Table of contents will be automatically generated here...
Introduction
In the primary survey, circulation becomes the priority after airway and breathing have been definitively managed. Delivery ofoxygen to the tissues is dependent on adequate circulation. In this chapter, differences between adults and
children are discussed followed by a review of circulatory compromise and its definitive management.
How are children different?
-
Normal vital signs vary with age;
-
Blood volume is relatively larger (80-90ml/kg) than that of adults (65-70mls/kg);
-
Blood volume is relatively smaller in absolute terms (800mls in a 1-year-old);
-
Children compensate for large intravascular losses (more than 30%) before becoming hypotensive.
-
Chest-wall is more compliant than in the adult. Therefore major contusions or lacerations to the heart and lungs may occur in the absence of rib fractures.
-
Urine out-put is relatively greater (Child 1-2mls/kg/hr; Adult 0.5mls/kg/hr)
Hypotension indicates that death is
imminent.
Causes of circulatory compromise
-
Respiratory failure/hypoxemia/hypercarbia;
-
Blood loss - internal or external;
-
Tension pneumothorax;
-
Pericardial tamponade;
-
Ruptured ventricle (rare);
-
Cardiac contusions;
-
Acidosis;
-
Burns;
-
Profound hypothermia.
Effects of circulatory compromise
-
Decreased or complete loss of consciousness;
-
Respiratory distress/failure;
-
Hypovolaemia: - Reduced cardiac output leads to inadequate blood flow to all body organs (Hypovolaemic shock);
-
Tissue hypoxia, metabolic acidosis and increased respiratory rate;
-
Ischaemic injury to the brain, heart, kidneys, liver, bowel with cell death and inadequate function of these organs.
In all aspects of trauma management,
the primary survey is the first priority
Primary survey
Airway with c-spine stabilisation
(see airway management section) Breathing
(see breathing management section)
Circulation assessment and management
Circulation assessment
Examine
Pulse
-
Brachial artery in an infant, up to 1 year;
-
Carotid artery in a child, 1 year or older
-
Femoral artery
-
Tachycardia - is a sign of shock, as well as of fear and anxiety.
-
Bradycardia - is a sign of imminent death.
-
Pulse volume is reduced in shock
Capillary Refill
-
Press on the sternum for 5 seconds then release and count the time to reperfusion. Up to 2 seconds is normal.
-
Capillary refill is prolonged early in shock, but is also prolonged by pain, fever and environmental factors, such as cold.
-
This is a sensitive sign, but not specific, and should only be used in conjunction with other signs of shock.
Skin colour/temperature
-
Mottling/pallor and cyanosis of the skin indicate poor perfusion due to either a sympathetic response to low cardiac output or to pain, fear or cold.
Blood Pressure
-
Hypotension is a late sign of shock, and imminent death.
Look for other signs of circulatory inadequacy
-
Respiratory distress or failure;
-
Agitation, confusion or decreased conscious level;
-
Rapid, deep breathing may be a sign of metabolic acidosis
-
Decreased urinary output.
Management of circulation
-
Consider need for chest compressions
-
Ensure adequate vascular access
-
Obtain blood specimens
-
Assess and manage haemorrhage
-
Fluid Resuscitation
-
Drugs
-
Re-assessment
Ensure adequate monitoring of saturations: cardiac monitor, finger on femoral pulse for pulse check.
If the pulse is abscent or less than
60 and there are no other signs of life: commence immediate chest
compressions and full cardiopulmonary resuscitation.
1. Chest compressions Infant <1 year
| Landmark |
1 finger-breadth below inter-nipple line. |
| Technique |
Two fingers depth 1/3 of the AP diameter of the chest |
| Rate |
100 per minute |
Ratio of compressions to breaths: 5:1

landmark infant
Small Child <8 years
| Landmark |
1 finger breadth above the xiphisterum |
| Technique |
Heel of one hand - depth 1/3 of the AP diameter of the |
| Rate |
100 per minute |
Ratio of compressions to breaths 5:1
Larger child
Landmark Two fingers above the xiphisterum Technique Two hands overlaid (as in adults) Rate 100 per minute Ratio of compressions to breaths 15:2
2. Ensure adequate vascular access

-
At least 2 large-bore cannulae.
