Fracture Guideline Index
See also:
Supracondylar fracture of the humerus - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
-
Parent information fact sheet
1. Summary
Anteroposterior (AP) and lateral x-rays of the distal humerus (not elbow) should be ordered if a supracondylar fracture of the humerus is suspected.
|
Gartland classification for extension fractures
|
ED management
|
Follow-up
|
|
|
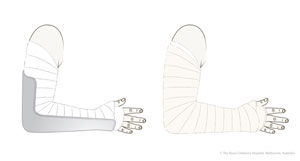
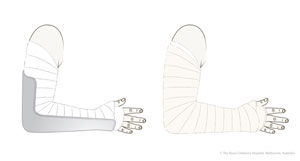
Immobilisation in an above-elbow backslab in 90 degrees elbow flexion with sling for 3 weeks. The backslab and sling should be worn under clothing (e.g. loose fitting shirt) and not through the sleeve
|
TIP: Avoid putting on a short, flimsy backslab. The backslab should extend as high above the elbow as possible (i.e. close to the axilla) and down to the metacarpophalangeal joints (MCP) joints.
|
|
Give parent
undisplaced supracondylar fracture fact sheet
Undisplaced fractures can be followed up with the GP in 3 weeks. Repeat x-ray is not required. |
|
|
Refer to the nearest orthopaedic on call service for advice
A gentle reduction can be achieved by an anterior push on the distal fragment as the elbow is flexed to 90 degrees
Note the exception is type II injuries with coronal plane deformity (see radiological assessment). These must always be managed by orthopaedics
|
Observation overnight
Fracture clinic within 7 days post-injury with x-ray of distal humerus in backslab
|
|
|
Refer to the nearest orthopaedic on call service
Requires urgent reduction and percutaneous pin fixation
|
To be organised by orthopaedic service
|
2. How are they classified?
A supracondylar fracture occurs through the thin part of the distal humerus above the level of the growth plate.
Supracondylar fractures are initially divided into two types, depending on the direction of displacement of the distal fragment:
- Flexion-type (rare) - distal fragment is displaced anteriorly
- Extension-type (98%) - distal fragment is displaced posteriorly
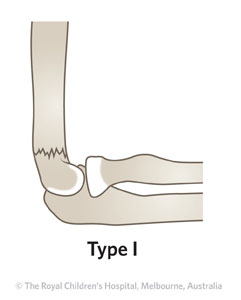
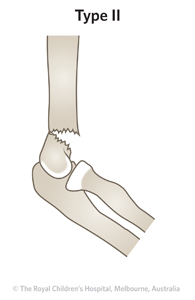
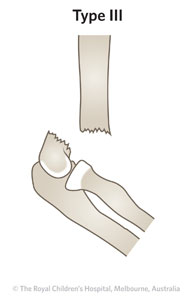
The Gartland classification system is used to describe the severity of displacement for extension-type supracondylar fractures.
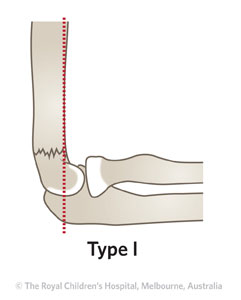
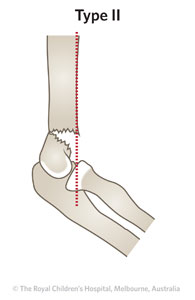
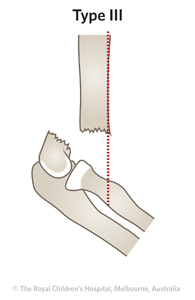
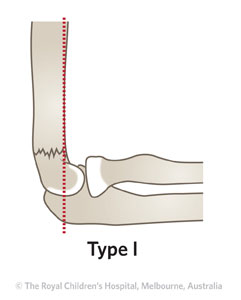
Table 1: Gartland classification system for extension-type supracondylar fractures.
|
Type
|
Description
|
|
|
Undisplaced fracture
|
|
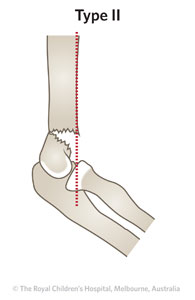
Angulated fracture with intact posterior cortex
|
|
|
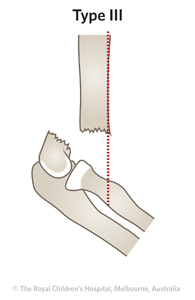
Displaced distal fragment posteriorly, no cortical contact
|
3. How common are they and how do they occur?
Supracondylar fractures are the most common elbow fracture in children, especially in the first decade of life. The peak age is from 5-8 years. The usual mechanism is a fall onto the outstretched hand with hyperextension at the elbow.
4. What do they look like - clinically?
The child will present with pain, swelling, and limited elbow range of motion (ROM). A displaced fracture in extension typically has an S-shaped deformity. Swelling can be very rapid. Younger children can present with the appearance of a dislocated elbow.
