Introduction
As a young person with oesophageal atresia (OA) and tracheo-oesophageal fistula (TOF) your ongoing care is important.
As you become an adult, you will need to understand your care and monitoring needs, and you will need to transition from paediatric to adult health care.
The information in this booklet will help you learn about your condition, what surgery you had when you were a baby, and learn what problems may develop so you know when to see your doctor.
What is OA and TOF?
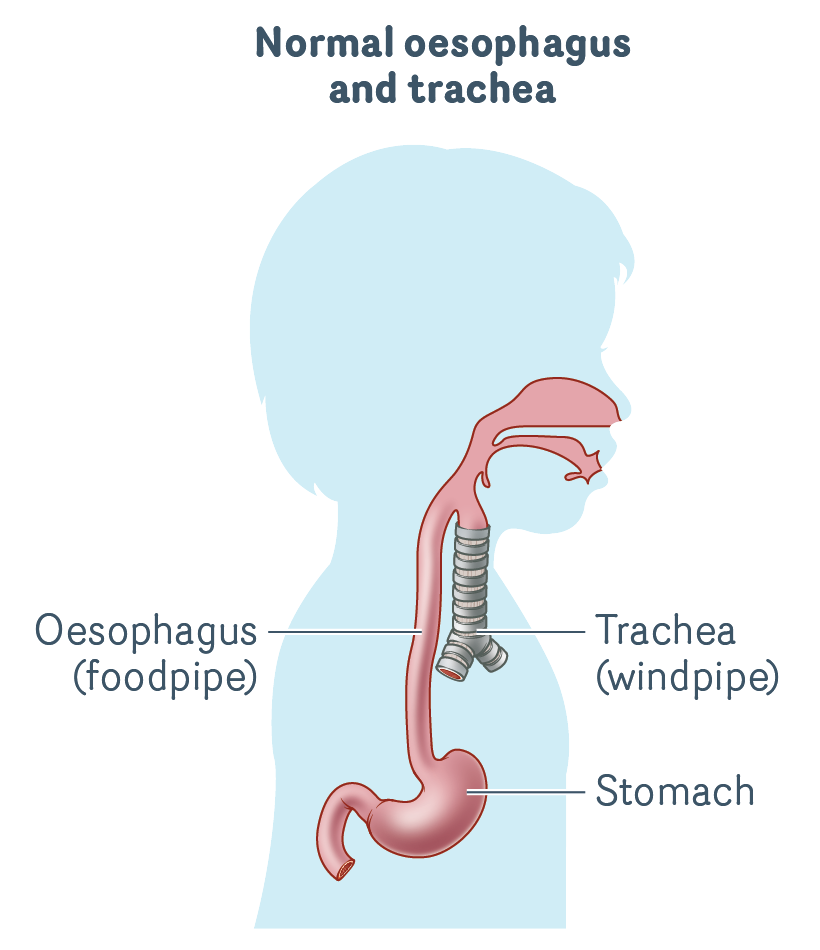
In normal development, babies are born with an oesophagus and a trachea.
The oesophagus (food pipe) is a tube that transports food, fluids and saliva from your mouth to your stomach.
The trachea (windpipe) is a tube made of cartilage that connects your larynx (voice box) to smaller tubes called bronchi which connect to your lungs. The trachea transports air in and out of your lungs as you breathe.
When you were diagnosed as a baby, you may have had a range of scans and tests to check for other problems. This is because OA/TOF is commonly associated with VACTERL association which may affect your heart, kidneys, spine and other organs.
- OA is when the upper end of the oesophagus (which normally connects to the stomach) ends in a blind pouch (atresia). It means that food and saliva cannot travel from the mouth to the stomach.
- TOF is where a fistula (abnormal connection) incorrectly joins the trachea to the oesophagus. This means anything swallowed (e.g. liquid, food, saliva) could end up in the lungs, and in some cases air breathed in can enter the stomach.
What causes OA/TOF?
It is not known what causes OA or TOF, but they usually occur together. In some cases, OA or TOF occur on their own without the other.
Sometimes OA/TOF is diagnosed before birth, but it is more commonly diagnosed soon after a baby is born.
Types of OA/TOF
There are five main types of OA/TOF. It is important you understand your condition when it’s time for you to move to adult health care – this will help you understand any problems that develop. You need to know:
- what type of OA/TOF you were born with
- what surgery you had.
