Introduction
Comprehensive neurological assessment is essential for the early recognition and management of neurological deterioration. Delays in recognising changes in neurological status can result in permanent deficits and even death.
Aim
The aim of this clinical nursing guideline is to outline the required neurological assessment to recognise early changes or deterioration. This guideline should be used in conjunction with the Observation
and Continuous Monitoring Nursing Guideline
Definition of Terms
- Intracranial
Pressure (ICP)- Normal intracranial pressure is defined as the pressure of the combined volume of the components of the skull, being the brain tissue, blood, and cerebrospinal fluid.
- Primary Brain Injury- the immediate and irreversible injury that occurs at the time of insult. It can be both traumatic (head strike) or non-traumatic (stoke, mass or infection).
- Raised Intracranial
Pressure – the increase in the combined volume of the skull components.
- Secondary Brain injury- may occur as a consequence of the primary injury, raised ICP, hypoxia, hypotension, acidosis, or cerebral oedema.
Assessment
All hospitalised children require an assessment of consciousness (AVPU), on admission and then at minimum, with every set of vital sign observations.
Assessing the Childs level of consciousness:
AVPU (Alert/Voice/Pain/Unresponsive)
- Alert - The patient is awake
- Voice - The patient responds to verbal stimuli
- Pain - The patient responds to painful Stimuli (Trapezium squeeze/ear lobe pinch)
- Unresponsive - The patient is unresponsive to all above stimuli.
Indications for neurological observations
- Patients who require neurological observations include but are not limited to patients with:
- Proven or suspected change in intracranial pressure
- Endocrine disorders:
- Diabetic Ketoacidosis
- Diabetes Insipidus
- Recent hypoglycaemia
- Encephalopathy
- Some Metabolic disorders
- Significant liver failure
- High ammonia
- Hepatic/uraemic coma
- Meningitis
- Electrolyte instabilities
- Demyelinating neurological conditions
- Following cranial or neurosurgical procedures
- Cerebral arteriogram
- Cardiac catheters
- Brain tumour or space occupying lesion
- Extradural /subdural / intracerebral haematomas
- Hydrocephalus
- Patient with ventricular shunt, lumbar drain, or external ventricular drain
- Seizures
- of unknown origin
- Epileptic patients when postictal
- Frequent uncontrolled seizures
- Those at increased risk of stroke or bleeding
- Ventricular Assist Devices
- Altered INR
- Moya Moya disease
- Sedated patients
- Trauma- when head is involved
- Proven or suspected head injury
- Proven or suspected spinal injury (cervical)
- ANY unexplained change in status of patient's neurological function
Neurological Observations
Baseline neurological observations are part of admission for any patient with actual or potential neurological impairment. Frequency of neurological observations should then be determined by the clinical status of the patient and placed as an order.
At a minimum, neurological observations should be carried out with vital signs, 4 hourly for patients at risk of neurological decline.
Neurological Observation includes:
- Glascow Coma Scale (GCS)
- Pupil response
- Limb function
- Vital signs
Neurological assessment in young children can be challenging due to the variation of normal, psychological, and physiological development, this can be further complicated with the response to hospitalisation. Engaging parents and family members to understand
the child’s baseline will support the assessment. Parents should also be educated on the importance of undertaking neurological observations and why their child may be woken regularly for assessment.
Changes in vital signs are typically late
signs of increased intracranial pressure:
- Bradycardia can occur as a late sign of progressive increased intracranial pressure
- Bradycardia, hypertension and bradypnea are called Cushing’s Triad and indicate pressure on the medullary centre of the brain (The connection between the brainstem and the spinal cord).
Respiratory rate is also important as it provides early information about the malfunction in the medulla oblongata and the pons. Injury and/or pressure to the respiratory centre will indicate injury or pressure on the brain stem.
Altered temperature may be indicative of injury to the hypothalamus which regulates body temperature.
The Glasgow Coma Scale (GCS)
The GCS is a clinical scale to reliably measure the patient’s level of consciousness including assessment of eye opening, verbal response and motor response. The patient is assessed
and scored in each area and the scores are added together to the give the
patients final GCS score.
Any drop in GCS from the patient’s baseline should be considered a potential neurological emergency and should be escalated as per hospital policy.
It's important to appreciate that the maximum baseline GCS may vary depending on the underlying conditions or level of development. e.g. children who are non-verbal. Monitoring changes in GCS score is essential.
Eye opening
|
4
|
Patient eyes open spontaneously
|
|
3
|
Patient opens eyes to speech/touch
|
|
2
|
Patient opens eyes to pain
|
|
1
|
None
|
Children must be woken for neurological observations, and many children will require verbal stimulation or gentle touch (which then receives a score of 3). If children do not wake easily then painful stimuli should be applied, trapezius pinch for children
12months and older or ear lobe pinch to children less than 12 months old.
