Fracture Guideline Index
See also:
Distal radial physeal fractures - Fracture clinics
-
Summary
-
How are they classified?
-
How common are they and how do they occur?
-
What do they look like- clinically?
-
What radiological investigations should be ordered?
-
What do they look like on x-ray?
-
When is reduction (non-operative and operative) required?
-
Do I need to refer to orthopaedics now?
-
What is the usual ED management for this fracture?
-
What follow-up is required?
-
What advice should I give to parents?
-
What are the potential complications associated with this injury?
-
Parent information fact sheet
1. Summary
|
Salter-Harris fracture type and frequency
|
Complications
|
ED management
|
Follow-up
|
|

Common
|
Rarely associated with growth disturbance
|
Undisplaced: Below-elbow plaster backslab or removable splint for 4 weeks
Displaced: Closed reduction and below-elbow plaster backslab for 4 weeks
Reduction is not advisable after ≥5 days of initial injury
Refer to orthopaedics if unable to perform closed reduction
Provide parent with
fracture of the wrist fact sheet
|
Undisplaced and displaced:
Fracture clinic within 5 days of immobilisation
|
|
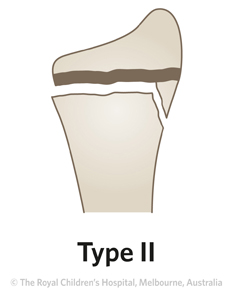
Most common
|
Rarely associated with growth disturbance
|
As per Salter-Harris type I
|
As per Salter-Harris type I
|
|
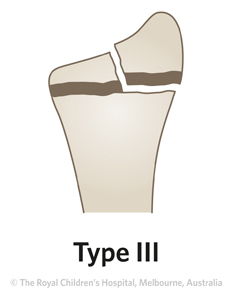
Rare
|
Medium risk of growth disturbance
|
Refer to orthopaedics - usually requires open reduction and internal fixation (ORIF)
|
Fracture clinic as per post-operative orders
|
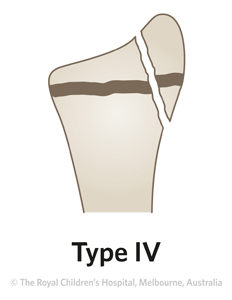
|
Rare
|
High risk of growth disturbance
|
As per Salter-Harris type III
|
Fracture clinic as per post-operative orders
|
|
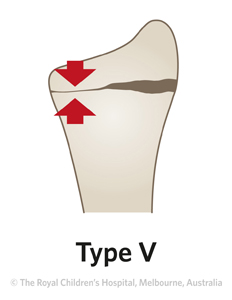
Very rare
|
High risk of growth disturbance
|
Not seen in acute injury; diagnosis usually made in retrospect
|
Fracture clinic as per post-operative orders
|
2. How are they classified?
Physeal fractures are classified by the Salter-Harris classification and whether the radius, ulna, or both bones are injured.
Radial physeal fractures can occur in isolation or be associated with an ulna fracture (greenstick, physeal or styloid).
3. How common are they and how do they occur?
The peak age for injury to the growth plate is in the pre-adolescent growth spurt. The Salter-Harris type II fracture is the most common type. Distal radial physeal fractures are uncommon in children younger than five years.
The most common mechanism of injury is a fall on an outstretched hand (Figure 1). Extension of the wrist at the time of injury causes the distal fragment to be displaced dorsally (posteriorly). Commonly there is an associated ulna fracture (greenstick, physeal or styloid).
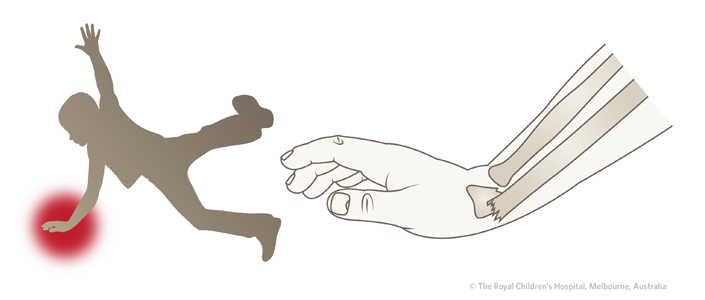
Figure 1: Dorsal (posterior) displacement of the distal fragment is usually the result of a fall on an extended wrist.
4. What do they look like -clinically?
There is usually pain and tenderness directly over the fracture site, and limited range of motion in the wrist and hand. There may be little, if any swelling. Deformity depends on the degree of physeal displacement.
|
!
|
Remember to always examine the elbow for associated injuries
|
5. What radiological investigations should be ordered?
Appropriate analgesia and splinting for pain relief prior to x-ray is required.
A 'wrist x-ray' request will provide anteroposterior (AP) and lateral views of the distal forearm and wrist.
If the injury is to the mid forearm or the pain is poorly localised, a 'forearm x-ray' should be ordered. Avoid ordering 'x-ray arm' as it is better to have images focused to the region of local tenderness. If there are any elbow joint symptoms, an 'elbow x-ray' should be ordered as some fractures around the elbow can be difficult to detect.
If, in an older child with a painful wrist (as a result of a fall on an outstretched hand), there is no distal radial fracture seen on x-ray, consider the possibility of a scaphoid fracture. Examine for tenderness in the anatomical snuff box and consider ordering scaphoid views.
6. What do they look like on x-ray?
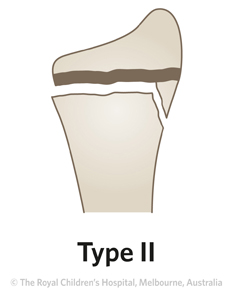
Table 1: Salter-Harris fracture classification.
|
Classification
|
X-ray
|
|