If you are unsure what type of OA/TOF you were born with, your parents, carers or medical team will be able to provide you with this information.
More common types
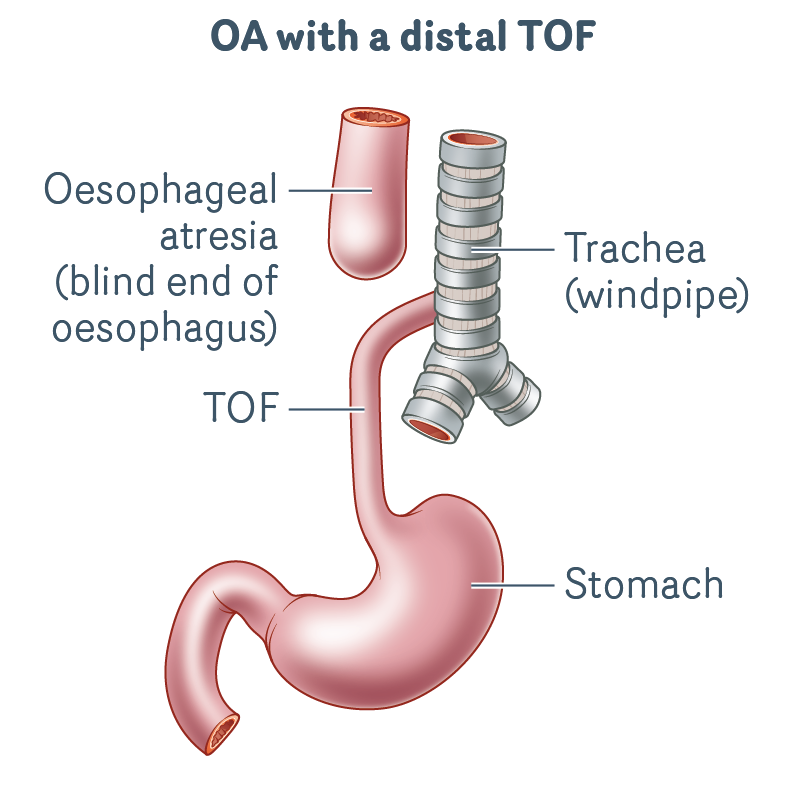
OA with a distal TOF
- This is the most common type of OA/TOF.
- The upper oesophagus ends in a blind pouch.
- There is an abnormal connection (TOF) between the windpipe and lower oesophagus.
- There is no connection from the upper oesophagus to the stomach.
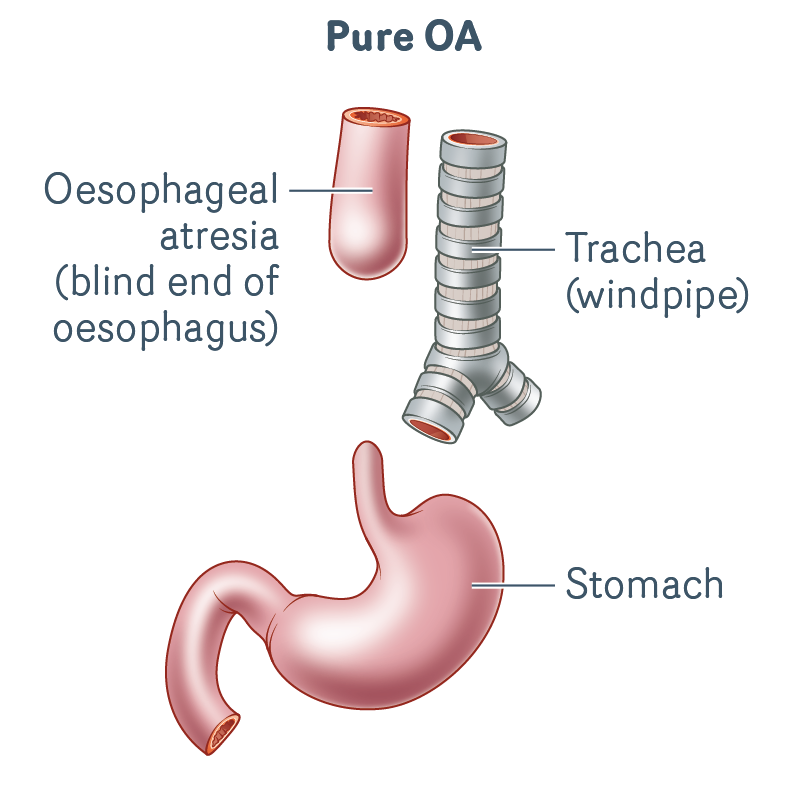
Pure OA
- The upper oesophagus ends in a blind pouch.
