Introduction
Clean Intermittent Catheterisation (CIC) is a method of draining urine via a catheter inserted into the urethra, past the sphincter into the bladder. Once the urine is drained the catheter is removed. CIC is vital in reducing bladder pressure or draining residual urine, and therefore preserving kidney health. Correctly performed, CIC can also reduce the risk of urinary tract infections (UTIs) and promote continence.
This guideline does not refer to children and adolescents with an acute short term requirement for bladder emptying such as post-operative urinary retention, or need for an indwelling urinary catheter. Please refer to the Indwelling Urinary Catheter Guideline:
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Indwelling_urinary_catheter_insertion_and_ongoing_care/
This guideline does not refer to the child or adolescent using CIC through a stoma such as a Mitrofanoff.
Aim
To provide information that will assist nursing staff to educate and support parents and carers of children who require ongoing CIC.
Definition of Terms
- Aseptic technique: aims to prevent pathogenic microorganisms in sufficient quantity to cause infection, from being introduced to susceptible sites by hands, surfaces and equipment. Therefore, unlike sterile techniques, aseptic techniques are possible and can be achieved in
typical hospital and community settings.
- Clean Intermittent Catheterisation (CIC): Refers to the act of draining urine by passing a catheter through the urethra, past the sphincter into the bladder. The catheter is removed after the urine has been drained. This process is performed using a clean technique. A new sterile catheter is
used for each episode.
- Clean Intermittent Self Catheterisation
(CISC): Performing CIC for oneself.
- Clean: The process of performing a procedure under clean conditions to reduce the number of microorganisms. This includes handwashing, non-sterile gloves, a clean field and clean or sterile equipment.
- Detrusor Overactivity: A condition in which there is increased activity in the detrusor muscle of the bladder, often resulting in incontinence.
- Detrusor Underactivity: A condition in which there is ineffective contraction of the detrusor muscles of the bladder resulting in an inability to empty the bladder and incontinence.
- Detrusor Sphincter Dyssynergia: Dis-coordination of the detrusor muscle of the bladder and the urethral sphincter muscles resulting urinary retention and incontinence in the context of neurological impairment.
- Dysfunctional Voiding: Dis-coordination of the detrusor muscle of the bladder and the urethral sphincter muscles resulting urinary retention and incontinence in the context of no neurological impairment.
- Haematuria: The presence of blood in the urine.
- Hydrophilic Coated Urinary Catheters: Urinary catheters which are coated, and either activated with water or pre-packed with a sterile gel or fluid reservoir.
- Mitrofanoff: A surgical procedure in which the appendix and bowel are used to create a connection between the bladder and the abdominal skin surface to allow for urinary catheterisation through a stoma.
- Myelomeningocele: A neural tube defect in which the bones of the spine do not completely form resulting in a defect in the spinal canal. This can cause lack of sensation and/or movement in the lower limbs and bladder and bowel dysfunction.
- Neurogenic Bladder: A dysfunction of the bladder due to a neurological condition.
- Sensate Urethra: The experiencing of full or partial sensation in the urethra.
- Urinary Tract Infection (UTI): An infection of the kidney ureter, bladder and/or urethra.
Assessment
This guideline applies to infants, children and adolescents who require ongoing CIC due to:
- Dysfunctional voiding such as in the case of detrusor overactivity, detrusor underactivity, detrusor sphincter dyssynergia or dysfunctional voiding.
- An ongoing condition that results in a neurogenic bladder such as myelomeningocele or congenital or acquired spinal lesions.
- Spinal Cord Injury
Physical Assessment
Patient and family assessment should include:
- The reason for CIC, including establishing past and/or ongoing urology involvement and initial CIC education given by Stomal Therapy/Continence Consultants. If
family has not had initial education in CIC please contact the urology
team for referral to the Stomal Therapy/Continence Consultants.
