Fracture Guideline Index
See also:
Distal radius and / or ulna metaphyseal fractures - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like - clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
-
Parent information fact sheet
1. Summary
|
Fracture type
|
ED management
|
Follow-up
|
|
Buckle injury

|
Below-elbow fibreglass/plaster backslab or removable wrist splint for 3 weeks
|
!
|
Check that both cortices are intact on the anteroposterior (AP) and lateral x-ray.
|
Provide parent with buckle injury fact sheet.
|
No follow-up by GP or fracture clinic is required.
No follow-up x-ray is needed
|
|
Complete - undisplaced or minimally displaced fractures
|
Refer to
acceptable angulations
Below-elbow cast for 6 weeks
|
Fracture clinic within 7 days with x-ray
|
|
Complete - displaced fractures

|
Refer to
acceptable angulations
Closed reduction with immobilisation in below-elbow cast for 6 weeks
For young children, above-elbow casts may be applied
|
Fracture clinic within 7 days with x-ray
|
2. How are they classified?
Distal radius metaphyseal fractures can be classified according to:
- displacement (whether undisplaced or displaced)
- bone involvement (radius only, both radius and ulna)
- fracture type:
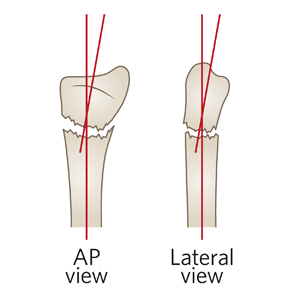
Buckle injury: Compression injury failure of bone resulting in the cortex bulging outwards (unilateral or bilateral). Also known as a torus injury. Although there is a disruption to the cortical bone, the integrity of the bone is minimally compromised, resulting in different patient management from other fractures
See fracture education module for more information
|

|

|
|
Anteroposterior (AP) view
|
Lateral view
|
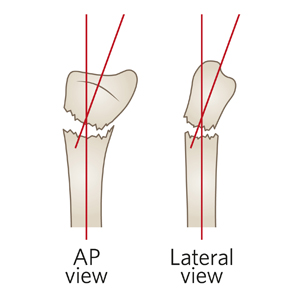
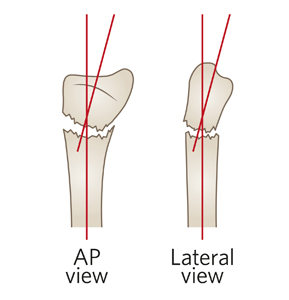
Complete: A fracture that extends through both cortices. Most complete metaphyseal fractures involve both the radius and ulna. The radius is commonly a complete fracture. The ulna may have a complete fracture, greenstick fracture, or a plastic deformity
|
|

|
|
AP view
|
Lateral view
|
3. How common are they and how do they occur?
Metaphyseal fractures have a peak incidence during the adolescent growth spurt (girls aged 11-12 years, boys 12-13 years) due to weakening through the metaphysis with rapid growth.
Up to 13% incidence of other arm injuries (hand, forearm, elbow) occur on the same side.
The most common mechanism of injury is a fall on an outstretched hand. Extension of the wrist at the time of injury causes the distal fragment to be displaced dorsally (posteriorly). Volar (anterior) displacement of the distal fragment is usually the result of a fall on a flexed wrist.
These injuries can occur in conjunction with more proximal forearm fractures, such as Monteggia fracture-dislocations, supracondylar humeral fractures and hand fractures.
4. What do they look like - clinically?
There is usually pain and tenderness directly over the fracture site, and limited range of motion in the wrist and hand.
Deformity depends on the degree of fracture displacement. Buckle injuries present with no or minimal deformity. Buckle injuries are often misdiagnosed as a wrist sprain. An x-ray of the wrist should be ordered to clarify the diagnosis.
5. What radiological investigations should be ordered?
A 'wrist x-ray' request will provide AP and lateral views of the distal forearm and wrist. If the injury is to the mid forearm or the pain is poorly localised, a 'forearm x-ray' should be ordered. Avoid ordering 'x-ray arm' as it is better to have images focused to the region of local tenderness. If there are any elbow joint symptoms, an 'elbow x-ray' should be ordered as some fractures around the elbow can be difficult to detect.
6. What do they look like on x-ray?
Buckle injury


Figure 1: Lateral and AP x-ray of a five year old who sustained a buckle injury of the distal radius.Buckle injuries are often subtle radiographically.They are best viewed on the lateral x-ray. Bilateral or unicortical cortical bulging can occur.
|
!
|
Minimally displaced complete metaphyseal fractures can be mistaken for buckle injuries (Figure 2). These fractures are potentially unstable and need to be managed in a well moulded cast.
 
Figure 2: Six year old with complete metaphyseal fracture. On the lateral view, there is a minimally displaced radial metaphysis, which could be mistaken for a buckle fracture. However on the AP view, it shows that both cortices are broken (i.e. it is a complete fracture).
|
Complete fracture