- There is no connection from the upper oesophagus to the stomach.
- There is no TOF (no abnormal connection between oesophagus and trachea).
- There is a long gap between the ends of the oesophagus.
Less common types
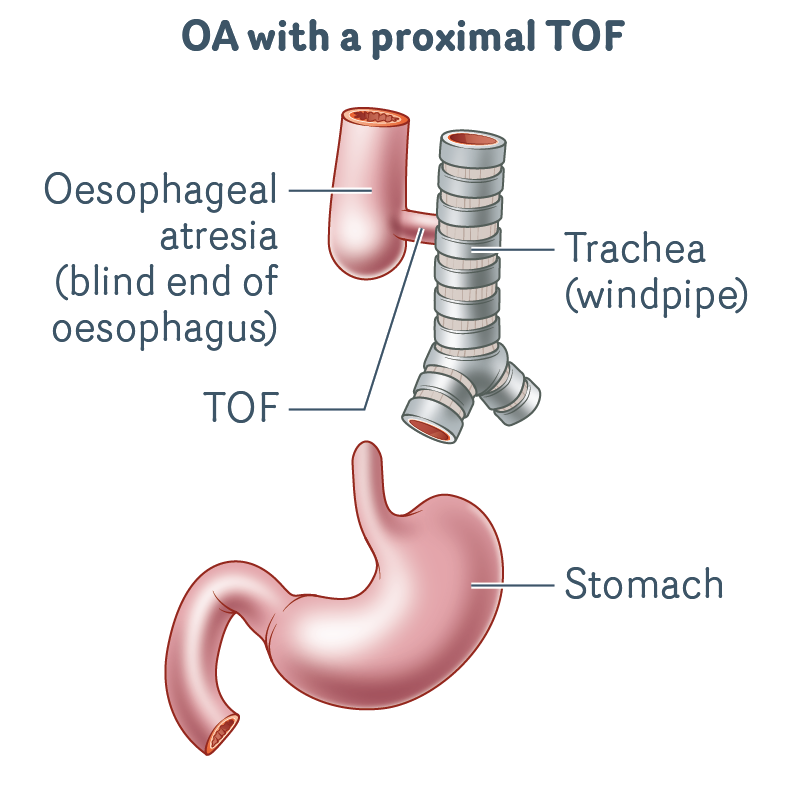
OA with a proximal TOF
- The upper oesophagus ends in a blind pouch.
- There is an abnormal connection (TOF) between the windpipe and upper oesophagus.
- There is no connection from the upper oesophagus to the stomach.
- There is a long gap between the ends of the oesophagus.
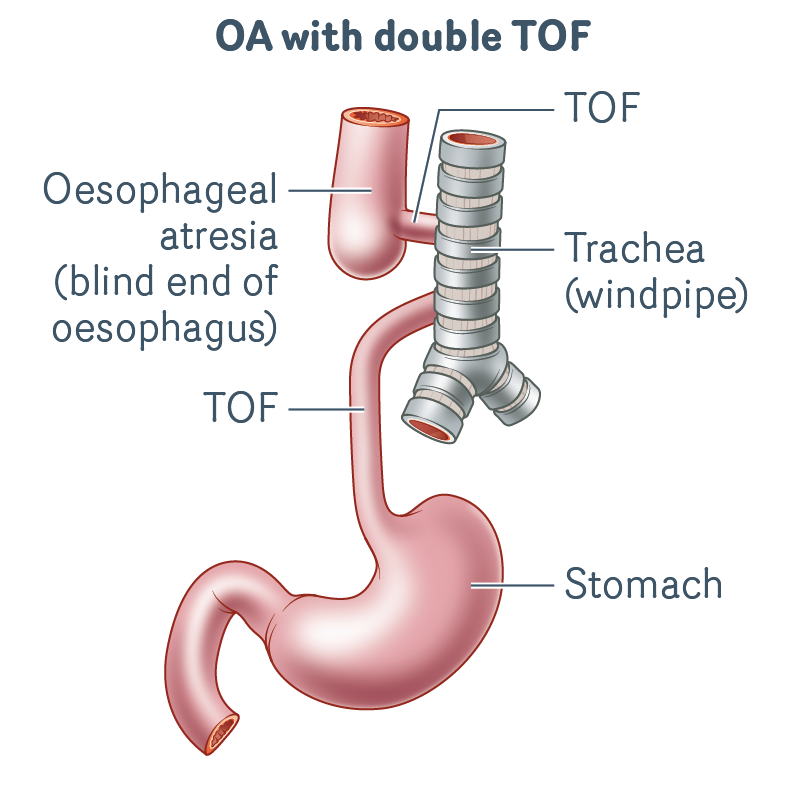
OA with double TOF
- The upper oesophagus ends in a blind pouch.
