1. Summary
- Dislocation of the patella is a relatively common injury in the active adolescent population and usually a traumatic event associated with either an awkward fall or direct trauma to the patella itself.
- Almost all dislocations are lateral in nature and are most easily reduced by simple extension of the knee, with medial pressure on the patella - analgesia may be required.
- Some patients will present with spontaneous reduction having occurred pre-hospital. They may relate a history of resolved knee deformity following a twisting injury. Examination findings may be of knee effusion with tenderness medial to the patella. Examination of the other knee may show a mobile patella or hypermobility. The same investigation and follow up advice applies to these patients.
- When the patella dislocates it may damage the articular cartilage resulting in chondral scuffing or an osteochondral fracture from either the lateral femoral condyle or patella itself.
- Patients who sustain a traumatic dislocation are at risk of developing recurrent patellar instability and therefore require knee rehabilitation which includes proprioceptive exercises and VMO strengthening
2. How are they classified
- Acute first time dislocation
a.With unstable osteochondral fracture
b.Without unstable osteochondral fracture
- Recurrent dislocation
a.With identifiable anatomical abnormality
b.Without identifiable anatomical abnormality
3. How common are they and how do they occur?
Most acute patellar dislocations occur in athletically active children with an incidence in the 10- to 17-year age group (29 per 100 000) without a clear gender predilection.
It is the second most common cause of a knee haemarthrosis second only to ACL injury
The patella usually dislocates laterally when the knee is subjected to a valgus force with the foot firmly planted and the femur internally rotates. Occasionally a direct blow to the patella will produce a dislocation.
Recurrent dislocation may be related to damage to the medial patellofemoral ligament, abnormal shape / site of the patella, shape of the trochlear groove or a combination of these. Hypermobility of the joint can also lead to recurrent dislocation.
4. What do they look like - clinically?
Many patients will present with a swollen painful knee without the appearance of a dislocation as the patella has either reduced spontaneously or been reduced indirectly.
If the patella is dislocated the medial femoral condyle looks prominent and there is usually an obvious lateral bulge of the displaced patella making the whole of the front of the knee look flat. The knee is generally in a flexed position.
There is usually considerable swelling present and there may be local tenderness over the medial patellar facet or lateral condyle indicating trauma to these regions. There may be a palpable rent where the medial capsule and medial patellofemoral ligament are torn or avulsed.
The knee should be thoroughly assessed for instability after the patellar dislocation has been reduced. This can be difficult as the knee can be very painful to move.

Figure 1: An intact medial Patellofemoral Ligament (MPFL)
5. What radiological investigations should be ordered?
It is best to ensure that the patellar is reduced before taking radiographs as the films are not so much for checking the patellar position but for identifying osteochondral fragments
With appropriate analgesia AP, lateral, and skyline images should be obtained. Each view should be carefully reviewed for any osseous abnormality no matter how small. A small osseous lesion may represent a large chondral defect. Commonly this is seen on the medial aspect of the patella in the skyline view or in the joint in the other views.
6. What do they look like on X-ray?
If the patella is dislocated it is obvious on the radiograph. Most patients will have at least an effusion but a number will have a lipo-haemarthrosis ( fat fluid level in the knee) that indicates either a significant soft tissue injury or an osteochondral fracture

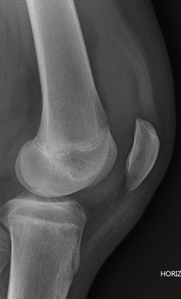
Figure 2: Lateral subluxation of patella alta

Figure 3: Patellar slightly subluxated and osteochondral lesion below lateral condyle in the joint.
The patella usually remains somewhat subluxated on the initial radiographs due to the combination of haemarthrosis and ligament injury