Always examine for associated injuries. A thorough neurological examination including screening of the median, radial and ulnar nerves should be undertaken and documented. The radial pulse should be felt and documented. The skin should be assessed for swelling and bruising.
|
|
Clinical signs that indicate urgent orthopaedic review in the ED include:
- absence of radial pulse
- ischaemia of hand: pale, cool
- severe swelling in forearm and or elbow
- skin puckering or anterior bruising
- open injury
- neurological injury
|
5. What radiological investigations should be ordered?
Clinically deformed fractures should be immobilised in about 30 degrees short of full extension, prior to x-ray evaluation. This is important for pain management.
Anteroposterior (AP) and lateral x-rays of the distal humerus (not elbow) should be obtained. If there is any clinical suspicion of injury in the forearm or wrist then separate films of these areas should be ordered.
|
|
It is very important to identify other injuries in the forearm, as this has major implications with regards to swelling. |
6. What do they look like on x-ray?
|
|
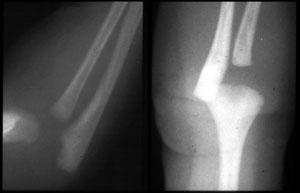
The Gartland type classification is based on the lateral x-ray, identifying where the capitellum sits in relation to a line drawn down the anterior aspect of the humerus - the anterior humeral line.
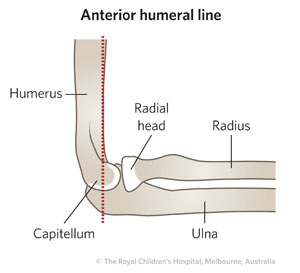
In a normal elbow, a line drawn on a lateral view along the anterior surface of the humerus should pass through the middle third of the capitellum. To assess this accurately, the view must be a true lateral view of the elbow.
If it passes through the anterior third of the capitellum or misses the capitellum completely, the fracture is displaced posteriorly.
|
Gartland type I
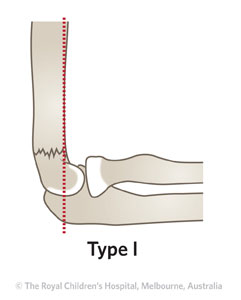
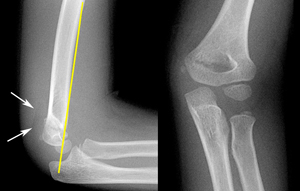
Figure 1: Lateral and AP x-ray of three year old girl with Gartland type I supracondylar fracture. In Gartland type I fractures, the anterior humeral line (yellow line) passes through the middle of the capitellum. These fractures may be difficult to see on plain x-ray. Suspect a fracture if anterior and/or posterior fat pad signs (arrows) are present (seen on lateral x-ray).
Gartland type II
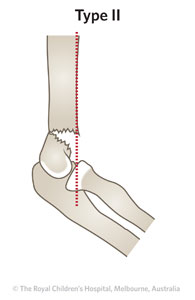
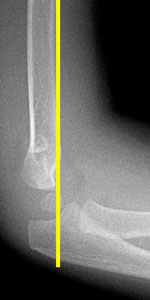

Figure 2: Lateral and AP view of two year old girl with Gartland type II supracondylar fracture. On lateral view the anterior humeral line is anterior to the middle of capitellum. On the AP view, fracture lines can be seen through the metaphyseal bone of the distal humerus on either side of the olecranon fossa. There may be medial or lateral translation or tilt of the distal fragment.
Gartland type II with coronal plane deformity
Figure 3: Four year old boy with Gartland type II fracture with coronal deformity. Gartland type II supracondylar fractures can sometimes have a significant displacement in the AP x-ray with either tilt or translation, which would indicate treatment according to the treatment protocol for type III injuries.
Gartland type III
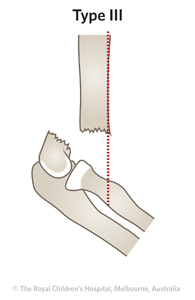

Figure 4: Gartland type III supracondylar fracture of six year old girl.
|
|
Extremely young patients less than 3 years of age do not yet have ossification of the capitellum. The supracondylar injury in these patients appears to be a dislocation of the elbow but is usually a physeal separation (Salter-Harris type I). True elbow dislocation in this age group is very rare.
Salter-Harris type I injury at birth
|
7. When is reduction (non-operative and operative) required?
Gartland type I fractures do not require reduction. Gartland type II fractures can be gently reduced by pushing anteriorly on the distal fragment as the elbow is flexed to 90 degrees. Gartland type III, and flexion supracondylar fractures are treated with reduction and percutaneous K-wire fixation.
Patients should be kept nil orally until a decision about the timing of surgery is made. For open fractures, tetanus immunisation status should be assessed.
|
|
On lateral x-ray post-reduction, it is acceptable for the fracture to remain in a degree of extension to the extent that it would still be classified as a type II fracture.