- There is an abnormal connection (TOF) from both the upper and lower oesophagus to windpipe.
- There is no connection from the upper oesophagus to the stomach.
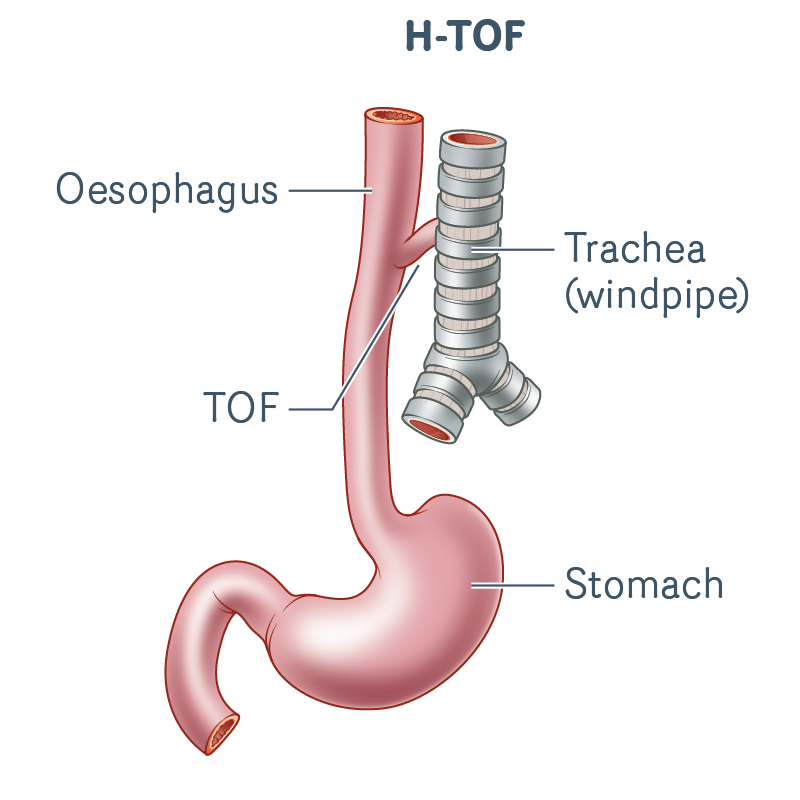
H-TOF
- The oesophagus has developed normally and connects to the stomach (there is no blind pouch).
- There is an abnormal connection (TOF) between the oesophagus and windpipe.
Surgery for OA/TOF
Surgery performed to repair OA/TOF depends on the type of OA/TOF you had. You may have one or more operations, and most of your surgery would have happened when you were a baby.
If you are unsure what type of surgery you had, your parents, carers or medical team will be able to provide you with this information.
