Table of contents will be automatically generated here...
You probably thought that arthritis only happens to old people. And now the doctor says you have Juvenile Idiopathic Arthritis (JIA)! You probably have lots of questions. This handout will give you some answers. But you'll probably need to talk to your
rheumatologist, rheumatology nurse educator and your parents as well. You may need to hear the answers several times. That's OK.
This is about Juvenile Idiopathic Arthritis. What causes it? How is it treated? What does it mean for you?
Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) is arthritis that young people get.
- Juvenile means young people
- Idiopathic means that we don't know what the cause is
- Arthritis is when a joint swells up, is stiff and hurts (gets inflamed).
JIA is a chronic condition
- Chronic means it lasts for a while - more than 6 weeks
- Chronic also means that treatment will make you feel better but won't cure JIA.
What are the symptoms and signs of JIA?
JIA can appear in many different ways. It mostly causes inflammation in joints and surrounding tissues.
Symptoms and signs of an inflamed joint are:
- swelling
- pain
- stiffness (especially in the morning)
- heat or warmth.
You may not have all of these symptoms in every joint that is inflamed. Sometimes the eyes can also be inflamed which is called "uveitis" (more about this later).
Other much less common symptoms of JIA can be:
- fever
- rash
- loss of appetite
- loss of weight.
How common is JIA?
JIA affects at least one young person in every 1,000 in Australia. There are at least 5,000 young people in Australia with JIA.
What causes JIA?
Your body has an immune system which fights germs from outside the body to keep you healthy. Sometimes the body's immune system mistakes a normal part of the body for something foreign (like a germ), and starts attacking the body itself. In JIA the immune
system attacks the joints. This is called an auto-immune process. We don't understand exactly how or why this happens.
Things that do not cause JIA
-
You didn't catch JIA from someone else (and you can't give JIA to another person)
-
There is nothing that anyone did or didn't do that caused your JIA
-
JIA is not caused by being too cold or living in a cold place
-
JIA is not caused by eating particular foods
-
You didn't get JIA from your parents (it is not hereditary).
What happens to the joints in JIA?
Your body has many joints. Your leg has joints in the hip, knee, ankle, foot and toes. The joints in your arm are at the shoulder, elbow, wrist, hands and fingers. There are also joints in your jaw, neck and back.
Joints are where two bones are connected. The ends of the bones have a smooth covering called cartilage. A joint is in a kind of bag called a capsule. The inside of the bag has a special lining (synovial membrane) that makes a fluid. The fluid lets the bones
move easily - like oil on your bike chain. It also protects the joint.
In arthritis, the lining of the joint becomes inflamed and thicker than normal, the capsule fills up with inflammatory cells, and the amount of synovial fluid increases. This is what makes joints swollen, stiff, hot and sore. If the inflammation is not
treated, it can damage the joint, the cartilage and the surrounding bone. Muscles around the joint can become weak and the joint may not be able to move as much as usual.
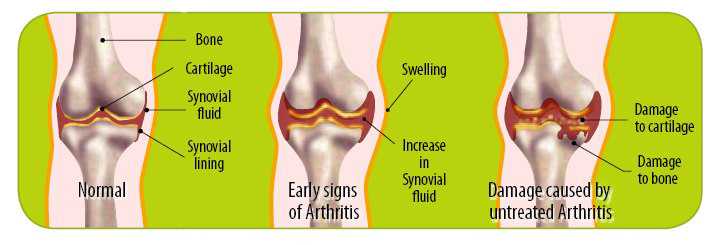
On the left is a joint without arthritis. The middle knee shows an inflamed joint and the one to the right shows a joint with untreated arthritis
How does your doctor know you have JIA?
There is no test for JIA and it can take a while for your doctor to be sure you have JIA. Sore joints can happen with other illnesses. Your doctor may have to rule out other things that can sometimes cause sore or swollen joints. Your doctor will ask many
questions about your health and will examine you, looking for inflammation in all joints. Your doctor may ask for some of the following tests to done.
-
Blood tests to measure the amount of inflammation in your body and your general health.
-
X-rays to look at bones and joints, and sometimes your lungs and heart.
