*Approved by CPG committee; PIC endorsement pending
See also
Diabetes mellitus
Key points
- Prolonged and/or severe hypoglycaemia can cause permanent neurological injury or death and therefore requires early recognition and management
- In children without diabetes, hypoglycaemia is considered at a BGL of <3.0 mmol/L if symptomatic, or at a BGL of <2.6 mmol/L, irrespective of symptoms or signs. Hypoglycaemia in neonates <48 hours of age is defined as a BGL of <2.6 mmol/L
- There are different BGL thresholds for children with diabetes
- Diagnostic tests should be considered in unexplained hypoglycaemia, however, should not delay management
- Enteral glucose replacement is preferable where conscious level allows
Background
Definition
- Hypoglycaemia in children is a blood glucose level (BGL) low enough to cause signs and/or symptoms of impaired brain function and neurogenic response. This response varies between individuals, age groups and developmental stages. Therefore, blood glucose thresholds are difficult to define
- In children who can communicate, diagnosis is based on symptoms of hypoglycaemia plus a low BGL with resolution of symptoms when BGL is normalised. In children who are unable to communicate, consider treatment if BGL is <3.0 mmol/L
- Neonates in the first 48 hours of life have a lower acceptable blood glucose level as they transition to extrauterine life. This should not persist beyond 72 hours of life. Neonatal hypoglycaemia in those <48 hours of age is defined as <2.6 mmol/L. This is irrespective of clinical signs and symptoms as neonates are often asymptomatic
- Severe hypoglycaemia refers to hypoglycaemia associated with serious cognitive dysfunction eg convulsions or coma
Cause
- An underlying medical condition is more likely in:
- Infants <1 year old
- Severe hypoglycaemia
- Recurrent hypoglycaemia
- Unexplained hypoglycaemia (absence of prolonged fast or intercurrent illness)
- Age at presentation can indicate the underlying cause
| Age |
Cause |
| Neonate <72 hours |
Prematurity, IUGR, perinatal asphyxia, hypothermia, sepsis, resp distress, hyperinsulinism secondary to maternal diabetic mother, macrosomia, syndrome (eg Beckwith-Wiedemann), pancreatic dysfunction, adrenal insufficiency |