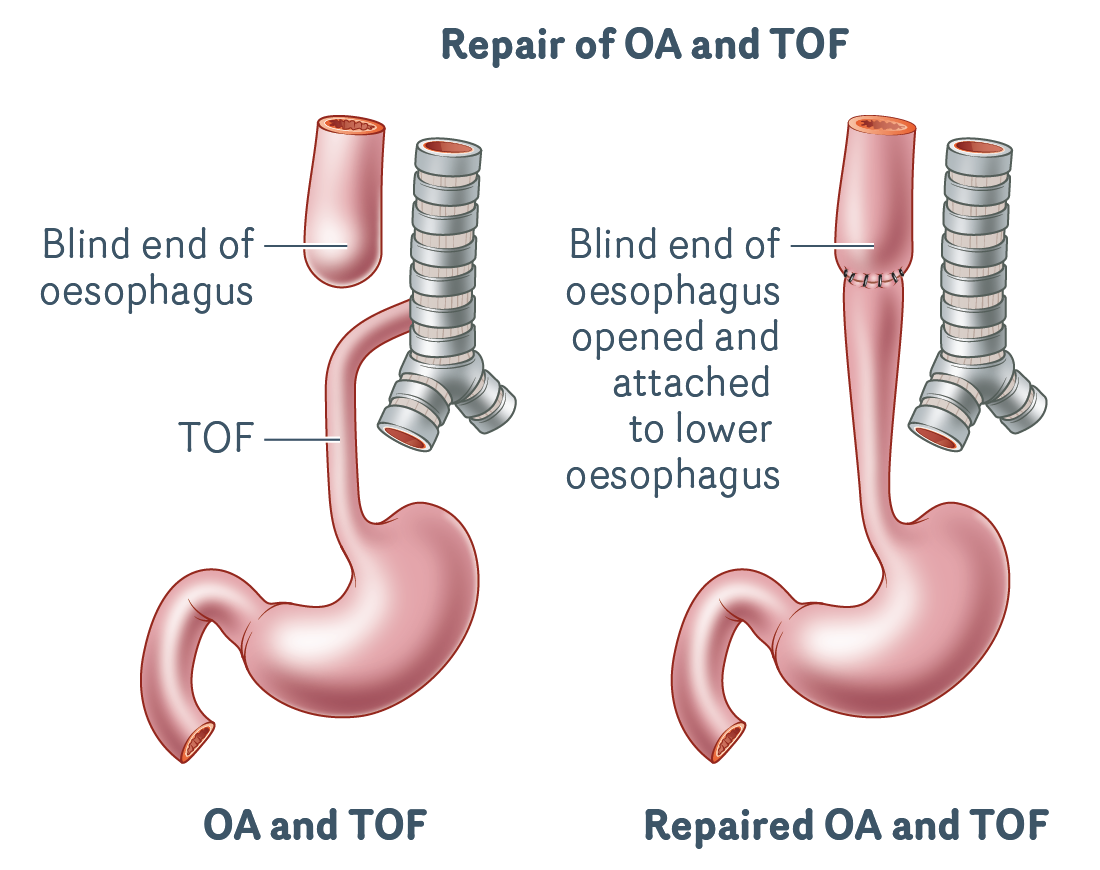
OA/TOF repair
OA/TOF can only be repaired with surgery. The surgery is usually done in babies when they are only a few days old.
OA/TOF surgery involves the following two procedures, which are usually done through a cut between the fourth and fifth ribs on the right side of the chest (called a thoracotomy):
- TOF Repair: where the connection (fistula) between the oesophagus and trachea is disconnected from the trachea and the trachea is closed off with stitches.
- Oesophageal anastomosis: when the blind oesophageal pouch is opened up and the two ends of the oesophagus are joined together with stitches.
H-TOF repair
The surgery to repair H-TOF is slightly different to an OA/TOF repair because the oesophagus has developed normally and does not need to be repaired.
- H-TOF repair: a cut is made in your neck rather than your chest and the connection (fistula) between your oesophagus and trachea is closed off with stitches.
Long-gap OA surgery
A long-gap OA is when the space between the upper and lower oesophagus is too large to repair straight away. A long gap often occurs in babies with pure OA, OA with a proximal TOF, and sometimes with OA and distal TOF.
Babies born with long-gap OA spend a much longer time in hospital. Long-gap OA often requires more than one surgery over a period of time (usually a few months) to completely repair the oesophagus. The complete repair of the oesophagus is often done in the first few months of life.
Babies born with long-gap OA may need one or more of the following surgeries:
- Gastrostomy: a tube placed into the stomach through the abdominal wall. Babies with long-gap OA have their feeds given through their gastrostomy tube until they can take all their feeds by mouth following repair of their oesophagus.
- Traction sutures: stitches put on the ends of the upper and lower oesophagus to help pull the ends closer together. If traction sutures are needed, the oesophagus is repaired later in a separate surgery.
