Introduction
A Replogle tube is used in the management of infants with long-gap oesophageal atresia awaiting a delayed repair of their oesophagus. Infants with long-gap oesophageal atresia may wait up to 3 months until surgical repair of the oesophagus.
A Replogle tube is used to continuously drain saliva from the upper oesophageal pouch and is positioned 0.5-1cm above the end of the oesophageal pouch. Adequate drainage of the upper oesophageal pouch is essential to prevent saliva spilling over into
the trachea resulting in aspiration.
Aim
To outline the principles of management of infants with a Replogle tube in-situ at The Royal Children’s Hospital.
Definition of Terms
- Long-gap oesophageal atresia: Variants of OA with a large gap (wider than ~4cm between the two ends of the oesophagus). This includes pure OA and OA with a proximal TOF.
- Oesophageal atresia (OA): A congenital anomaly in which the oesophagus ends in a blind upper pouch.
- Replogle tube: A double lumen tube which is placed into the oesophageal pouch and connected to continuous low-pressure suction (-20 to -35 cmH2O), allowing the pouch to be kept clear of saliva and secretions which can spill into
the lungs.
- Securement of Replogle tube: taping similar to securement used for ETT, or use of NEOfitTM
- Tracheo-oesophageal fistula (TOF): an abnormal connection between the trachea and oesophagus.
- Traction suture techniques: involves the placement of sutures under tension in the upper and lower ends of the oesophagus. The infant will return to theatre after approximately 4-8 weeks for a delayed repair of the oesophageal atresia
if the oesophageal ends are approximated.

Figure 1. Long gap OA (without TOF)
|

Figure 2. Long gap OA (with TOF) |

Figure 3. Long gap OA with proximal TOF |
Diagrams sourced from Royal Children's Hospital, Melbourne
Assessment
All patients with an unrepaired OA should be on continuous cardiorespiratory monitoring due to the high risk of aspiration.
Suitability of a Replogle Tube:
- Infants who have been assessed to have a long-gap OA and awaiting a delayed repair of their oesophagus
- Infants who have not had their TOF/OA repaired but are deemed appropriate for Replogle insertion with Air flushes only (due to the aspiration risk with unrepaired proximal TOF) until surgery can be attended
An order within the EMR Orders tab is required to
- initiate use of a Replogle tube
- record the length of Replogle tube insertion
- determine the negative pressure set on the UWSD unit
- discontinue treatment with a Replogle tube
Management
Size of the Replogle tube:
- For infants > 32 weeks' gestation use a size 10Fr Replogle tube inserted into a nare if possible.
- For infants
<1500 grams, discuss the suitability of Replogle tube with the Surgeon.
- If resistance is observed when inserting into the nare, place the tube into the mouth and secure
Initial measurement of and insertion of a Replogle tube should be carried out by the Surgical Registrar.
- A lubricated Replogle tube is then inserted to ~0.5cm above the end of the oesophageal pouch as per the procedure below
- The measured length of the Replogle tube and the length of the oesophageal pouch (from nares or lips) is documented in the EMR on the Replogle Tube Care Order and LDA Assessment in Flowsheets.
- The length of Replogle tube insertion should also be documented on the suction card on the infant’s cot.
Subsequent measurement of the oesophageal pouch should be undertaken every 2-4 weeks (or sooner if indicated) by the Surgical Registrar or the Oesophageal Atresia Nurse, and Replogle tube length documented as above.
Prior to insertion or changing of a Replogle tube:
- Check the Replogle Tube Care Order for depth of Replogle tube insertion, suction pressure and specific requirements for each infant i.e.. flush requirements, air or 0.9% Saline
- Ensure adequate settling and comfort measures are in place to minimise trauma to the patient
Equipment
- ArgyleTM Replogle Suction Catheter size 10Fr & additional spare tube at patient bedside
- "Atrium"Oasis Dry (UWSD) Unit 2000ml
- Hi-flow, low vacuum suction regulator unit (blue and white suction regulator)
- Suction tubing (long length)
- 10 mL Luerlock syringe with plunger removed
- 10 mL syringe of sodium chloride 0.9% (labelled)
- NEOfitTM endotracheal tube holder
- Suction catheters (8Fr, 10Fr) for additional intermittent oesophageal pouch suction
- Additional suction regulator unit for intermittent oesophageal pouch suction
- Monitoring equipment for cardiorespiratory & SpO2 continuous monitoring
- NeopuffTM at patient bedside that has been checked and ready to use
Process for Insertion
- Nurse infant with head of bed elevated 30-45 degrees.