-
Bone scan to look for inflammation in your body.
-
Electrocardiograph (ECG) to check how your heart is working.
-
Bone marrow aspirate to check for blood problems that can sometimes cause sore joints.
What are the different types of JIA?
What is uveitis?
Uveitis is inflammation of parts of the eye, including the iris (the coloured bit of the eye) and the muscles and tissues that focus the eye. It sometimes happens with JIA. The inflammation is caused by an auto-immune process, just like inflammation in your
joints. It doesn't hurt, and you and your doctor can't tell if there is inflammation just by looking at the eye. However if uveitis is not treated it can make your vision blurry. It is very important that you have regular check-ups with an ophthalmologist
(specialist eye doctor) to check if there is inflammation in your eyes.
What is it like to live with JIA?
The symptoms of JIA change over time, sometimes even day to day. You may have times where you feel much better, and then times when you notice more symptoms and feel more tired, stiff or sore. This is called a 'flare' or 'flare-up'. Flare-ups can sometimes be
triggered by an infection, but mostly seem to happen for no reason. If you have a flare-up, you might need to change treatments for a short time, until the JIA is back under control.
Just as your physical well-being can change over time, there are likely to be times when you feel upset about the effect JIA has on your life. It is important that you talk about these feelings with your friends, family and treatment team, so you can be supported
and learn to live well with JIA.
How is JIA treated?
Your treatment is planned just for you - it may be different for another person.
Treatment for JIA might include:
-
medications to control the inflammation
-
exercises to keeping the joints moving well
-
splints to support the joints
-
joint injections to reduce inflammation in particular joints
-
pain management strategies to reduce pain and to help you cope with pain.
You will need treatment for as long as the JIA continues. Treatment may change as the JIA changes over time, but treatment is only stopped completely when the symptoms have been gone for quite a while.
Your treatment may involve a few different professionals. They are called your treatment team.
1993 World Champion surfer Pauline Menczer is a long term arthritis suferer and has risen to the top in a physically demanding sport.
Who is my treatment team?
You and your parents
You and your parents are the most important people in the treatment team. Your team will work together to help you manage your JIA. You should ask about the treatments and how they work, so you can use them properly and help your team to help you.
Paediatric rheumatologist
Paediatric rheumatologists are doctors who look after children with arthritis.
Rheumatology nurse
Rheumatology nurses provide education, support and coordinate your treatment.
Physiotherapist (physio)
Physiotherapists are experts in how joints and muscles work. They might give you exercises to help keep joints moving well, and to keep you strong.
Occupational therapist (OT)
Occupational Therapists can give you splints for supporting joints and provide other aids to help you with everyday activities like getting dressed or writing.
Ophthalmologist
Ophthalmologists are doctors who specialise in eye problems.
Psychologist / Psychiatrist
/ Counsellor
Psychologists and psychiatrists help kids and families manage feelings about JIA, and can also help you learn to manage pain.
General practitioner (GP)
Your GP looks after your general health. Contact your GP if you have any health concerns other than joint problems.
Pharmacist
Pharmacists dispense your medication at the chemist.
Teachers
Your teachers need to know about your condition and its treatments so they can help you at school. Your nurse educator can talk to your school if you ask for this.
Support groups
It can be great to meet other kids with JIA. They understand what it's like. Local arthritis foundations often have fun activity days and camps for kids with JIA.
Meeting other families who have a child with JIA can be a valuable experience for your whole family. It can help to share ideas and experiences with other families in the same situation. Local Arthritis Foundations often run support groups for parents
and activities for families.
What's going to happen to me?
We can't say exactly how long your JIA will last. JIA can last for months or years. Sometimes the symptoms just go away on their own. This is called remission. Remission may last for months, years, or forever. About half of children with JIA go into
remission before they are adults.
Even if JIA continues, it doesn't stop most young people growing up to have active and enjoyable lives. With treatment, most JIA can be controlled and good physical function maintained.
JIA may be a challenge for you and your family, and there will be ups and downs. However, your rheumatology team will provide you with treatments, support and strategies to help you live a full and active life.