Figure 3: AP and lateral x-ray of 15 year old with complete metaphyseal fracture of radius and ulna. Most metaphyseal fractures displace posteriorly.
7. When is reduction (non-operative and operative) required?
|
!
|
As a rule of thumb, if the deformity is clinically visible, reduction may be indicated.
|
Acceptable angulations are dependent on the age of the child. Table 1 shows the acceptable angulations for distal radius metaphyseal fractures. Fractures angulated more than these values usually need to be reduced. Angulation in the coronal plane (as seen on AP x-ray) is less tolerated as it does not remodel as well as angulation in the sagittal plane (as seen on the lateral x-ray).
X-rays should be taken post-reduction. Angles should be within the same parameters for acceptable angulation.
Table 1: Acceptable angulations for distal radius metaphyseal fractures.
|
Age
|
Acceptable angulation
|
|
0-5 years
|
<20 degrees
|
|
5-10 years
|
<15 degrees
|
|
10-15 years*
|
<10 degrees
|
* As girls mature earlier, acceptable angulations may be less.
Bayonet apposition is acceptable in children up to age of six as long as angulation alignment parameters are acceptable. For children aged 6-10 years, if the fracture is still in bayonet position after reduction, ask the orthopaedic on call service to review the post-reduction x-rays to check if the position is acceptable. Children aged 11 years and above need to have apposition at the fracture site.
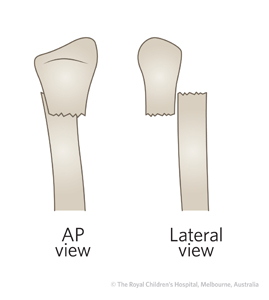

Figure 4: Bayonet apposition refers to a fracture in which the two bone fragments are aligned side-by-side rather than in end-to-end contact.
8. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- Open fractures
- Fractures with associated neurovascular compromise
- Inability to achieve an acceptable reduction (including if ED is not experienced in fracture reduction, splinting or casting)
- An associated arm fracture in the same upper limb or opposite limb
9. What is the usual ED management for this fracture?
Treatment options depend on the fracture type, age of patient (years of remaining growth) and the amount of displacement (Table 2).
Table 2: ED management of metaphyseal distal radius fracture.
|
Fracture type
|
Type of reduction
|
Immobilisation method & duration
|
|
Buckle injury
|
No reduction required
|
Below-elbow fibreglass/plaster backslab or removable wrist splint for 3 weeks
|
|
Complete - undisplaced or minimally displaced fractures
|
No reduction required
|
Below-elbow cast for 6 weeks
|
|
Complete - displaced fractures
|
Closed reduction
This fracture is suitable for a
local anaesthetic, manipulation and plaster (LAMP)or
procedural sedation in the ED, provided that there are appropriate resources and accredited personnel at your health service
|
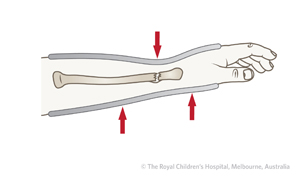
Below elbow plaster cast for 6 weeks. For young children, above-elbow casts may be applied
Fractures where the distal fragment is angulated dorsally should have a cast with three point moulding with slight wrist flexion
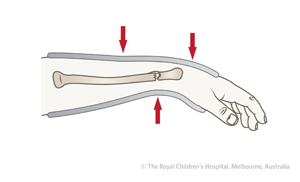
Fractures where the distal fragment is angulated volarly should have casting with three point moulding with slight wrist extension
|
10. What follow-up is required?
- Buckle injury: No follow-up is required by GP or fracture clinic. Radiographic follow-up is not required. Instruct parent to remove backslab or splint in 3 weeks. Provide parent with buckle injury fact sheet. Ensure parents understand signs for concern (ongoing pain, etc.).
- Complete fractures: All complete fractures should be reviewed in fracture clinic within 7 days with an x-ray in cast at first appointment.
11. What advice should I give to parents?
Distal metaphyseal fractures of the radius have very good remodelling potential because of the proximity to the growth plate. There is a very low risk of growth arrest.
For complete metaphyseal displaced fractures and fractures involving both the radius and ulna, the need for close follow-up should be emphasised due to the risk of loss of reduction.
12. What are the potential complications associated with this injury?
The main early complication is loss of reduction. One in ten (10%) will lose position and will need a re-reduction. Contributing factors are poor cast technique and residual angulation/displacement after the initial reduction. Loss of position and the opportunity for re-reduction can only happen with appropriately timed follow-up.
Another complication is compartment syndrome due to restriction by cast.
See
fracture clinics for other potential complications.
13. Parent information fact sheet
References (ED setting)
Bae D. Pediatric distal radius and forearm fractures. J Hand Surgery 2008; 33: 1911-23.
Bohm ER, Bubbar V, Yong Hing K, Dzus A. Above and below the elbow plaster casts for distal forearm fractures in children: A randomized controlled trial. J Bone Joint Surg Am 2006; 88: 1-8.
Crawford SN, Lee LSK, Izuka SH. Closed treatment of overriding distal radial fractures without reduction in children. J Bone Joint Surg Am 2012; 94: 246-52.
Herring JA. Upper extremity injuries. In Tachdjian's Pediatric Orthopedics, 4th Ed. Saunders, Philadelphia 2008. p.2536-68.
Kennedy SA, Slobogean GP, Mulpuri K. Does degree of immobilization influence refracture rate in the forearm buckle fracture? J Pediat Ortho B 2010; 19(1): 77-81.
Rang M, Stearns P, Chambers H. Radius and ulna. In Rang's Children's Fractures, 3rd Ed. Rang M, Pring ME, Wenger DR (Eds). Lippincott Williams & Wilkins, Philadelphia 2005. p.135-50.
Stutz C, Mencio G. Fractures of the distal radius and ulna: metaphyseal and physeal injuries. J Pediat Ortho 2010; 30: S85-9.
Waters PM, Bae DS. Fractures of the distal radius and ulna. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.292-346.
Webb GR, Galpin RD, Armstrong DG. Comparison of short and long arm plaster casts for displaced fractures in the distal third of the forearm in children.J Bone Joint Surg Am 2006, 88(1): 9-17.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network.
To provide feedback, please email rch.orthopaedics@rch.org.au