- Ensure water seal is filled to 2cm line as per instructions
- Connect suction regulator to suction outlet on wall, and turn on the wall suction to -80mmHg pressure
- Attach suction tubing to “Atrium” UWSD unit
- Set suction control dial on Atrium to -20cmH2O (or recommended pressure as per Surgeon or Oesophageal Atresia nurse)
- Suction can be increased on “Atrium” following discussion with Surgeon, Neonatal Consultant or Oesophageal Atresia Nurse and updated order.
- Flush and aspirate the Replogle tube with sodium chloride 0.9% to pre-lubricate the Replogle tube prior to insertion.
- Measure required length of insertion on Replogle and mark with a piece of Leukoplast placed circumferentially
- Apply lubricant to tip of Replogle ensure patency of lumen holes
- Gently insert the Replogle tube to predetermined length via nares or mouth as indicated observing for signs of physiological instability.
- Secure Replogle tube with the NEOfit tube holder by wrapping snuggly around the Replogle tube (see Figure 4 below).
- Connect a 3-way tap with a 2 x 10mL luer lock syringes to the vent lumen of the Replogle (the blue, smaller lumen).
- Connect the Replogle tube to the Atrium Dry Suction Underwater seal drain (UWSD) tubing
- Ensure suction pressures remain at -80mmHg on the wall suction unit and as ordered on the Atrium Dry Suction dial
- Perform hand hygiene at the end of the procedure.

Figure 4. Steps on how to secure an orally inserted Replogle tube, secured with NEOfitTM.
Photograph property of The Royal Children’s Hospital.
If there is any acute respiratory distress, compromise or if there is any resistance during insertion of the Replogle tube, remove the tube immediately and seek medical assistance.

Figure 5. Photo depicting Replogle atrium uwsd.
Photograph property of The Royal Children’s Hospital.
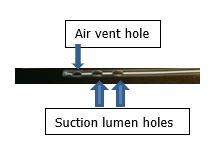
Figure 6. Photo depicting of the holes in the tip of the Replogle tube (inserted into the patient’s oesophageal pouch via the nares or mouth).
Photograph property of The Royal Children’s Hospital.
Ongoing Management
Flush the suction lumen of the Replogle tube every 2 hours, as required with 1-2mL sodium chloride 0.9%. This is done by gently aspirating the suction lumen of the Replogle tube with a 5mL luer slip syringe, then flush with 1-2mL sodium chloride
0.9% and gently aspirate the 1-2mL sodium chloride 0.9% back from the oesophageal pouch. This is to prevent the suction lumen from blocking with secretions. See Figure 7 below for images of gentle aspiration & flushing of the suction lumen.
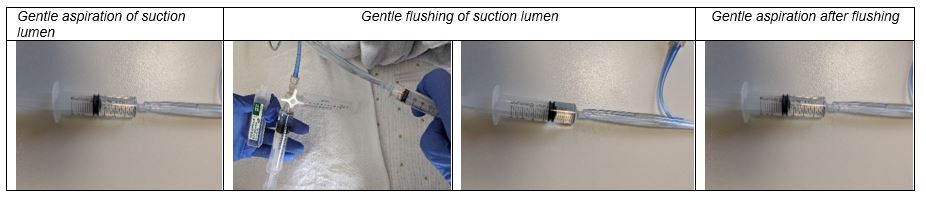
Figure 7. Aspiration and flushing of the Replogle tube suction lumen.
