Introduction
Retinopathy of prematurity (ROP) is a disorder of the developing retina of low-birth-weight preterm infants that potentially leads to blindness in a small but significant percentage of those infants. Neonatal eye examinations are performed to monitor Retinopathy of Prematurity (ROP). Timely treatment of ROP ensures treatment is effective and reduces the risk of vision loss.
Aim
To provide guidance of nursing care for neonates undergoing an eye examination on the Butterfly Ward.
Definition of terms
Retinopathy of Prematurity (ROP): A disorder resulting in alteration of the normal retinal vascular development, affecting premature infants, which can lead to visual impairment and blindness.
Very Low Birth Weight: Birth weight
< 1500 grams.
Risk Factors
- Infants born with a very low birth weight or gestational age of 32 weeks or less
|
- Oxygen supplementation
- Anaemia
- Blood transfusion
- Intraventricular haemorrhage
- Respiratory distress syndrome
- Multiple spells of apnoea/bradycardia
- Mechanical ventilation
|
- Congenital abnormalities or structural abnormalities of the eye
- Severe eye infections
- Non-accidental injuries in infants
|
Management
Ophthalmology referral
Neonatal medical staff identify all infants at risk of ROP and make a referral to Ophthalmology. The Neonatal registrar completes the referral request form in EMR as ‘Ophthalmology Inpatient Consult’. Referrals are found in the Eye Examination Book.
If the infant is medically unstable (as determined by medical team and/or ANUM) and would not tolerate the examination at the time of consultation with the ophthalmologist, the procedure will need to be rescheduled. This is documented by the ophthalmologist in the Consultation Notes and in the Eye Appointment
Book with the reason for not being seen.
On transfer to another hospital, documentation on the discharge summary of when the next eye review is required should be clearly stated.
The initial eye examination should be carried out as determined by the table below, and by the neonatal team.
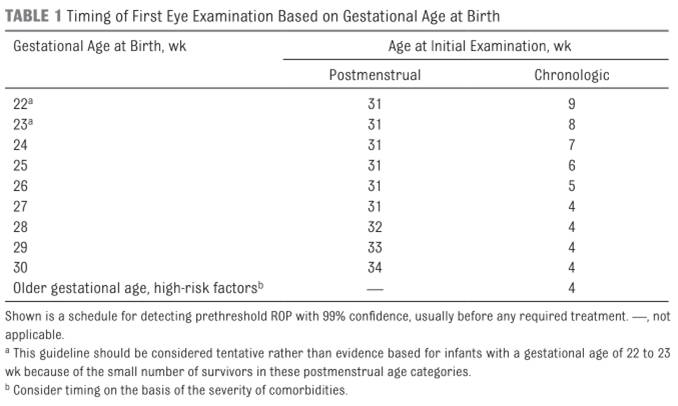
Source: (Fierson, 2018).
Follow up examinations are determined by the ophthalmologist. The date for follow up examinations should be recorded in the Consultation Notes in EMR, and in the Eye Examination Book by the ophthalmologist.
Administration
- Phenylephrine 2.5% minims and Tropicamide (i.e. Mydriacyl) 0.5% minims are to be used for eye reviews.
- Prior to laser treatment or in an infant with poorly dilating pupils, a more intensive regime may be requested by the consultant ophthalmologist during the round.
- Expected outcomes of the drops include dilation of the pupils.
If the patient is already ordered one or both drops as a regular medication, the patient will still require the extra doses for the eye examination. If the regular dose has been given within the hour of the eye examination, then consider that to be the first dose for the eye examination.
The ophthalmologist will advise the ANUM the time to commence the eye drop administration. The ANUM will inform the bedside nurse and medical team of the commencement time. The drops will be ordered in the MAR.