Alignment in the AP x-ray is more important. No degree of tilt can be accepted on the post-reduction films. Such displacement would imply a more unstable fracture requiring surgical reduction.
|
8. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- Associated absence of pulse or ischaemia
- Open or impending open fracture (large anterior bruise)
- Associated nerve injuries
- Gartland type II & III fractures
- Associated same arm forearm or wrist injury
- Flexion supracondylar fractures
- Unable to achieve or maintain reduction (including if ED is not experienced in fracture reduction, splinting or casting)
9. What is the usual ED management for this fracture?
For extension-type supracondylar fractures, management is guided by the Gartland classification system and clinical examination (e.g. presence of neurovascular compromise).
Table 1: ED management of supracondylar fractures of the distal humerus.
|
Fracture type
|
Type of reduction
|
Immobilisation method & duration
|
|
|
No reduction required
|
Immobilisation in an above-elbow backslab with 90 degrees elbow flexion with sling for 3 weeks
|
TIP: Avoid putting on a short, flimsy backslab. The backslab should extend as high above the elbow as possible (i.e. close to the axilla) and down to the MCP joints.
|
|
|
|
Refer to the nearest orthopaedic on call service for advice
A gentle reduction can be achieved by an anterior push on the distal fragment as the elbows is flexed to 90 degrees
Note the exception is type II injuries with coronal plane deformity (see radiological assessment). These must always be managed by orthopaedics
|
Immobilisation in an above-elbow backslab with 90 degrees elbow flexion with sling for 3 weeks
The position of the elbow after supracondylar fracture is much more important than the position of the fracture. That is, immobilisation in greater than 90 degrees of flexion can result in significant swelling and potentially vascular compromise. This can have a much more profound effect on final functional outcome than a minor displacement of the fracture
|
|
|
Refer to the nearest orthopaedic on call service
Requires reduction and percutaneous pin fixation
|
Refer to the nearest orthopaedic on call service
|
10. What follow-up is required?
Gartland type I fractures can be followed up by a GP in three weeks. Repeat x-ray is not required.
Gartland type II supracondylar fractures should have follow-up arranged in the fracture clinic one week post-injury.
11. What advice should I give to parents?
For Gartland type I fractures, parents should be given
undisplaced supracondylar fracture fact sheet.
The child should be managed in a sling for 3 weeks. Emphasis should be placed on elevation of the limb (elbow above the heart) for the first 48 hours. The backslab and sling should be worn under clothing (e.g. loose fitting shirt) and not through the sleeve.
All supracondylar fractures result in marked elbow stiffness following removal of the backslab. In the majority of cases, full (or near) ROM returns with time and physiotherapy is not required.
Minor degrees of extension of the distal fragment can result in a slightly altered range of extension movement at the elbow at one year.
Displacement in the coronal plane can result in a varus malposition, which is unacceptable cosmetically, although this has very little functional deficit.
Poorer outcomes result from vascular injury, compartment syndrome, Volkmann's ischaemic contracture of the forearm, permanent nerve palsy or malunion (gunstock deformity/cubitus varus).
12. What are the potential complications associated with this injury?
|
|
Gartland type II injuries rarely have neurovascular problems but may result in malunion (gunstock deformity/cubitus varus) and need a corrective osteotomy.
Gartland type III injuries have the highest risk of neurovascular injury. However, with appropriate management, Volkmann's ischaemia can be avoided and permanent nerve injury is very rare.
|
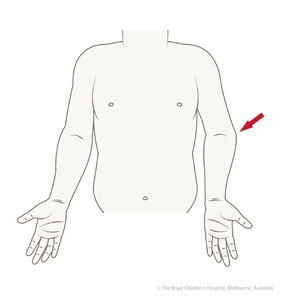
Figure 5: Cubitus varus (red arrow) deformity of the elbow can result from malunion of a supracondylar humeral fracture. The normal carrying angle of the arm is reversed and the forearm deviates to the midline when the elbow is extended.
Complications associated with vascular injury include compartment syndrome followed by the later development of Volkmann's ischaemic contracture of the forearm.
Malunion (gunstock deformity/cubitus varus) can result from tilt in the coronal plane.
Neurological injuries can result from the fracture itself or the treatment. The great majority of the neurological injuries resolve with time.
See
fracture clinics for other potential complications.
13. Parent information fact sheet
References (ED setting)
American Academy of Orthopedic Surgeons. Guideline on the Treatment of Pediatric Supracondylar Humerus Fractures 2011.
http://www.aaos.org/Research/guidelines/ SupracondylarFracture/SupracondylarFracture_Guideline.asp. Retrieved 19 December 2011.
Azbug JM, Herman MJ. Management of supracondylar humerus fractures in children: Current concepts. J Am Acad Ortho Surg 2012; 20(2): 69-77.
Herring JA. Upper extremity injuries. In Tachdjian's Pediatric Orthopedics, 4th Ed. Saunders, Philadelphia 2008. p.2451-536.
Skaggs DL, Flynn JM. Supracondylar fractures of the distal humerus. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.487-532.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network.
To provide feedback, please email rch.orthopaedics@rch.org.au