- The person who usually performs CICs at home, the usual routine and frequency of CIC, the equipment used
- The level of comfort with parent/child performing CIC
- The reason for hospitalisation and how this may impact ability to perform CIC
- The current fluid Intake and urine output of child
- The current discomfort/pain of child
- Any specific psychosocial considerations
Catheter type
Catheter size
Below is an approximate guide for catheter size:
| Age |
Weight (kg) |
Catheter Size (French) |
| 0-6 months |
3.5kg - 7kg |
6 |
| 1 year |
10kg |
6-8 |
| 2 years |
12kg |
8 |
| 3 years |
14kg |
8-10 |
| 5 years |
18kg |
10 |
| 6 years |
21kg |
10 |
| 8 years |
27kg |
10-12 |
| 12+years |
30+kg |
12-14 |
Positioning
Assess the preferred positioning before commencing catheterisation.
- For a baby or an infant lying supine is preferred. This position may also be preferred while a parent is learning to catheterise their child.
- If the child is older, or performs CISC, the preferred option is usually sitting on the toilet. A child who is experienced at performing CISC may still require assistance to position their legs or to find a suitable surface on which to place equipment in an unfamiliar environment.
Self-catheterisation
All children who require long term catheterisation should be considered for education in CISC. Readiness to learn CISC should consider the following:
- Age: generally children can perform parts of the procedure from age 4 or 5 years but are not independent in CISC until age 6-8 years or older
- Cognitive level
- Physical dexterity
- Level of urethral sensation: many children with neurogenic bladder have little or no urethral sensation. Children with sensate urethras may have increased anxiety about pain or discomfort
- Anxiety level
- Motivation to perform CISC
Management
Equipment
needed:
- Catheter of appropriate size
- Alcohol and scent free wipes
- Water soluble lubricated gel (unless using a hydrophilic catheter)
- Container into which to drain urine (unless draining into toilet)
- Alcohol based hand rub to use, if there is no facility to wash hands adequately with soap and water
- Latex-free gloves (child and parents performing CIC may choose not to wear gloves)
- Xylocaine gel if used for children with a sensate urethra
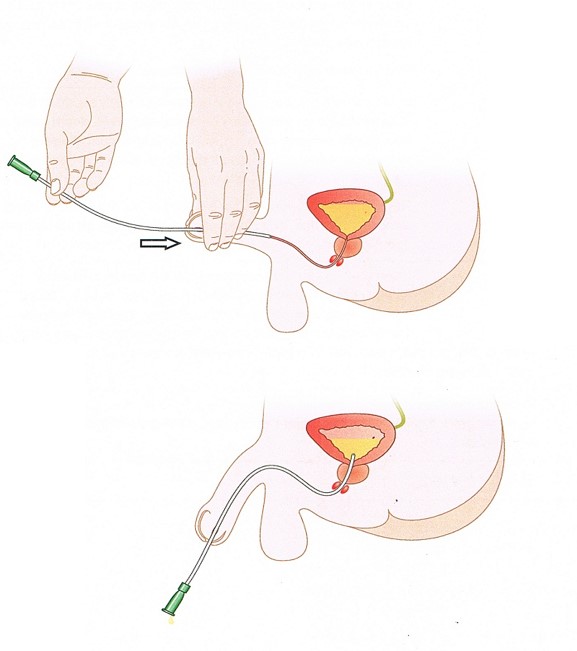
Parent/carer
directions for catheterising boys:
- Ensure the child is comfortably positioned.
- Perform hand hygiene.
- Open catheter package half way, being careful not to touch catheter tip. Place lubricant gel on the inside of open packet. Put on gloves where appropriate.
- Gently pull back child’s foreskin if he has one. You will be able to see the urethral opening. Hold penis pointing towards stomach.
- Wash tip of penis starting at urethral opening and work outwards in a circular motion with an alcohol-free wipe.
- Lubricate the tip of the catheter with the water -soluble lubricating gel or xylocaine gel.
- Slide the catheter slowly into the opening of the urethra until urine starts to flow. If resistance is felt, stop for a few seconds then continue.
- Once urine starts to flow, point the penis and catheter downwards draining into a container or toilet. Pull the foreskin gently back over the penis.
- When urine flow stops, withdraw the catheter slowly. It may start to drain again. Wait until this cease again, then remove the catheter. This ensures complete bladder emptying.
- The catheter should be discarded into the waste bin
- Remove gloves if worn and perform hand hygiene
- Document procedure in EMR as relevant.