Photograph property of The Royal Children’s Hospital.
Documentation
Document site assessment, securement method and patency of vent lumen and vent lumen intervention, patency of drainage lumen, and drainage lumen interventions in the LDA EMR tab.
Troubleshooting
Do not flush the Replogle tube if there are immediate concerns about the infant’s deteriorating condition, position of the Replogle tube, or secretions. Remove Replogle tube and perform intermittent oesophageal pouch suction until any issues have been
resolved.
|
Signs of Replogle tube blockage
|
Management
|
|
Fluid (sodium chloride 0.9%) running out into the air vent syringe barrel this may indicate the Replogle tube is obstructed.
|
Remove excess saline from vent lumen and gently inject 2-3mL AIR (not saline) into air vent lumen to help unblock.
If unsuccessful in clearing the Replogle tube, flush the suction lumen with 1- 2mlL sodium chloride 0.9% with a 5mL syringe and aspirate to return.
If unsuccessful in restoring patency, remove Replogle tube and replace with a new Replogle tube
Perform intermittent oesophageal pouch suction as required until a patent Replogle tube is in-situ and draining well.
|
|
If there is no drainage from the Replogle tube or the infant is requiring intermittent oral oesophageal pouch suction.
|
Flush Replogle tube with 1mL of air or sodium chloride 0.9% via vent lumen and check for movement of fluid through the tubing.
If no movement of fluid through the Replogle tube, gently aspirate the suction lumen with a 5mL syringe.
Gently flush the Replogle tube with 1-2mL of sodium chloride 0.9%, gently aspirating the sodium chloride 0.9% back
If no movement of fluid through the Replogle tube, or no return of sodium chloride 0.9% remove and replace with a new Replogle tube.
|
Family Centred Care
It is the responsibility of the clinician caring for the infant with a Replogle tube to ensure that the parents and caregivers understand the rationale for the intervention, as well as potential complications. Infants with Replogle tubes in situ for
an extended period of time (long gap OA) should be offered age appropriate developmental opportunities. Parents and caregivers should be encouraged to participate in all other aspects of day to day care to promote attachment and bonding. If not already
involved, refer to COCOON for ongoing developmental support.
Links
RCH Policies & Procedures:
RCH Nursing Guidelines
COCOON Parent Website
Parent support groups
Evidence Table
| Reference
|
Source of Evidence | Key
findings and considerations |
| Alberti D, Boroni G, Corasaniti L & Torri F. 2011. “Esophageal atresia: pre and post-operative management.’ Journal of Maternal-Fetal and Neonatal Medicine. 24 (S(1): 4-6. |
Systematic review |
- A 10F double-lumen Replogle tube allows the aspiration of secretions but limits the suction on the mucosa preventing ulcerations.
- Quite frequently the suction catheter becomes blocked by thick salivary secretions with a significant risk of aspiration if not recognized. Frequent irrigations with saline or infusion of 3–5cc of air are useful to prevent blockage of the Replogle tube
|
| Bairdain, S., Hamilton, T.E., Smithers, C.J., Manfredi, M., Ngo, P., & Gallagher, D., Zurakowski, D., Foker, J.E., & Jennings, R.W. (2015). Foker process for the correction of long gap esophageal atresia: Primary treatment versus secondary treatment after prior esophageal surgery. Journal of Pediatric Surgery, 50(6): 933-937. doi: 10.1016/j.jpedsurg.2015.03.010 |
RCT |
- The Foker process (FP) uses tension-induced growth for primary esophageal reconstruction in patients with long gap esophageal atresia.
|
Braithwaite, I. (2011). Continuous low suction pressure: an innovative solution to transporting patients with Replogle tubes. Infant, 7(4):132-133.
|
Editorial review |
- Design of a double lumen catheter should be used with suction pressures of -25-30mmHg, which equates to 3-4kPa or 34-40cmH20 of negative pressure.