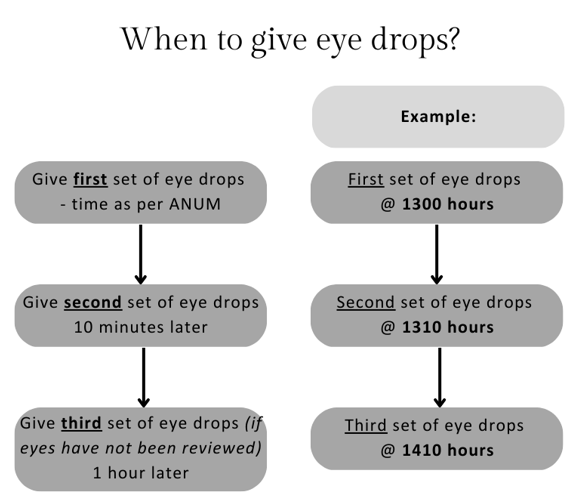
Administer the eye drops one hour
prior to the examination. The dose is then repeated 10 minutes after the initial dose. A third dose should be given again one hour later if the eyes have not been reviewed.
If the ophthalmology team is not present one hour after the third set of drops, please contact the ANUM to see if the ophthalmology team would like another set of drops.
Adverse
effects
Phenylephrine: common side effects include rebound miosis, hyperemia, stinging on instillation.
Tropicamide: rare side effects include photophobia, stinging of eyes (transient), blurred vision and transient intraocular pressure elevation (especially in pre-existing ocular hypertension).
Nursing care during and post procedure
- Ensure required dilating eye drops have been administered at the appropriate time.
- Administer
oral sucrose prior to the examination if needed.
- Position the infant supine in the bed and wrapped securely in a blanket.
- Assess the infant’s vital signs throughout the procedure; ask the ophthalmologist to cease the examination if the infant is unstable.
Post procedure documentation and communication
- The ophthalmologist records the results of the examination and further review or appointments in the Consultation Notes in EMR, and in the Eye Examination Book.
- The ophthalmologist will speak to the parents after the examination if parents are available. Otherwise, the managing neonatal team will discuss results with the parents, and if necessary, an appointment will be made with the ophthalmologist if there are any concerns.
Links
Disclaimer
Please remember to
read the disclaimer.
The development of this nursing guideline was coordinated by Lauren Cross RN, Butterfly Ward, and approved by the Nursing Clinical Effectiveness Committee. Updated October 2023.
Evidence Table
| Reference |
Source of
Evidence |
Key findings and
considerations |
| Dogra, M. R., Katoch, D., & Dogra, M. (2017). An Update on Retinopathy of Prematurity (ROP). The Indian Journal of Pediatrics, 1-7.
https://doi.org/10.1007/s12098-017-2404-3 |
Systematic Review |
- Screening guidelines
- Risk factors
- Classification
|
| Kennedy, K. A., Wrage, L. A., Higgins, R. D., Finer, N. N., Carlo, W. A., Walsh, M. C., Laptook, A. R., Faix, R. G., Yoder, B. A., Schibler, K., Gantz, M. G., Das, A., Newman, N. S., & Phelps, D. L. (2014). Evaluating retinopathy of prematurity screening guidelines for 24- to
27-week gestational age infants. Journal
of Perinatology, 34(4), 311-318.
https://doi.org/10.1038/jp.2014.12 |
Randomised Control Trial |
|
| Kristoffersen, L., Støen, R., Bergseng, H., Follestad, T., Theodorsson, E., Vederhus, B., Adde, L., & Austeng, D. (2019). Skin-to-skin contact during eye examination did not reduce pain compared to standard care with parental support in preterm infants. Acta Paediatrica, 108(8), 1434-1440.
https://doi.org/https://doi.org/10.1111/apa.14699 |
Randomised crossover study |
- Skin-to-skin during procedure, showing that there is no difference in pain compared with standard care
|
| Ramunno, B. (2022). Nursing management of neonates undergoing screening for retinopathy of prematurity. Infant, 18(1), 31-34. |
Quality improvement article |
- Nursing care during eye examination
|
|
Safer Care Victoria. (2021, February 17). Retinopathy
of prematurity (ROP). Retrieved from Safer Care Victoria: https://www.safercare.vic.gov.au/clinical-guidance/neonatal/retinopathy-of-prematurity-rop#goto-moreinformation- |
Clinical guideline/recommendations from authoritative bodies or national standards |
- Risk factors
- Screening criteria
- Treatment
- Follow-up
|