| Neonate–2 years |
Congenital hyperinsulinism, inborn errors of metabolism, congenital hormone deficiencies eg growth hormone deficiency |
| Child |
Accelerated starvation*, hypopituitarism, adrenal insufficiency |
| Adolescent |
Insulinoma, adrenal insufficiency, eating disorder |
| All ages |
Complication of diabetes mellitus (see Diabetes mellitus), toxin ingestion (see Poisoning), other illness eg sepsis, congenital heart disease, tumour, adrenal insufficiency |
*Accelerated starvation is a diagnosis of exclusion. It requires a history of a prolonged fast (usually precipitated by a mild illness), with low BGL in association with ketonuria and/or ketonaemia and normalisation of BGL upon feeding
Assessment
Assess for features of hypoglycaemia and consider causes of increased glucose demand eg sepsis, cardiac failure, tumour, trauma
History
- Symptoms of hypoglycaemia
- Palpitations, anxiety, hunger, paraesthesia, lethargy, irritability
- Neonates <48 hrs may have apnoea, lethargy, seizures, hypotonia, jitteriness, poor feeding, a high pitched cry, altered behaviour or be asymptomatic
- Dietary history
- Prolonged fast or restrictive eating patterns
- Dairy intake (galactosemia)
- Juice (fructose intolerance)
- Protein (amino acid or organic acid disorders)
- Toxin ingestion eg alcohol, oral hypoglycaemic agents, aspirin, beta-blockers
- Past medical history
- Neonatal hypoglycaemia and birth weight
- Episodes suggestive of hypoglycaemia e.g. undiagnosed seizure disorder
- Insulin dependent diabetes mellitus (see Diabetes mellitus)
- Eating disorder
- Previous gastric surgery, fundoplication (postprandial hypoglycaemia)
- Family history
- Consanguinity
- Unexplained infant deaths (inborn errors of metabolism)
- Hormonal abnormalities eg adrenal insufficiency, growth hormone deficiency, hyperinsulinism
Examination
Signs related to hypoglycaemia
- Altered conscious state
- Hypothermia
- Pallor
- Tremor
- Sweating
- Seizures
- Weakness
Signs related to underlying diagnosis
- Poor growth and nutrition
- Features suggestive of a genetic syndrome
- Hyperpigmentation (can involve scars, mucosa, creases or be generalised)
- Midline defects including cleft palate, differences of sex development