- Use of a dry chest drain in conjunction with suction regulator provides safe, constant suction of upper oesophageal pouch
|
Cardinal Health (2020). ArgyleTM Replogle Suction Catheters. Accessed June 22, 2020, https://www.cardinalhealth.com.au/en_au/medical-products/patient-care/obstetric-and-neonatal/neonatal-care/argyle-replogle-suction-catheters.html
|
Manufacturing guideline |
- ARGYLE™ replogle suction catheters were specially designed for the neonate
- Double lumen, clear tube with three smooth eyes
- Venting action provides safe and effective drainage
- Markings on tube for depth measurement
|
Kolimarala, V., Jawaheer, G., & Reda, B. (2010). Management of the upper pouch in neonates with oesophageal atresia: National survey on use of Replogle tubes in United Kingdom (Poster). Pediatric Research, 68, 476. DOI: 10.1203/00006450-201011001-00954
|
Qualitative research study |
- Research study involving questionnaire to obtain information relating to the use of Replogle tubes in neonates with oesophageal atresia in Neonatal units in the United Kingdom
- Low flow suction was used in conjunction with Replogle tubes in 87% of cases. Guidelines on the use of Replogle tubes were available in 40% of cases. The tube was flushed in 36% of cases.
- Variable practices & methods for managing the upper pouch were noted.
|
Leeds Teaching Hospitals NHS Trust. (2018). Oesophageal atresia and trache-oesophageal fistula requiring a Replogle tube – Management of Infants with. Leeds Teaching Hospitals NHS Trust, Leeds, UK. Retrieved May 3, 2024 from http://lhp.leedsth.nhs.uk/detail.aspx?id=4008
|
Hospital guideline | - Replogle tube - 10Fg > 1500gms
- Size 8Fg Replogle <1500g, for the very premature infant.
- Documentation of secretion volume, consistency and colour
- Do not include instilled volumes of sodium chloride 0.9% within fluid balance. Sodium chloride 0.9% instilled is continuously aspirated and therefore not an intake.
|
| Royal Hospital Women (2014). Procedure Guideline: Set-up and insertion of Replogle Rube. Retrieved on 3/5/24 from Replogleset.pdf (nsw.gov.au) |
Hospital guideline | - Double lumen tube with drainage and air venting functions
- Discusses insertion of tube into oro- or naso-pharynx 0.5cm above base of oesphageal pouch
|
| Scott, JE, Hawley, A, Brooks, J-A. (2020). Delayed diagnosis in esophageal atresia and tracheoesophageal fistula. Advances in Neonatal Care. doi:10.1097/ANC.0000000000000763 |
Case study |
- Discussion of methods of oesophageal pouch suction either intermittently or by Replogle tube (10 Fr) 0.5 cm above the distal end of the esophageal pouch on continuous low pressure suction to remove saliva
|
| Southern West Midlands Maternity & Newborn Network. (2020). Neonatal Guidelines 2020: Management of Tracheo-oesophageal Atresia Retrieved May 3, 2024 from TOF/OA (bwc.nhs.uk) |
Hospital guideline |
- Recommendation of flushing Replogle tube with 0.5ml sodium chloride every 15 minutes, more frequent if oral secretions present
- If occluded after flushing, change the tube
|
Women and Newborn Health Service Neonatal Directorate. (2022). Clinical Practice Guideline: Oesophageal atresia / tracheoesophageal fistula. Government of Western Australia, North Metropolitan Health Service. Retrieved on May 3, 2024 from Oesophageal Atresia / Tracheoesophageal Fistula (health.wa.gov.au)
|
Hospital guideline | - Atrium suction control set -15cmH2O to -40cmH2O (As per medical orders)
- Vent lumen of Replogle flushed with 0.5ml sodium chloride
- Flush drainage lumen manually 2-4 hourly or more frequently if required with 1-2ml sodium chloride to maintain patency
|
The revision of this nursing guideline was coordinated by Brooke Smith, Julia McKeown and Jo Brooks, CNS, Butterfly, and approved by the Nursing Clinical Effectiveness Committee. Updated August 2024.
Please remember to read the
disclaimer.