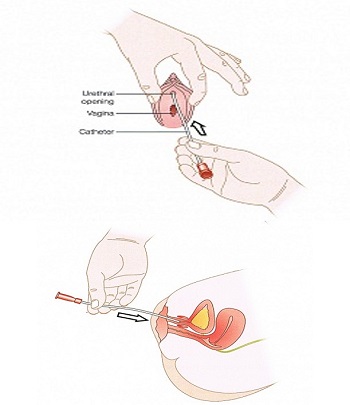
Parent/carer
directions for catheterising girls:
- Ensure the child is comfortably positioned.
- Perform hand hygiene
- Open catheter package half way, being careful not to touch catheter tip. Place lubricant gel on the inside of open packet. Put on gloves where appropriate.
- Gently separate the labia with one hand and wash down from top to bottom using an alcohol-free wipe and discard. Repeat with a clean wipe.
- Lubricate the tip of the catheter with the water- soluble lubricating gel/xylocaine gel and gently slide catheter tip into the urethra. If resistance is felt gently rotate the catheter a little. Once urine is flowing push catheter in a few
more centimetres to ensure that it is in the bladder.
- When urine flow stops, withdraw the catheter slowly. It may start to drain again. Wait until this cease again, then remove the catheter. This ensures complete bladder emptying.
- The catheter should be discarded into the waste bin
- Remove gloves if worn, and perform hand hygiene
- Document procedure in EMR as relevant.
Potential
complications:
| Complications |
Signs and Symptoms |
Prevention and management |
| Urinary tract infection (UTI) |
http://www.rch.org.au/clinicalguide/guideline_index/Urinary_Tract_Infection/
Children who perform CIC may notice increased leaking of urine between catheterization |
http://www.rch.org.au/clinicalguide/guideline_index/Urinary_Tract_Infection/
Children May need to perform more frequent catheterization until symptoms of the UTI clear.
If a child performing CIC has repeated UTIs, careful assessment of catheterization technique is recommended. Observation of technique is more accurate than parent or child recall |
| Urethral trauma |
Pain on passing the catheter (for children with sensate urethra)
Hematuria
Chronic UTI’s
Inability to pass a catheter |
Seek advice from the Stomal Therapy/Continence Consultants or the Urology Team
For mild trauma-consideration of the use of hydrophilic catheters
For severe trauma- the treating team may consider surgical options such as dilatation of the urethra or a surgical urinary stoma formation, such as a Mitrofanoff |
| Catheter obstruction |
Difficulty or inability to pass a catheter |
Can be due to muscle spasm, do not force the catheter. Wait a minute or two to allow spasm to pass
Assess anxiety of child- anxiety can increase muscle spasm that prevents catheter passing smoothly- utilize deep breathing, visualization or distraction techniques
If catheter unable to be passed, contact the Stomal Therapy/Continence Consultants or the Urology team |
Special Considerations
Psychosocial
Considerations:
- Families can find CIC an emotionally difficult procedure when it is first introduced. If a child has significant anxiety do not force the process.
- Consider assistance from Child life therapy in preparing the child and during the procedure.
- Allowing children to handle equipment, hold the catheter, clean themselves or assist in placing the catheter, even from the first catheterisation, can give them a sense of control.
- Use of diagrams and models can be helpful. Some children find the use of mirrors very confronting
- Ongoing anxieties for children who perform CICs regularly, include leakage, pain and peers finding out.
- Children who are proficient in CICs can still require assistance if in an unfamiliar bathroom or toilet, particularly with positioning. Most children who are independent performing CICs do not want others to perform it for them.
Other:
- On discharge assess if the family need extra support with CICs due to any change in physical status – refer to HITH/PAC
- If there are any concerns with the family’s level of knowledge or ability to manage CIC please contact the Stomal Therapy/Continence Consultants.
Companion Documents
Links
Evidence Table
Click here for the
Evidence Table for this guideline.
Please remember to read the
disclaimer.
The revision of this nursing guideline was coordinated by Carmen Akaoui, Stomal Therapy, and approved by the Nursing Clinical Effectiveness Committee. Updated February 2023.