|

.jpg?n=1333)
.jpg)
Figure 2: AP and lateral x-ray of 10 year old girl with Salter-Harris type I fracture. A Salter-Harris type I fracture occurs through the growth plate. These fractures are difficult to see on x-ray and are primarily diagnosed on clinical findings. The key clinical sign is localised tenderness.
|
|
|

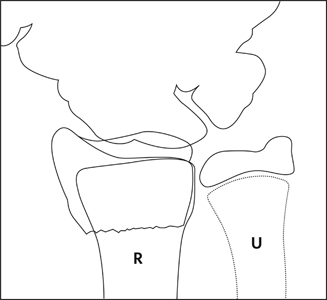

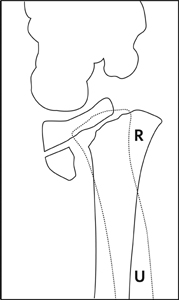
Figure 3: AP and lateral x-ray of 13 year old boy with Salter-Harris type II fracture. On lateral view, the fracture pattern through the growth plate is more evident.
|
|
|
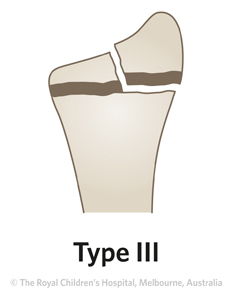
Salter-Harris type III fractures are rare.
|
|
|
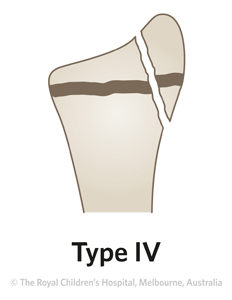
Salter-Harris type IV fractures are very rare.
|
|
|