-
If unable to obtain access in 90 secs, insertion of an intra-osseous needle is recommended.
-
If experienced in advanced vascular access, consider inserting a large-bore, rapid-infusion canula into the femoral, internal jugular or subclavian where major ongoing blood loss.
-
Venous cut down. Use only as a last
resort.
Sites of venous access
-
Medial antecubital fossa at the elbow.
-
Long saphenous vein at the ankle.
-
Cephalic vein higher in the upper arm.
-
Dorsum of hand and foot; use in an infant when it has not been possible to cannulate a larger vein. Usually a Size 22G cannula can be inserted. This may be sufficient for initial volume expansion, but will be insufficient in older children, if there is ongoing
bleeding or a poor response to the initial fluid bolus.
-
Intra-osseous. In a child with established shock, if venous access cannot be gained within 90 seconds, insertion of an intra-osseus needle is recommended
(See chapter 2).
-
Femoral vein if skilled, and there is no severe intra-abdominal or pelvic haemorrhage.
3. Obtain blood specimens for:
-
FBC,
-
Blood sugar
-
Cross-Match (minimal requirements): -Infant 2 units -Child 4 units -Large child 6 units
4. Assess and manage haemorrhage
Control haemorrhage:
-
External: Assessment of blood loss (at the scene, in the linen, on the floor). Remember the scalp, which can be a major source of blood loss in children. Most external haemorrhage in children can be controlled with direct pressure. Use of focal pressure with limited dressings is more likely to control bleeding than large bandages. Where extremity bleeding cannot be controlled with direct pressure, a tourniquet may be helpful.
-
Internal: Chest and abdomen bleeding may require surgical intervention in order to achieve control.
Splint and stabilise fractures.
-
Pelvic fractures may cause significant blood loss, and a binder to the pelvis may substantially reduce this. A sheet or towel wrapped tightly around the entire pelvis may stabilise the haemorrhage.
-
Later definitive control in theatre - where appropriate.
5. Fluid Resuscitation
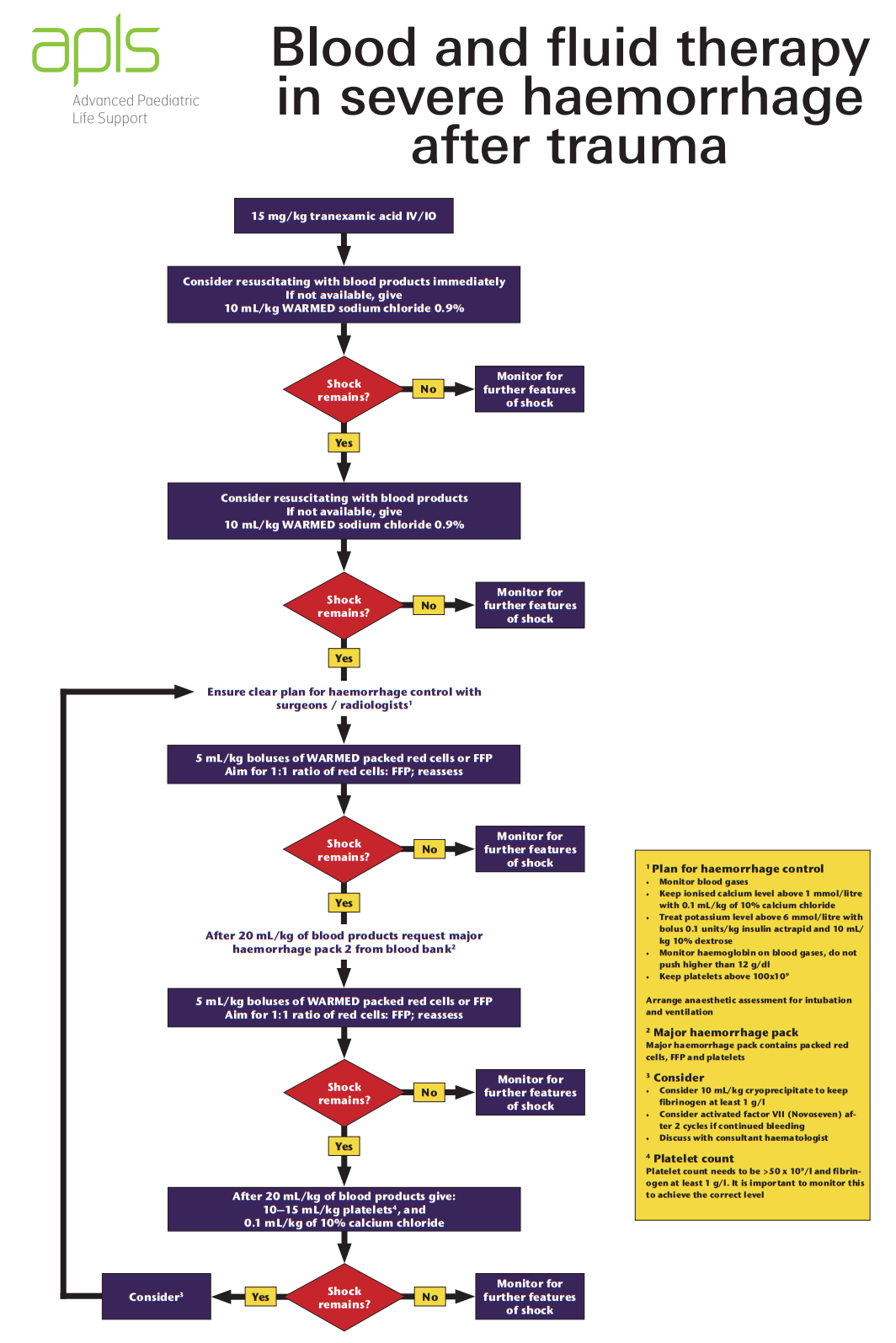