- Hepatomegaly and/or hypotonia (inborn error of metabolism)
Management
Investigations
- Point of care BGL, ketone level and first urine sample following hypoglycaemic event
- Confirm true BGL with blood gas or a formal (laboratory) glucose level as, in the hypoglycaemic range, point of care glucometers can be inaccurate
- Infants <48 hours of age who respond appropriately to enteral feeds are unlikely to need extensive investigations
- Consider formal hypoglycaemia screen if there is unexplained, severe or recurrent hypoglycaemia, but do not delay correction of hypoglycaemia if venepuncture/IV access is challenging
Hypoglycaemia screen
- Ideally taken at the time of hypoglycaemia; send to lab immediately on ice
- Specimen collection advice may vary across institutions; consult local pathology services. Consider providing pre-prepared hypoglycaemia packs containing pathology tubes and information on local collection guidelines
| Blood |
Prioritise the following whilst hypoglycaemic:
- glucose level
- ketones (beta-hydroxybutyrate) if point of care ketones not already obtained
- insulin and C-peptide
- cortisol
- growth hormone
- lactate
If insufficient blood, the following can be collected following hypoglycaemia treatment:
- liver function tests
- ammonia
- free fatty acids
- amino acids
- acylcarnitine
|
| Urine |
This should be the first sample following the hypoglycaemic event and does not need to be sterile
- organic and amino acids
- reducing substances
- glucose
- ketones
|
Treatment
- Enteral glucose replacement is preferable where possible
- Appropriate short acting carbohydrates include apple juice, honey (in children >12 months) or 10% glucose polymer eg Polyjoule®
- Unsuitable options include oral rehydration solutions or icy poles (eg Hydralyte®) as these have minimal glucose content
- Consider NGT and antiemetics if vomiting
- Give glucose 10% 2 mL/kg IV bolus in severe hypoglycaemia. If there is no IV access or this is delayed, intraosseous glucose or IM glucagon should be considered
IM glucagon may be ineffective in prolonged hypoglycaemia or fasting
- Correction of hypoglycaemia must be followed by either administration of a slow-release carbohydrate (eg sandwich) or ongoing intravenous fluids (containing 5 or 10% glucose with normal saline)
