-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
- References
1. Summary
The Scaphoid bone is one of 8 carpal bones in the wrist.
The scaphoid begins ossification around the 4th year of age and may be earlier in females than males.
Scaphoid fractures are much more common in adolescents than younger children. Approximately 75% of the arterial supply is from branches of the radial artery through vascular perforations on the dorsal surface near the tubercle and waist.
As vascular supply to the proximal pole is mainly retrograde, a fracture through the waist places the proximal pole at risk of avascular necrosis. As such, fractures to this area or more proximally can cause poor outcomes if not managed appropriately. Mismanaged fractures can cause malunion and necrosis to the proximal end of the bone and in turn cause instability of the wrist joint.
Whilst immobilisation of scaphoid fractures has traditionally been in a thumb spica, there is good evidence to show that immobilisation of the wrist alone in a short-arm cast is just as effective in promoting union and preventing avascular necrosis.
2. How are they classified?
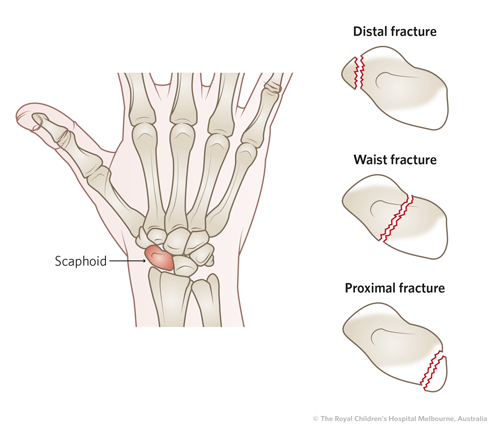
By location: Proximal third, Middle third, Distal third, articular surface or tubercle
By orientation: transverse, vertical or oblique
Displaced or non-displaced
3. How common are they and how do they occur?
Scaphoid fractures are easily the most common fracture of the carpal bones.
It is rare for very young children (
<10 years) to sustain scaphoid fractures. Predominantly, scaphoid fractures happen in adolescents or older children.
Scaphoid fractures usually occur as a result of a fall on the outstretched hand
4. What do they look like clinically?
On examination
- tenderness in the anatomical snuffbox
- tenderness on axial loading of the thumb caused by holding the thumb and applying force towards the 1st metacarpal.
- Limited range of motion of the wrist
- Bruising may also be present over this area
5. What Radiological Investigations should be ordered?
Plain x-ray with scaphoid-specific views is a good initial screening test, however, negative x rays do not necessarily rule out a scaphoid fracture especially if clinical suspicion is high.
If x-ray is normal and clinical suspicion is high, then CT or MRI may be obtained to further rule out fracture depending on clinical situation. If further imaging cannot be obtained in time, the patient can be treated with a plaster and followed up early with GP or fracture clinic where CT/MRI can be arranged.
If the x-ray is normal and an MRI cannot be immediately obtained, then it is generally recommended to immobilize the wrist as discussed below.
6. What do they look like on x ray?
Scaphoid fractures are not always visible on X-ray as discussed above.
The above images show a non-displaced fracture of middle third of scaphoid
The above images show a fracture of the scaphoid tubercle
Undisplaced fracture of distal pole of scaphoid
7. When is reduction required?
Scaphoid fractures almost never require acute reduction in ED.
(The exception is associated with a trans-scaphoid peri-lunate fracture-dislocation - in this setting, orthopaedics should be contacted to assist with urgent reduction, ideally in theatre).
8. Do I need to refer to Orthopaedics now?
Urgent referrals are very rarely required for scaphoid fractures, except for open injuries or dislocations.
Most scaphoid fractures can be referred for fracture clinic review ideally in 1-2 weeks.
9. What is the usual ED management for this fracture?
|
Confirmed Scaphoid Fracture on X-Ray or CT |
- Immobilisation as shown below
- Referral to be seen in fracture clinic within 1-2 weeks (in some areas, this may be a GP with an interest in the area)
|
|
Clinically Suspected Scaphoid Fracture not shown on plain X-Ray |
- Immobilisation as shown below
- Referral to be seen in fracture clinic within 1-2 weeks with repeat X-Ray (in some areas, this may be a GP with an interest in the area)
- Where the repeat X-ray shows a fracture which was previously occult, the patient should complete 6 weeks of immobilisation
- Where the repeat X-ray does not reveal a fracture but there is persisting snuff box tenderness, consideration should be given to MRI to confirm or exclude a fracture
- Where the repeat X-ray does not reveal a fracture and there is no ongoing tenderness, the cast can be removed and the patient discharged from follow-up.
Alternative:
- If the circumstances are such that immobilisation for two weeks with review represents too much inconvenience for the child, they can consult with their GP for consideration of MRI scaphoid. If an MRI occurs and shows no fracture, the cast can be removed.
|
Immobilisation: The most important thing is immobilisation at the wrist to prevent movement at the radio-carpal joint. There is no difference in the rates of non-union between a short-arm cast or a thumb spica; either is perfectly acceptable treatment, but the short-arm cast has less impact on function and is better tolerated.