Look for any signs of circulatory compromise, as above. If present consider fluid resuscitation with blood as per your own institution protocol, or as per the APLS algorithm below:
Obtain an URGENT
SURGICAL REVIEW if there has been inadequate response to the first two fluid boluses.
Reassess: HR, capillary refill, and other signs of circulatory adequacy.
If the circulatory signs are deteriorating and not
responding to fluid bolus, consider whether there is:
-
Presence of on-going internal bleeding;
-
Tension pneumothorax;
-
Haemothorax;
-
Haemopericardium;
-
Spinal cord injury (low blood pressure, warm skin, slow heart rate, no limb movement, patulous anus).
In hypovolaemia, fluids will need to
be infused rapidly.
This requires:
-
50 ml bolus via syringe for small volumes and small children;
-
Rapid infusion catheters, if available;
-
Blood pump sets;
-
Pressure bags;
-
Blood warmers.
6. Inotropic support
Injured patients usually require replacement of volume rather than use of inotropes. Consider discussion with a paediatric intensive care physician if you consider your patient requires inotropic support.
7. After assessment: re-assessment
Repeat Primary Survey and continue monitoring vital signs, saturation, conscious state and urine out-put.
Specific management issues of circulation
-
Burns
(see burns / management of burn wounds clinical practice guideline)
-
Head injury (see head injury section)
-
Cardiac tamponade (see
chest injury section)
-
Myocardial contusions (see chest injury section)
-
Pneumothorax (see chest injury section)
-
Haemothorax (see chest injury section)
Suggesting reading list
-
Advanced Paediatric Life Support. 6th ed. John Wiley & Sons, 2017
-
Fleisher G, Ludwig S (eds): Textbook of Pediatric Emergency Medicine (4th ed). Philadelphia: Lippincott 2000. Chapters 1 (Resuscitation: pediatric basic and advanced life support); 10 (Cardia emergencies); 104 (Major trauma); 3 (Shock);.
-
Bersten A, Soni N (eds): Oh's Intensive Care Manual (5th ed) London: Butterworth Heinemann 2003.
-
Macnab a, Macrae D, Henning R (eds): Care of the critically ill child. London: Churchill Livingstone 1999.