury
Chemical burns
Acid
and alkaline solutions that come into contact with the eye surface can cause
considerable damage and are a true ophthalmic emergency. Immediate
irrigation prior to arrival in ED is ideal, if this hasn’t occurred it should
be performed on arrival to ED
To
facilitate irrigate of the eye:
- Instil local anaesthetic drops to affected
eye(s)
- Irrigate with normal saline - minimum one litre, aim to include under
eyelids and conjunctival fornices.
- If possible use a Morgan Lens otherwise continue
irrigation using a gloved hand to retract lids as possible.
- Review patient’s pain regularly, re-instil local
anaesthetic drops 10 minutely as required.
- After one litre of irrigation, review the
eye. Wait 5 minutes after ceasing
irrigation to check eye pH using universal indicator paper, aim for pH equal to
unaffected eye or if both eyes are effected then aim for pH close to neutral;
discuss with specialist and continue irrigating if outside this range.
- Severe burns will usually require a minimum of 30
minutes of irrigation.
All
chemical burns should be assessed by ophthalmology after wash-out.
Alkaline
burns are especially damaging as the base solution will denature proteins, lyse
cell membranes which enhances penetration into the eye and increases further
damage.
Acid
solutions also cause severe damage, however acid solutions largely precipitate
proteins which can limit the area and depth of necrosis.
Corneal abrasions and foreign bodies
One of the most common paediatric ocular presentations to
emergency:
- Present with (often sudden onset) painful and
watering red eye.
- Use slit lamp, if available and child can
tolerate, or ophthalmoscope for examination.
- Examine both pre and post instillation of 2% fluorescein
drops to identify foreign body and potential corneal abrasion by the child inadvertently
rubbing their eyes.
- Always evert lids if possible. Most subtarsal
foreign bodies will be close to the eyelid margin.
Precautions
- Attempt to remove the foreign body as retained matter can
cause issues: infections if organic, rust rings if metallic.
- Upon successful removal of foreign body and in setting of
corneal abrasion, discharge with topical antibiotic drops (e.g. chlorsig) and
consider antibiotics ointment nocte as lubricating effects are soothing and can
help with sleeping.
To remove the foreign body
- Instil topical anaesthetic drop (e.g. tetracaine
hydrochloride 0.5%); warn the patient the drop will sting briefly.
- Attempt to remove foreign body with a moistened cotton
bud.
- If unsuccessful and if child is able to tolerate
sitting still at a slit-lamp, use a 25 gauge needle with bevel up to remove
corneal foreign bodies.
- If still unsuccessful after 2 attempts, cease
and contact Ophthalmology.
Fig 7: Corneal foreign body - metal fragment with rust ring
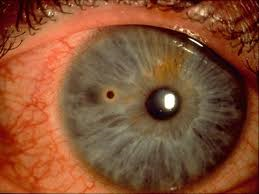
Fig 8: Linear corneal abrasions suggestive of a subtarsal foreign body
Lid lacerations
An
eyelid laceration should be treated as a potential penetrating injury until
proven otherwise. Superficial
laceration away from the lid margin, may be safely closed by standard suture
techniques. However any laceration that
involves the eyelid margin should be repaired by an ophthalmologist given the
complex lid anatomy (tarsus, grey line, medial and lateral longitudinal tendons
and canaliculus).
Lacerations,
even minor, to the medial canthus may involve the canaliculus and thus should
be referred.
Treatment
- Control the bleeding with elevation of head and direct pressure. Avoid pressure to the globe.
- Examine eye for penetrating injury once lid-bleeding is controlled.
- Suspect canalicular injury, if the medial part of either the upper or lower eyelid is involved. In this situation, early involvement of the Ophthalmology Unit is required.
References:
- Abott J, Shah P.
The epidemiology and etiology of pediatric ocular trauma. Surv
Ophthalmol. 2013; 58(5):476-485
- Sii, F et al. The UK Paediatric Ocular Trauma
Study 2 (POTS2): demographics and mechanisms of injuries. Clinical Ophthalmology 2018:12:105-111
- Xintong, L. et al. Pediatric open globe injury: A review of the
literature. K Emerg Trauma Shock
2015;8(4):216-223
- MacEwen, CJ. Et al. Eye injuries in children: the current
picture. Br J Ophthalmol. 1999;83:933-936
- Hoskin, AK. Et al. Eye Injury Prevention for the Pediatric
Population. Asia-Pacific J Ophthalmol
2016 5(3):202-211
- Hoskin AK et al.
Sports-related eye and adnexal injuries in the Western Australian
paediatric population Acta Opthalmologica
2016;94:e407-e410
- Root, JM et al.
Nonpenetrating Eye Injuries in Children. Clinical Pediatric Emergency Medicine 2017;18(1):74-86
- DeRidder, CA et al. Subconjunctival Hemorrhages in Infants and
Children: A sign of nonaccidental Trauma. Ped
Emerg Care 2013;29(2):222-226
- Gunes et al.
Characteristics of Open Globe Injuries in Preschool children Paediatric Emergency Care 2015;31(10):
701-703