1.
Summary
Toe fractures are common in children
Suspected fractures of the smaller toes (2nd-5th) with no clinical deformity may not require X-ray, as it would be unlikely to change management.
The big (1st) toe has an important role in toe-off phase of gait; suspected fractures should be formally diagnosed with xray with any fractures followed up in with the orthopaedics team.
Correction of any clinically evident angulation is a key part of Emergency Department Management.
Orthopaedic team management is necessary in the case of toe fractures with associated open nailbed injury (Seymour fractures)
2. How are they classified?
Phalanx fractures are classified by the following:
- Location of fracture: which toe and which phalanx is affected.
- Open or closed (includes nail bed injuries)
- Displacement / Rotational deformity
- Growth Plate involvement (Salter-Harris Classification)
3. How common are they and how do they occur?
Phalangeal fractures are the most common foot fracture in children.
Common mechanisms of injury include:
- Axial loading (stubbing toe)
- Abduction injury, often involving the 5th digit
- Crush injury caused by a heavy object falling on the foot or motor vehicle tyre running over foot
Less common mechanism:
- Joint hyperextension or hyperflexion, which can lead to spiral or avulsion fractures
4. What do they look like – clinically?
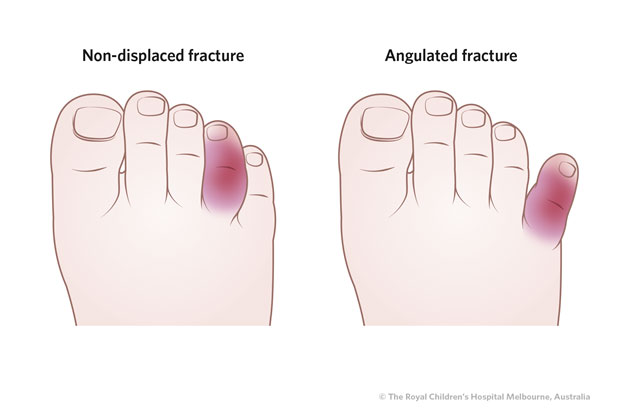
Fractured toes usually present with localised bruising and swelling.
It is important to check for angulation/mal-alignment and for rotational deformity (the position of the nail plate will give a guide to this and compare with toes on the other foot)
It is also important to check for significant nailbed injury. Any nail avulsion or displacement out of eponychial fold may indicate a Seymour fracture (see below)
5. What radiological investigations should be ordered?
Plain film – dorsoplantar, oblique and lateral views should be ordered where there is a suspected open fracture, a suspected fracture with associated angulation, a nailbed injury, or for any fracture of the great (1st) toe.
Note that where there is bruising and swelling of toe 2, 3, 4 or 5 but no significant deformity and no open wound, it may be reasonable to diagnose a fracture clinically (i.e. without X-ray) with management as below (ie simply buddy-tape the affected toe and wear firm-soled shoes for 3 weeks)
6. What do they look like on x-ray?
Figure 1: Seymour Fracture of the Great Toe (SH I with associated Nail Plate displacement)
 |
 |
Figure 2: Salter Harris III at base of distal phalanx
|
Figure 3: Undisplaced distal phalanx fracture
|
Figure 4 &5: Displaced and anbulated Salter-Harris II of 5th toe proximal phalanx, & undisplaced shaft fracture of 5th toe proximal phalanx . The angulated fracture will need reduction

Figure 6: Undisplaced Salter-Harris II of fourth and fifth toes
Figure 7 & 8: Salter-Harris IV and Salter-Harris III of great toe proximal phalanx.
7. When is reduction (non-operative and operative) required?
Significantly displaced or angulated fractures require reduction
This is particularly true of the fifth toe as malunion will cause longer-term issues such as fitting into shoes.
8. Do I need to refer to orthopaedics now?
- Open Fractures require orthopaedic consultation, including where a significant nailbed injury is suspected (see Seymour fracture, above in point 4).