- TOF repair: is needed in babies who have a TOF. The connection (fistula) between the oesophagus and trachea is closed off with stitches.
- Oesophageal anastomosis: when the blind oesophageal pouch is opened up and the two ends of the oesophagus are joined together. This surgery is delayed in babies with long-gap OA.
- Oesophagostomy: where the upper oesophagus is brought up and out of the neck, so saliva can drain. This procedure is uncommon. If an oesophagostomy is needed, an oesophageal replacement procedure is done later to repair the OA, and the oesophagostomy is reversed.
- Oesophageal replacement procedure: where a tube is created using other parts of the stomach or bowel. This tube can then be joined to the oesophagus and stomach to repair the oesophagus.
There are a few options for an oesophageal replacement procedure:
- Reverse gastric tube: Part of the side of the stomach (called the greater curvature) is used to form a tube. This tube is connected to the upper oesophagus.
- Colon interposition: A piece of colon (large bowel) is used to join your upper oesophagus to the stomach.
- Jejunal interposition: A piece of jejunum or small bowel is used to join the upper oesophagus to the stomach.
- Gastric transposition: The stomach is moved up higher into the chest so it is closer to the upper oesophagus and can be joined together.
Transition to adult health services
If you have been treated in a paediatric hospital, you will usually go through a process called ‘transition’ that helps to prepare you for your move to care in an adult setting. Transition begins in your teenage years, usually around the age of 15, sometimes earlier.
There may be a transition lead who will work with you, your parents and carers, and your doctors to develop a transition plan. This transition plan will help you develop the skills (such as knowing more about your condition and gaining confidence to communicate with your care team/s) you need to independently navigate and take care of your health to the best of
your ability.
Transition is important to empower you (and your parents and carers) to have a greater sense of control over the process and to maximise your capacity to live well and to achieve your goals.
Ongoing monitoring as a teenager/adult
People who have had surgery to repair OA/TOF generally have an excellent quality of life. However, oesophageal problems can develop at any time, sometimes without symptoms. To ensure any problems are picked up and can be treated before further complications occur, it is important you have the following regular check-ups:
Gastroenterologist
Regardless of the type of OA/TOF you have, you will need life-long follow-up with a gastroenterologist (a doctor who specialises in the digestive system) for the ongoing monitoring of your oesophagus.
Gastroscopy
You will need regular gastroscopies to monitor your oesophagus for any changes. A gastroscopy is done under sedation (you are not awake for the procedure) and is a procedure where the gastroenterologist uses a small telescope-type instrument with a camera to look inside your oesophagus and stomach. These areas are examined and biopsies (small samples) of tissue may be taken for testing.
How often you need to see a gastroenterologist and have a gastroscopy depends on your age
- When you are 18–30, you should see a gastroenterologist every four years.
- When you are 30–40 years old, you need to see a gastroenterologist every three years.
- Once you are 40 or older, you should see a gastroenterologist every two years.
You will need to see your gastroenterologist more often if you develop any problems or if your doctor has asked to see you more often.
Local GP
Having a good local GP who you trust and who understands your condition is important as they can help to coordinate your care needs as an adult in the community.
Your GP plays a key role during and after your transition from paediatric care, as they can communicate with your specialists and refer you to other healthcare professionals or supports if needed.
Possible problems
After the initial surgery as a newborn, some people who have had an OA/TOF repair have ongoing or life-long problems. In some cases, problems may develop in adulthood.
Reflux
A common problem is gastro-oesophageal reflux.
Reflux is when the contents of the stomach are regurgitated (brought back up), either up the oesophagus or into the mouth.
The stomach contains acid to help digest food, so when reflux occurs the symptoms may include:
- heartburn
- regurgitation of food
- a bitter taste in the mouth
- sore throat
- dental problems
- pain
- swallowing problems
- coughing
- chest infections.
You should see your gastroenterologist if you have any symptoms of reflux.
If reflux is ongoing (chronic) and not treated, it can cause further problems such as oesophagitis, oesophageal strictures, Barrett’s oesophagus, and breathing issues.