Option 1:
Option 2:
Note that if you are referring to a GP for follow up, a removable splint should be applied as removal of a circumferential cast is difficult in that setting.
10. What follow up is required?
See point 9 above
11. What advice should I give to parents?
If identified early and managed appropriately then union of the fracture is very likely, (provide the fracture is not in the proximal pole).
Keep cast on until reviewed post-imaging.
Follow up is very important and parents should be advised that they attend appointment as arranged, because undertreated scaphoid fractures can have significant long-term implications.
12. What are the potential complications of this injury?
Potential complications of this injury include avascular necrosis, leading to what is termed SNAC wrist (scaphoid non-union advanced collapse) when established.
Delayed diagnosis and scaphoid nonunion can result in attrition of fracture ends, bone loss, and cyst formation, which jeopardizes chance of success with surgery.
References
Adler, B.H., Bloom, D.A., Bulas, D.I., Coley, B.D., Donaldson, J.S., Faerber, E.N., Frush, D.P., Hernanz-Schulmann, M., & Strouse P.J. (2008). Caffeys Paediatric Diagnostic Imaging (11th Ed.). Philadelphia: Mosby Elsevier.
Ahmed, I., Ashton, F., Tay, W.K., & Porter, D. (2014). The Paediatric Fracture of the Scaphoid in Patients aged 13 Years and Under: An Epidemiological Study. Journal of Paediatric Orthopaedics, 34(2), 150-154.
Australian Government Department of Health and Aging (2009) Australasian Triage Scale: Emergency Triage Education Kit. Retrieved April 10, 2017 from
https://www.health.gov.au/internet/main/publishing.nsf/Content/387970CE723E2BD8CA257BF0001DC49F/$File/Triage%20Education%20Kit.pdf
Clay et al ‘Need the thumb be immobilized in scaphoid fractures? A randomized prospective trial’ J Bone Joint Surg Br 73(5):828-32
Carty,H., Brunelle, F., Stringer, D.A., & Kao, S.C. (2005). Imaging Children (2nd Ed.). Sydney: Elsevier Churchill Livingstone.
Evenski, A.J., Adamczyk, M.J., Steiner, R.P., Morscher, M.A., & Riley, P.M. (2009). Clinically Suspected Scaphoid Fractures in Children. Journal of Paediatric Orthopaedics, 29(4), 352-355.
Gunal, L., & Altay, T. (2011). Avascular necrosis of the scaphoid in children treated by splint immobilisation. The Journal of Bone and Joint Surgery, 93B(6), 847-848.
Gurian. M.S., & Pollock. A. (2010). Scaphoid Fracture: Paediatric Emergency Care. Paediatric Emergency Care, 26(11), 871-872.
Jones, B.J., & Sunnamon, M. (2015). Review of MRI wrist examination since introduction of Medicare item number. Journal of Medical Imaging and Radiation Oncology, 59, 289-291.
Jorgsholm, P., Thomsen, N., Besjakov, J., Abrahamson, S., & Bjorkman, A. (2016) MRI shows a high incidence of carpal fractures in children with posttraumatic radial-sided wrist tenderness. Acta Orthopaedica, 87(5), 533-537.
Kawanishi et al (2017) In Vivo Scaphoid Motion During Thumb and Forearm Motion, J Hand Surg Am 42(6):475.e1-e.7
Khalid, M., Jummani Z.R., Kanagaraj, K., Hussain, A., Robinson, D., Walker, R. (2010), Role of MRI in the diagnosis of clinically suspected scaphoid fracture: analysis of 611 consecutive cases and a literature review. Emergency Medical Journal, 27(4), 266-269.
Lotgers, T.T., Linhart, W., Schubert, D., Windolf, J., & Schadel-Hopfner, M. (2008). Diagnostic Approach for Suspected Scaphoid Fractures in Children. European Journal of Trauma and Emergency Surgery. 2, 131-134.
Memarsadeghi, M., Breirenseher, M.J., Schaefer-Prokop, C., Weber, M., Aldrian, S., Gabler, C., & Prokop, M. (2006). Occult Scaphoid Fractures: Comparison of Multidetector CT and MR Imaging – Initial Experience. Radiology, 240(1), 169-176.
Unay, K., Gokcen, B., Ozkan, K., Poyanli, O., & Eceviz, E. (2009). Examination tests predictive of bone injury in patients with clinically suspected occult scaphoid fractures. Injury, 40, 1265-1268.
Waters; P, Hedequist D. Boston Childrens Illustrated Tips and Tricks in Pediatric Orthopaedic Fracture Surgery. 2019.
Waters P, Bae D. Pediatric Hand and Upper Limb Surgery: A Practical Guide. 2nd ed. Boston: 2020.
Yin, Z.G., Zhang, J.B., Kan, S.L., & Wang, X.G. (2012). Diagnostic accuracy of imaging modalities for suspected scaphoid fractures. The Journal of Bone and Joint Surgery. 94B(8), 1077-1085.
Last updated December 2020