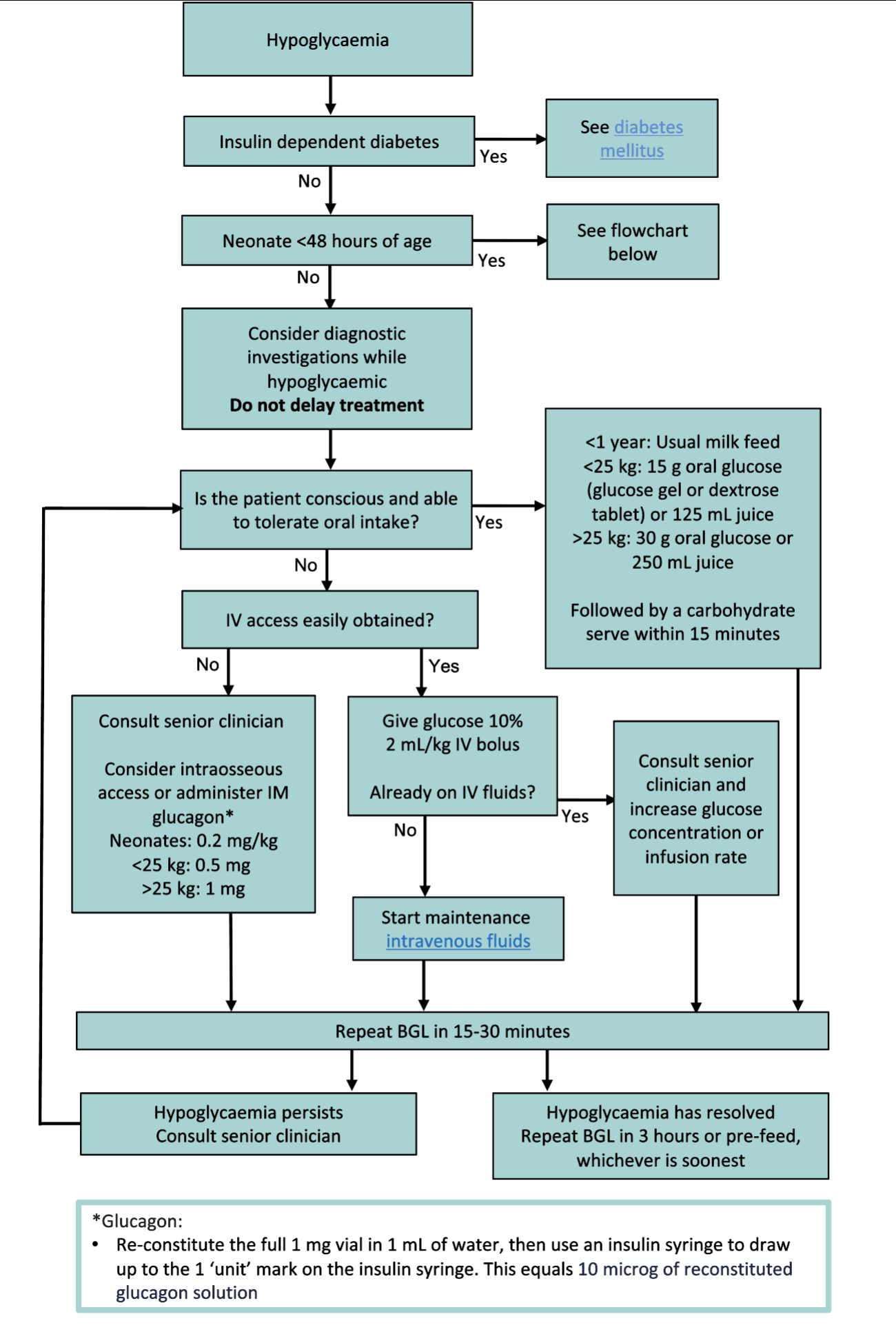
Treatment of hypoglycaemia
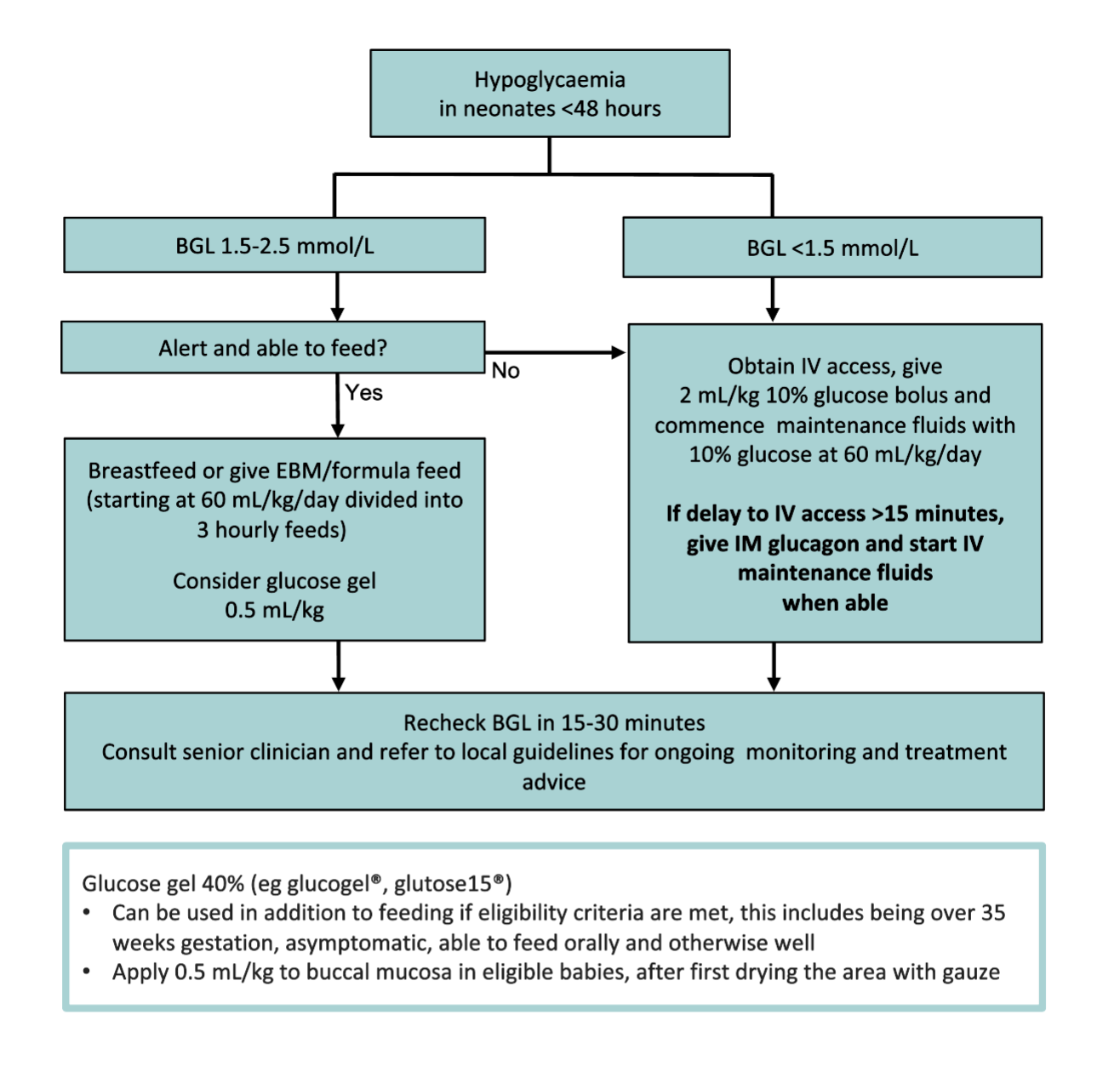
Treatment of hypoglycaemia in neonates
Discharge criteria
- Cause of hypoglycaemia is known or accelerated starvation assumed
- BGL is >3.0 on 2 consecutive occasions 3 hours apart, the child is asymptomatic and tolerating adequate oral intake
- Parental education has been provided
- Follow up is arranged if a hypoglycaemia screen was taken
Consider consultation with local paediatric team when
- Child not responding to treatment
- All neonates
- Unexplained hypoglycaemia or suspicion for an underlying medical cause
Consider transfer when
Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, call Retrieval Services
Additional notes
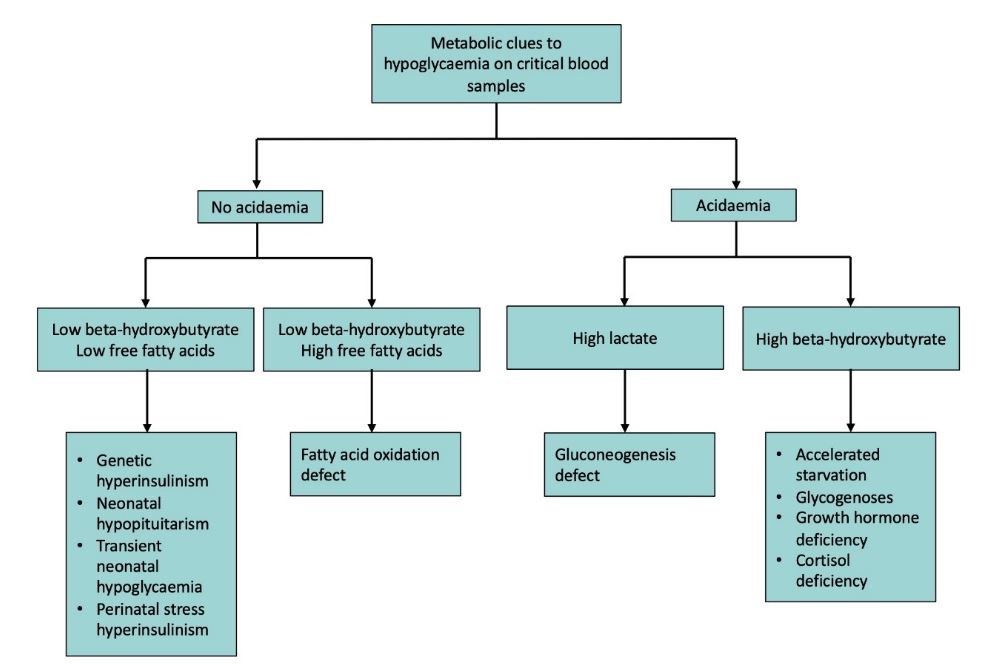
Interpretation of test results
Consult the Metabolic or Endocrinology team if there are any abnormal or unclear results
| Sample |
Test |
Interpretation |
| Blood |
Glucose |
Decreased in hypoglycaemia |
Ketones
(Beta hydroxybutyrate) |
Decreased or absent in:- Fatty acid oxidation defect
- Hyperinsulinaemia
|
| Lactate |
Increased in:
- Metabolic liver disease
- Glycogen storage disorders
- Sepsis
- Prolonged convulsion
|
| Free fatty acids |
Increased in fatty acid oxidation defect |
| Carnitine/acylcarnitine |
Abnormal in fatty acid oxidation defect |
| Ammonia |
Increased in:
- Organic acidaemias
- Tyrosinaemia
- Liver dysfunction
- Hyperinsulinism-hyperammonaemia syndrome
|
| Cortisol |
Decreased or lower than expected for clinical scenario in:
- Hypoadrenalism
- Hypopituitarism
- ACTH deficiency
|
| Insulin and C-peptide |
Any detectable insulin in the presence of BGL <2.6 mmol/L is inappropriate |
| Growth hormone |
Decreased or lower than expected for clinical scenario in:- GH deficiency
- Panhypopituitarism
|
| Amino Acids |
Abnormal in amino acid disorders |
| Electrolytes |
Abnormal in adrenal disorders |
| Liver function tests |
Abnormal in:
- Sepsis
- Liver Disease
- Metabolic defects
|
| Urine |
Ketones |
Decreased in: - Fatty acid oxidation defect
- Hyperinsulinaemia
|
|
| Reducing substances |
Present in:- Galactosaemia
- Fructosaemia
|
*Last updated August 2025
Reference List