1. Summary
Normal thumb function is an essential part of many activities of daily living, leisure activities and future occupational function. Careful early detection and management of thumb injuries in the ED is important for minimising any long-term morbidity associated with the injury
Most simple fractures can be immobilised in a thumb spica splint and followed up in an appropriate hand surgery clinic
This guideline covers types of thumb fracture that require specific management which differs from fractures of other digits. Other fractures are managed in the same way as fractures of the other digits: please consult [insert link to finger fracture guideline here]
2. How are they classified?
- By location (distal or proximal phalanx, or metacarpal),
- By presence or absence of growth plate involvement (Salter Harris classification),
- By particular fracture pattern (UCL injury/Skier's thumb, Bennett's fracture)
- Or as closed vs open fractures
Specific fracture types are shown in point 6 below.
3. How common are they and how do they occur?
Crush mechanism (for example in doorways) is particularly common in younger children, often resulting in tuft fractures or less commonly Seymour fractures , and may be associated with a nailbed injury [link eventually to hand injury guideline]
Hyperabduction of the thumb from either a fall or awkward contact from a ball whilst playing sports may result in a 'Skier's thumb' (UCL injury with or without bony avulsion from the base of P1)
Axial loading of the thumb may result in intra-articular metacarpal base fracture in the adolescent patient (Bennett or Rolando)
4. What do they look like - clinically?
Fractures of the thumb are usually associated with local bruising, swelling, pain and loss of function, with or without deformity. Rotational deformity can be assessed by comparison with the uninjured side, but is difficult to appreciate in the thumb.
Subungual haematoma or displacement of the proximal edge of the nail plate out of the eponychial fold may indicate an underlying fracture.
Findings for specific fracture types are listed in the table below
5. What radiological investigations should be ordered?
True lateral, true AP and oblique views on XRay
6. What do they look like on x-ray?
Fractures at the base of thumb:
 |
Bennett Fracture, usually from axial loading of the thumb in patients with closed physes.
X-ray shows a small fragment of the metacarpal base articulating with the trapezium; muscles attaching elsewhere on the main part of the metacarpal tend to pull it into subluxation.
Examination will show bruising and tenderness at the thumb MCP joint
ED management involves immobilisation in a thumb-spica (see below) and arranging an appointment within a week with the hand surgery team (At RCH this is Plastic Surgery)
Definitive management by the hand surgery team requires reduction, usually involving K-wire insertion
|
 |
Fracture through an open physis, involving the same mechanism and deformation patterns as in a Bennett fracture.
X-ray: This example shows a Salter-Harris II fracture of the metacarpal.
Management is as with a Bennett Fracture above. |
 |
Fracture proximal shaft of metacarpal, usually from axial loading.
Management is as with a Bennett fracture, as it is usually subjected to the same deforming forces from the muscle insertions. |
Fractures of proximal phalanx
 |
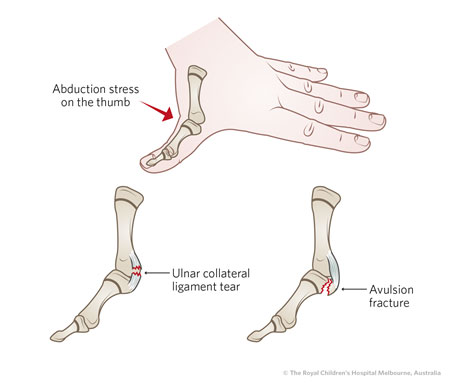
Ulnar Collateral Ligament Injury/Avulsion (a.k.a. Skier's thumb)
Usually results from hyperabduction of the thumb.
Examination shows bruising and swelling to MCP joint, with focal tenderness to ulnar aspect of joint and pain there with pinch grip.
Test the ligament by applying a valgus deformity to the MCP joint with thumb in slight flexion and also full extension: laxity of >35 degrees (or >15 degrees more than uninjured thumb) indicates UCL injury, regardless of Xray appearance .
X-Ray may show an avulsion at the UCL insertion, or may be normal
ED Management involves application of a thumb spica (below) and arranging early follow-up with the Hand Surgery Team (regardless of whether avulsion present or absent)
Definitive Management is mostly not-operative with hand therapy, but some cases require surgical repair.
 |
| |
Radial Collateral Ligament Injuries
Examination reveals ligamentous laxity on the radial aspect of the MCP joint, and local tenderness
X-Ray findings are usually normal; avulsion is uncommon. |
 |
Proximal Phalanx shaft fracture
Examination reveals local swelling and tenderness +/- deformity
ED Management involves closed reduction if angulated or displaced, then immobilisation in a thumb spica.