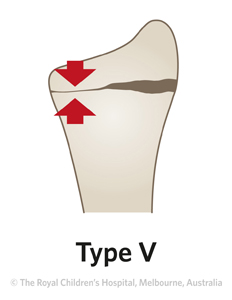
Figure 4: A type V fracture will not be visible in an acute injury but is usually recognised later because of growth arrest and progressive deformity. This AP and lateral x-ray shows a bony bar extending across the growth plate of the distal radius, indicating the presence of a growth arrest.
|
7. When is reduction (non-operative or operative) required?
In general, distal radial physeal fractures that are angulated >20 degrees (as seen on the lateral x-ray) need to be reduced. Angulation is less acceptable if there is less than two years of growth remaining. More angulation can be accepted in children less than eight years old and those presenting late.
|
!
|
For patients who have a delayed presentation of physeal fracture >5 days, it is not advisable to attempt closed reduction, as this increases the risk of growth plate injury. These patients should be discussed with the orthopaedic service.
|
Repeat x-rays should be taken after reduction and immobilisation.
Fractures with angulation up to 20 degrees post-reduction (as seen on lateral x-ray) should remodel if there is two years or more of growth remaining.
8. Do I need to refer to orthopaedics now?
Indications for prompt orthopaedic consultation include:
- Fractures with associated neurovascular compromise
- Open fractures
- Salter-Harris types III and IV
- Inability to achieve an acceptable reduction (including if ED is not experienced in paediatric fracture reduction, splinting or casting)
- An associated fracture in the same upper limb
9. What is the usual ED management for this fracture?
Treatment can be determined according to the Salter-Harris classification (Table 2).
Table 2: ED management of distal radial physeal fractures.
|
Fracture type
|
Type of reduction
|
Immobilisation method & duration
|
|
Type I and II - undisplaced
|
No reduction required
|
Below-elbow plaster backslab or removable splint for 4 weeks
|
|
Type I and II - displaced
|
Closed reduction
This fracture is suitable for a
local anaesthetic manipulation and plaster (LAMP) or
procedural sedation in the ED, provided that there are appropriate resources and accredited personnel at the health service
|
Below-elbow plaster cast for 6 weeks. For young children, above-elbow casts may be applied
|
✓
|
The quality of the reduction and achievement of a well moulded cast is more important than the length of the cast.
|
Fractures where the distal fragment is angulated dorsally should have a cast with three point moulding with slight wrist flexion
Fractures where the distal fragment is angulated volarly should have casting with three point moulding with slight wrist extension
|
|
Type III and IV - all
|
Splint and refer to the nearest orthopaedic on call service
Prompt open reduction and internal fixation (ORIF) is usually required
|
Splint and refer to the nearest orthopaedic on call service
|
10. What follow-up is required?
All physeal fractures should have follow-up care arranged in a fracture clinic within five days, with an x-ray at that visit.
11. What advice should I give to parents?
For all Salter-Harris type I and II injuries, a fracture clinic review is required within five days with x-ray. Provide instructions for elevation and close monitoring of swelling.
The wrist has extensive remodelling potential. The risk of physeal arrest is rare in young children but the risk is higher if the child is near the end of growth. Salter-Harris type I and II injuries rarely lead to growth problems. The risk of growth arrest is higher in Salter-Harris type III, IV and V.
12. What are the potential complications associated with this injury?
|
!
|
For patients who have a delayed presentation of physeal fracture >5 days, it is not advisable to attempt closed reduction as this increases the risk of growth plate injury. These patients should be discussed with the orthopaedic service.
|
Other early complications include:
- Compartment syndrome due to restriction by cast
- Median nerve neuropathy
See
fracture clinics for other potential complications.
13. Parent information fact sheet
References (ED setting)
Accabled F, Foster BK. Management of growth plate injuries. In Children's Orthopaedics and Fractures,3rd Ed.Benson M, Fixsen J, Macnicol M, Parsch K (Eds). Springer, London2010. p.687-99.
Bae D. Pediatric distal radius and forearm fractures. J HandSurgery 2008; 33: 1911-23.
Lee B, Esterhai JL Jr, Das M. Fracture of the distal radial epiphysis: Characteristics and surgical treatment of premature, post-traumatic epiphyseal closure. Clin Ortho Relat Res 1984; 185: 90-6.
Price CT, Flynn JM. Management of fractures. In Lovell and Winter's Pediatric Orthopaedics, 6th Ed,Vol 2. Morrissy RT, Weinstein SL (Eds). Lippincott, Philadelphia 2006. p.1473-74.
Rang M, Stearns P, Chambers H. Radius and ulna. In Rang's Children's Fractures, 3rd Ed. Rang M, Pring ME, Wenger DR (Eds). Lippincott Williams & Wilkins, Philadelphia 2005. p.135-50.
Stutz C, Mencio G. Fractures of the distal radius and ulna: Metaphyseal and physeal injuries. J Pediat Ortho 2010; 30:S85-9.
Waters PM, Bae DS. Fractures of the distal radius and ulna. In Rockwood and Wilkins' Fractures in Children,7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.292-346.
Feedback
Content developed by Victorian Paediatric Orthopaedic Network.
To provide feedback, please email rch.orthopaedics@rch.org.au