|
|
Figures 4 & 5: haemarthrosis following patella dislocation, AP and lateral views |
Patients sustaining a dislocated patella for the first time should undergo an outpatient MRI examination of the knee even if the radiological evaluation is normal. Osteochondral fractures occur in 25 -75% of cases and usually require surgical management. The MRI scan is not urgent and in most cases can be performed as an outpatient investigation within 7 days of the injury. It is very reasonable for this to be arranged in a primary care setting.
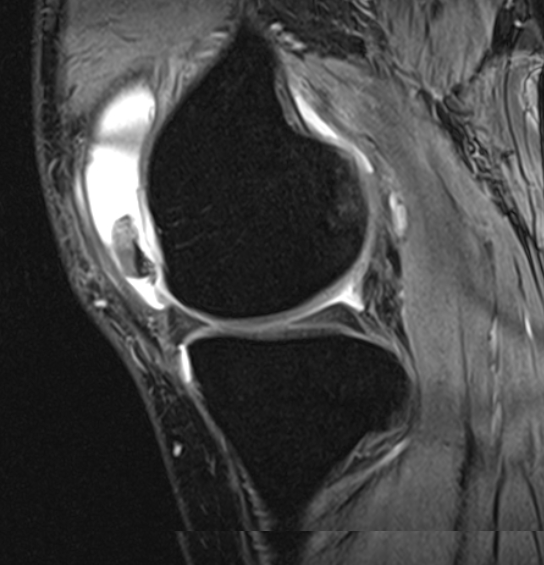
Figure 6: Large osteochondral fragment anterior aspect of knee on MRI
7. When is operative treatment required?
The presence of a significant chondral or osteochondral fragment on MRI requires operative treatment to remove, reattach or replace the fragment.
Acute reconstruction of the torn soft tissue structures (most notably the medial patellofemoral ligament) is usually not required as this does not appear to influence the long term outcome of an acute dislocation.
8. Do I need to refer to orthopaedics now?
Orthopaedic referral is required if the patella does not reduce, loose body or osteochondral fragment is identified on the x-ray or the patient has suffered multiple dislocations despite having good physiotherapy for several months.
Patients with small lesions can be referred during or after rehabilitation for assessment for arthroscopic removal of the fragment
If there is no lesion present patients may rehabilitate (via physiotherapy) and only be referred for ongoing instability or locking
9. What is the usual ED management for this condition?
If the patella is dislocated on arrival adequate analgesia should be given (penthrane or N2O) and the knee gently extended, with medial pressure on the patella, until the dislocation is reduced.
The patients should be thoroughly examined for associated injuries such as haemarthrosis, torn ligaments and avulsion fractures
High quality radiographs (3 views) should be obtained and examined carefully.
If the patient has a tense haemarthrosis aspiration of the knee should be considered after consultation with orthopaedics. In this situation an osteochondral injury is likely and the MRI scan should be obtained early.
An elastic stocking (tubigrip) of appropriate size should be applied to the whole limb and the knee iced
The knee should be splinted in full extension ideally with a hinged knee brace locked in full extension - with alternative of a zimmer knee splint - for a period of three weeks. Sometimes patients are unable to fully straighten the knee and locking a hinged brace at 20-30 deg may be more comfortable. The brace may be removed for bath or shower. Oral analgesia should be taken regularly and ice to the knee will help reduce swelling and pain.
MRI should be performed within 7 days in the first-time dislocator, and if an osteochondral lesion or loose body identified an orthopaedic opinion obtained early as when surgery is necessary it is best performed early.
Patients without bony or cartilage injury should be referred to a physiotherapist for a knee rehabilitation program after the initial period of immobilisation. This program needs to focus on range of motion, muscle strengthening (particularly VMO) and proprioception exercises.
10.What follow up is required?
Patients should be followed up by their GP within three days of the injury and either have the MRI scan performed locally or return to the hospital for imaging.
The risk of dislocation is increased six fold if there is a history of a contralateral dislocation therefore those patients should be referred to Orthopaedic Clinic.
Patients with problems of frequent recurrent dislocation should be referred to orthopaedics for consideration of surgical stabilisation.
11. What advice should I give to parents?
Parents should be told that this is a significant injury and that the MRI scan is an important part of the management. Adherence to the discharge instructions and obtaining good physiotherapy is the key to reducing the chance of long term instability.
If their child has pain that is not settling with oral analgesia and splintage they should be reviewed.
Ideally the patient will be encouraged to perform straight-leg raises in the splint to prevent excessive VMO wasting.
12.What are the potential complications associated with this injury?
Acute patellar dislocation is a significant knee injury that in the otherwise normal knee results in recurrent instability in over a third of patients.
Recovery periods are prolonged and nearly half of the affected patients never return to sport as the knee continues to feel unstable.
Unrecognised loose bodies within the knee may cause locking of the joint and osteochondral injuries may result in ongoing joint pain and the development of early arthritis.
13. References
- Seitlinger, G., Ladenhauf, H., Wierer, G. (2018). What is the chance that a patella dislocation will happen a second time Current Opinion in Pediatrics 30(1), 65-70.
https://dx.doi.org/10.1097/mop.0000000000000568
- Zhang, G., Zheng, L., Shi, H., Ji, B., Feng, Y., Ding, H. (2017). Injury patterns of medial patellofemoral ligament after acute lateral patellar dislocation in children: Correlation analysis with anatomical variants and articular cartilage lesion of the patella European Radiology 27(3), 1322-1330.
https://dx.doi.org/10.1007/s00330-016-4473-5
- Duthon, V. (2015). Acute traumatic patellar dislocation Orthopaedics & Traumatology: Surgery & Research 101(1), S59-S67.
https://dx.doi.org/10.1016/j.otsr.2014.12.001
- Jain, N., Khan, N., Fithian, D. (2011). A Treatment Algorithm for Primary Patellar Dislocations Sports Health: A Multidisciplinary Approach 3(2), 170-174.
https://dx.doi.org/10.1177/1941738111399237
Last updated October 2020