Follow-up will be via hand surgery clinic |
 |
Fracture through physeal plate of proximal phalanx (Salter-Harris)
Examination will reveal local swelling and tenderness
ED Management involves immobilisation in a thumb spica (with closed reduction if significantly angulated or displaced)
Follow-up will be via hand surgery clinic within a week. |
 |
Proximal Phalanx Neck fracture
Examination will reveal local swelling and tenderness.
Definitive Management requires early expert reduction by specialist hand surgery team, often with K-wire fixation. This should take place within a few days.
ED Management involves immobilisation in a thumb spica and appropriate communication with the hand surgery team. |
Fractures of distal phalanx
 |
Distal Phalanx Tuft Fracture
Examination reveals local swelling and tenderness +/- deformity +/- nailbed injury
Management consists mainly of treating any associated soft tissue or nailbed injury or tip avulsion.
Start appropriate oral antibiotics for any open fractures.
Follow up is with GP for most injuries, but Hand Surgery team if nailbed repair required or significant tissue disruption |
 |
Seymour Fracture
These are open fractures through the growth plate with associated nailbed injury and displacement of proximal nail plate from the nail fold.
They are significantly less common in the thumb than in the other fingers.
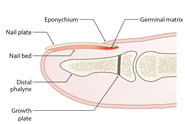

Management requires admission for washout, debridement, reduction, nailbed repair and antibiotics. |
7. When is reduction (non-operative and operative) required?
Extra-articular fractures with >30 degrees angulation require closed reduction, which may occur in the ED under local/regional anaesthesia or procedural sedation or both, with K- wire fixation if reduction is inadequate or unstable.
Seymour fractures require early identification with debridement and pinning in theatre to avoid malunion, infection or nail deformities
Fractures at the base of the Metacarpal require reduction with hand surgery team involvement, and likely K-wire fixation
The number of attempts at reducing fractures across a physis anywhere should be kept to a minimum; if reduction cannot be achieved after one or two attempts referral to the hand surgery team should occur to minimise chance of growth arrest.
8. Do I need to refer to hand surgery now?
- Open hand fractures, including Seymour fractures
- Joint dislocations unable to be reduced
- Displaced intra-articular fractures at the thumb carpo-metacarpal joint have better long-term outcomes with early reduction +/- k-wires performed by specialist hand surgery team
- Phalangeal neck fractures
- Delayed presentations 3-14 days after injury where angulation or joint involvement is present, as malunion may occur before clinic review is possible
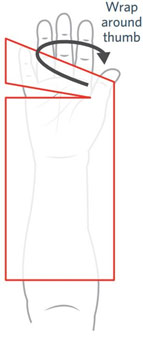
9. What is the usual ED management for these fractures?
- Reduction may be required in the ED as described above
- Almost all closed thumb fractures can be immobilised in a thumb spica in plaster or fibreglass, and followed up in clinic by hand surgery in approximately one week's time.
- In fractures of the thumb metacarpal (UCL/Skiers, Bennett's, shaft fractures) the spica should be applied in a fashion that allows mobility at the IP joint of the thumb


10. What follow-up is required?
- Almost all closed thumb fractures should be followed up in hand surgery clinic in approximately one week's time, with the exceptions in point 8. above.
- Swelling will mostly resolve during this interval, allowing a more accurate assessment of whether any further surgical management is required.
- The clinic also involves access where required to multidisciplinary assessment including with hand therapists (OT/physiotherapy) to optimise return to normal hand functioning.
11. What advice should I give to parents?
- Plaster care advice for the thumb spica
- Elevation of the injured limb in the first few days after injury to allow swelling to resolve
- Avoidance of any activities where sudden impact to the injured thumb is possible, such as sports.
12. What are the potential complications associated with these injuries?
Arthritis, particularly in the case of intra-articular fractures or delay to diagnosis
Malunion
Stenar Lesion of UCL resulting in MCP joint instability
Delayed diagnosis of base of thumb fractures leading to long term reduction in joint function.
13. References (ED setting)
Kozin Fractures and Dislocations along the Pediatric Thumb Ray Hand Clin 2006 22(1) 19-29
Nellans, K. et al "Pediatric Hand Fractures" Hand Clin 2013; 29(4): 569-78
Information specific to RCH: Thumb injuries requiring specialist input are handled here by the Plastic Surgery team. At other centres, this may be an orthopaedic surgical team. This guideline refers to 'hand surgery' to encompass both specialty fields.
Last updated December 2020