Fracture Guideline Index
See also:
Proximal humeral fractures - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
1. Summary
Most proximal humeral fractures do not require reduction as remodelling is extremely effective in the proximal humerus.
The usual treatment for this fracture is immobilisation of the shoulder in a sling, body swathe or shoulder immobiliser.
Patients should be seen in the fracture clinic or by an interested GP within 7 days for follow-up with x-rays to assess further displacement.
2. How are they classified?
Proximal humeral fractures can be classified according to its location:
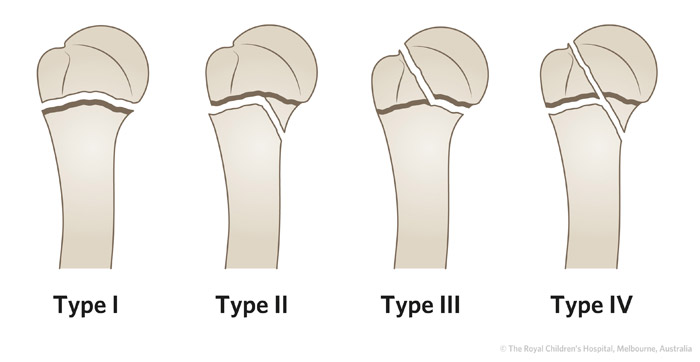
- Physeal fractures - based on
Salter-Harris classification system. Most are Salter-Harris I or II injuries.
- Metaphyseal fractures - buckle or complete
- Greater or lesser tuberosity fractures
3. How common are they and how do they occur?
Proximal humeral fractures represent
<5% of all paediatric fractures. These fractures may occur either through the physis (growth plate) or in the metaphysis. They are usually the result of a fall on an outstretched hand, with the humeral head locked against the glenoid and the force transmitted to the physeal or metaphyseal region.
Physeal injuries are more common in late childhood and adolescence, while metaphyseal injuries, including buckle injuries are more common in younger children.
Occasionally a fracture can occur through a benign bone cyst in childhood. This would be regarded as a pathological fracture. Lower energy trauma is required to sustain this type of fracture, than in a normal bone.
Proximal humeral fractures as a result of non-accidental injury are not common, and do not have the same association as humeral shaft fractures in this regard.
Infantile proximal injuries are usually transphyseal separation incurred during the birth process. These may not be seen on x-ray as the proximal humeral epiphysis appears at about six months of age. Ultrasound may be needed in this setting.
4. What do they look like - clinically?
The child will present after a defined injury with pain and loss of movement around the shoulder. There may be swelling and deformity, but with the coverage of the fracture by the shoulder muscles, this may not be obvious. The primary clinical sign is reluctance to move the shoulder and pain.
5. What radiological investigations should be ordered?
Anteroposterior (AP) and axillary lateral radiographs of the shoulder should be obtained. An axillary lateral view will give a lateral projection and show the relationship of the humeral head with the glenoid fossa.
6. What do they look like on x-ray?
The appearance will depend on the degree of angulation and/or displacement of the shaft relative to the humeral head. Attention should be drawn to growth plate involvement.
Buckle injuries may appear as a simple bump usually on the medial cortical margin of the metaphysis.
Proximal humeral fractures should be described in relation to:
- Displacement - a percentage of the humeral shaft diameter
- Angulation of neck shaft - varus (decreased) or valgus (increased)


Figure 1 : AP and lateral x-ray of 10 year old girl with Salter-Harris type II fracture of the proximal humerus.
7. When is reduction (non-operative and operative) required?
The proximal physis contributes 80% of the length of the humerus. Due to the enormous remodelling potential, most of these injuries do not require reduction. There is no role for attempted reduction in the ED.
The older child with greater deformity may be treated with closed reduction. This is controversial and there are no agreed figures to guide closed operative reduction.
Approximate indications are:
- 5-12 years - accept 60 degree angulation and 50% displacement
- >12 years - accept 30 degrees angulation and 30% displacement
Isolated greater tuberosity fractures with displacement in the adolescent are an exception group in which surgical reduction and fixation is usually required.
8. Do I need to refer to orthopaedics now?
Indications for prompt referral to the orthopaedic on call service include:
- >50% displacement of the humeral head relative to the shaft
- Angulation on the AP or lateral x-ray of >60 degrees in a child
<12 years old, or >30 degrees in a child >12 years
- Pathological fracture of the proximal humerus
- Associated injuries, i.e. brachial plexus injury, vascular injury
- In association with other unilateral upper limb fractures
- Multi trauma
9. What is the usual ED management for this fracture?
The usual treatment for this fracture is immobilisation of the shoulder in a sling, body swathe or shoulder immobiliser. Analgesia and thorough neurovascular assessment are essential.
10. What follow-up is required?
Patients should be seen in the fracture clinic or by an interested GP within seven days for follow-up with radiographs to assess further displacement.
11. What advice should I give to parents?
Due to the remodelling potential of this region, the outcome from this fracture is usually excellent. Nonunion is rare and shoulder function usually returns to normal even if there is residual deformity on xray. Mild shortening of the humerus and mild angular malunion are not noticeable cosmetically, and function is unaffected.
Physeal injuries in adolescents are typically Salter-Harris type I and II with very low subsequent growth arrest rates.
12. What are the potential complications associated with this injury?
Complications are rare and usually due to associated soft tissue and neurological injuries, i.e. brachial plexus.
Mild malunion can occur but is not a functional problem.
Nonunion is rare.
See
fracture clinics for other potential complications
References (ED setting)
Bahrs C, Zipplies S, Ochs BG, et al. Proximal humeral fractures in children and adolescents. J Pediat Ortho 2009; 29(3): 238-42.
Beaty JH . Fractures of the proximal humerus and shaft in children. Am Acad Ortho Surg Instr Course Lect. 1992; 41: 369-72.
Erikson M, Frick S. Fractures of the proximal radius and ulna . In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.405-45.
Herring JA. Upper extremity injuries. In Tachdjian's Pediatric Orthopedics, 4th Ed. Saunders, Philadelphia 2008. p.2432-36.
Landin LA. Epidemiology of children's fractures. J Pediat Ortho B 1997; 6(2): 79-83.
Manning Ryan, L. Proximal Humeral Fractures in Children.
http://www.uptodate.com/contents/proximal-humeral-fractures-in-children. 2012; Retrieved 19 April 2012.
Pahlavan S, Baldwin K, Pandya N, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: a systematic review. J Child Ortho 2011; 5 (3) : 187-94.
Pediatric Orthopaedic Society of North America. Fracture of the proximal humerus.
www.posna.org/education/StudyGuide/fracturesOfTheProximalHumerus.asp. 2012; Retrieved 19 April 2012.
Pring M, Wenger D, Rang M. Elbow-proximal radius and ulna. In Rang's Children's Fractures, 3rd Ed. Rang M, Pring ME, Wenger DR (Eds). Lippincott Williams & Wilkins, Philadelphia 2005. p.119-34.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network. To provide feedback, please email
rch.orthopaedics@rch.org.au