Verbal response
|
Score
|
Infant 0-12 months
|
Child 1-5 years
|
Child >5 years
|
|
5
|
Cries – periods of wakefulness
- Smiles and coos with interaction with staff or caregiver
|
Alert words or phrases usual ability
|
Orientated
|
|
4
|
Cries – alternating with sleep
|
Less than usual verbal ability
|
Confused
- Disoriented in conversation
|
|
3
|
Cries – deep pain only
- Persistent inappropriate crying and/or high-pitched cry
|
Cries/vocal sounds only to pain
- Persistent crying and/or scream
|
Inappropriate words
|
|
2
|
Grimace or facial movement only to pain
- Grunts, agitated, restless
|
Occasional whimpers/moans to pain
|
Vocal sounds
|
|
1
|
No facial expression to pain
|
No response
|
No response
|
Motor response
|
Score
|
Infant 0-23 months
|
Toddler 2-5 years
|
Child >5 years
|
|
6 - Obeys commands/age-appropriate movement
|
Moves spontaneously and purposefully
|
Obeys command
|
Obeys command
|
5 - Localises to stimuli
- Patient can purposefully move towards the area of painful stimuli to remove source
|
Withdraws to touch
|
Localises to pain
|
Localises to pain
|
4 - Withdraws to pain
- Patient flexes away from the area of painful stimuli with no attempt to remove source
|
Withdraws to central pain
|
Flexes in response to pain and not localises to source
|
Flexion withdrawal localising to painful stimuli but unable to remove source
|
3 - Abnormal flexion
- Shoulder adduction and wrist flexion making a fist
|
Abnormal flexion - Decorticate posturing
|
Abnormal flexion to painful stimuli - Decorticate posturing
|
Abnormal flexion to painful stimuli - Decorticate posturing
|
2 - Extensor response
- Extending limbs at the elbow adduction of the shoulder flexion, flexion of the wrist while either making a fist or extended fingers
|
Abnormal extension to pain - Decerebrate posturing
|
Abnormal extension to pain - Decerebrate posturing
|
Abnormal extension to pain - Decerebrate posturing
|
|
1 - No response
|
Decorticate posturing Decerebrate posturing
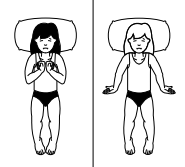
Images from the Victorian Children’s Tool for Observation and Response -Neurological Observation chart.
Assessment of limb strength
Limb muscle
strength is used to identify any asymmetry between limbs and can provide
information about the potential location of any intracranial pathological
process or dysfunction. Limb strength can be tested at the same time as motor response by observing patients' spontaneous movements, response to pain or when following motor commands.
Assessment of pupils (PEARL)
In addition to the GCS, pupillary response is also incorporated as it relays to the control and responsiveness of the third cranial nerve and maybe be an indicator of a raised intracranial pressure (ICP), brainstem damage and oculomotor nerve compression.
It is important to know the patient’s baseline (unequal pre-op, dilating drops, any abnormalities)
How to perform assessment of pupils
- Assessing pupil size, equality, and reaction.
- Check pupils in ambient light prior to assessment to observe the size of the pupil. The size of the pupil once adjusted to ambient light is the pupil size recorded.
- Instruct the patient to look forward. If unconscious, the eyelids are to be lifted to access pupils.
Using a penlight torch assess for:
- Direct constriction, move the penlight from the outer aspect of the eye, inwards. Repeat for both eyes.
- Consensual constriction, shine the light into one pupil and observe the other pupil for constriction. Repeat for both eyes
If pupils change from baseline or no pupillary constriction occurs, this may indicate a deterioration in the patient’s condition. This is potentially a neurological emergency.
Escalation of abnormal findings
If there are any clinical concerns for a patient's neurological status the RCH escalation pathway should be followed using the RCH Policies and Procedures: Medical
Emergency Response Procedure.
Other considerations
- Imaging CT/MRI
- Referral to neurology/neurosurgery for surgery +/- clot retrieval
- If clot retrieval needs to go to RMH via PIPER Family Centred Care
- Consider family and discharge education
- RCH Kid's Health Information: Head Injury
Companion Documents
Victorian
Children’s Tool for Observation and Response -Neurological
Links
Evidence Table
Coming soon.
Please remember to read the disclaimer.
This nursing guideline was developed by Kate Shepherd, CSN, Cockatoo Ward, and approved by the Nursing Clinical Effectiveness Committee. First published June 2025.