9. What is the usual ED management for this injury, and what follow-up is required?
|
Fracture type
|
ED management
|
Follow-up
|
|
Undisplaced phalanx fractures
|
Rest, ice, elevation.
Firm soled shoe (eg school shoe)
|
None required for toes 2,3,4 and 5
Heal rapidly- within 3 to 4 weeks
Fractures of the big toe should be followed up in fracture clinic, due to its role at the end of the stance phase in the gait cycle
|
|
Open fracture
|
Refer to Orthopaedics
Establish Tetanus immunity status
Irrigate wound
Antibiotics
|
To be arranged by orthopaedic service
|
|
Seymour Fracture:
(SH I fracture of distal phalanx with associated nailbed injury or avulsion of proximal nail plate from eponychium)
|
Needs orthopaedic admission for removal of nail, irrigation, repair of nailbed +/- fracture reduction.
Commence antibiotics (cefalexin or cefazolin first line)
Tetanus vaccination if indicated
|
To be arranged by orthopaedic service
|
|
Fractures through the growth plate (Salter-Harris I - IV)
|
Non displaced: Buddy tape toes and use firm soled shoe or walking boot (CAM) for 3 weeks
Displaced: Can be reduced in ED then buddy taped and firm soled shoe: - discuss with Orthopedics if reduction is unsuccessful
|
Nondisplaced fractures of the other toes do not require specific follow-up
Displaced fractures (or for any fractures involving the great toe) - Fracture clinic within 7 days
|
|
Displaced/Angulated Phalanx Fractures
|
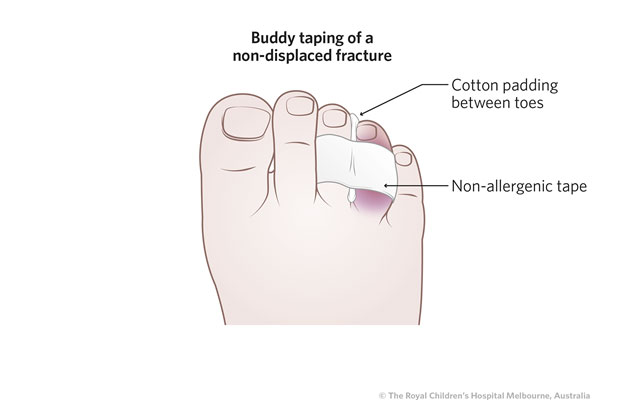
Can be reduced in ED: buddy tape in place with gauze between the toes.
Proximal fractures in children
<5yrs discuss with local Orthopaedic team as reduction success rate may be affected by size of phalanx
|
Fracture clinic in 7 days
|
|
Dislocation
|
Can typically be reduced and buddy taped, in ED (place some cotton between the toes to prevent skin maceration)
If irreducible, refer to Orthopaedics
|
No follow up required if successfully reduced
Wear supportive shoe until pain resolves (usually 3 weeks).
|
10. What advice should I give to parents?
Where buddy taping is performed, the parent should observe the method in case re-application is required in the coming weeks (including placing cotton between the toes to prevent skin maceration)
They should be instructed to keep the child in firm-soled shoes, ideally close-toed.
Where expectant management is appropriate, it is advised to keep the affected toe buddy taped for three weeks
11. What are the potential complications associated with this injury?
- Seymour fractures can result in osteomyelitis particularly where recognition of the injury is delayed
- Displaced Salter Harris fractures of the great toe may cause joint stiffness or growth arrest.
12. References
Boutis, K., 2018. Metatarsal and toe fractures in children, UpTodate.com
Eves, T., Oddy, M.J. Do broken toes need follow up in fracture clinic? The journal of foot and ankle surgery, 2016:55;488-491
Hatch, "Evaluation and Management of Toe Fractures", Am Fam Physician. 2003 Dec 15;68(12):2413-2418
Morris et al "Open Physeal Fracture of the Distal Phalanx of the Hallux" Am J Emerg Med 2017 35(7) 1035.e1.