Reflux can be treated with medicine to reduce acid in the stomach. If medicines do not help control your reflux symptoms, anti-reflux surgery may be required (fundoplication). This operation is done to strengthen the muscle in your lower oesophagus and reduce reflux. If you have already had the anti-reflux surgery as a child and have reflux symptoms, you may need to have another procedure to re-tighten or repair the initial fundoplication.
Sometimes you may have reflux with no symptoms. This is called silent reflux. Regular follow up with your GP and gastroenterologist is important in case you have silent reflux and experience no symptoms. Your doctors will be able to pick this up during your regular appointments.
Oesophagitis
Reflux of stomach acid can irritate the lining of the oesophagus causing inflammation. You will need to see a doctor if you develop any pain or have other symptoms of reflux.
Oesophageal strictures
An oesophageal stricture is a narrowing in your oesophagus. This usually occurs where the two ends of your oesophagus were joined together.
Swallowing can be difficult if the oesophagus narrows because it can slow or stop food moving down your oesophagus.
Treatment for an oesophageal stricture is to have this narrowed area stretched. This procedure is known as an oesophageal dilatation and is usually performed during a gastroscopy.
Oesophageal dilatation can be done:
- by inflating a balloon on the end of a catheter, which is passed down your oesophagus during the gastroscopy
- with flexible tubes of increasing size to stretch the area of narrowing.
Oesophageal dilatations are common. Some people with OA/TOF may have had many dilatations as a child and into adulthood following the repair of their OA/TOF. Others may only need a few, and some may not need any.
Barrett’s oesophagus
Chronic reflux can cause a permanent change in the cells that line the oesophagus – this is called Barrett’s oesophagus.
Barrett’s oesophagus is a pre-cancerous change in the cells of the oesophagus. It is important to continue regular appointments with a gastroenterologist so that any changes can be detected early.
If you are diagnosed with Barrett’s oesophagus, you may need more treatment for reflux and more frequent gastroscopies, so your oesophagus can be monitored for any further changes.
Oesophageal cancer
The risk of developing oesophageal cancer later in life is low, however it is more common in people with OA than in the general population.
Two types of oesophageal cancer have been reported in a very small number of patients with repaired OA: adenocarcinoma and squamous cell carcinoma.
It is important to continue regular appointments with your gastroenterologist, so any changes in your oesophagus can be monitored.
Breathing problems
Common breathing problems may include:
- TOF cough – a loud, brassy type cough that may happen if you have tracheomalacia (floppy trachea)
- chronic cough
- pneumonia (lung infection)
- bronchitis – inflammation of the bronchi (main airways that lead to the lungs)
- asthma – this can affect your airways at times, making it harder to breathe in and out.
If you have any breathing problems, you should see your GP as soon as possible or call an ambulance in an emergency.
Swallowing problems
If you have swallowing problems (dysphagia), you may experience food getting stuck when you swallow.
There are two main reasons you may have problems with swallowing:
- Oesophageal strictures
- Problems with motility – normally, muscles in the oesophagus move food and fluid down to the stomach in a wave-like movement called peristalsis. The peristalsis of your oesophagus might not work well, and you may experience this as difficulty swallowing or food getting stuck.
If you have swallowing problems, you can try having a drink with meals to help move the food down. It is important to be reviewed by your gastroenterologist if you have any swallowing problems.
Staying healthy
Anyone who has had an OA/TOF repair should maintain a healthy lifestyle into adulthood, including eating a healthy diet, exercising regularly and avoiding smoking or use of illicit drugs.
If you choose to drink alcohol, be aware it may cause increased problems with acid reflux. You may need to be more careful than your friends in order to drink safely and responsibly for your health.
Summary of information
- Oesophageal atresia (OA) is when the oesophagus does not connect to the stomach.
- A tracheo-oesophageal fistula (TOF) is when there is an abnormal connection between the trachea (windpipe) and the oesophagus (food pipe).
- OA/TOF needs to be repaired with surgery, which usually occurs in the first few days of life.
- If you were born with long-gap OA, your oesophagus was usually completely repaired in the first few months of life.
- Anyone who has had an OA/TOF will need to be monitored by a gastroenterologist every few years, even if they have no problems after surgery.
- You will need regular gastroscopies to check your oesophagus for any changes.
- Your follow-up needs to be lifelong.
- Common problems include reflux, breathing and swallowing problems – see your doctor if you experience any of these.
- It’s important to maintain a healthy lifestyle into adulthood.