1. Summary
Ankle Sprains are very common injuries, particularly in the older child or adolescent presenting to both the Emergency Department and to Primary Care.
Evaluation consists mostly of excluding an ankle or foot fracture, and assessing stability.
Management for the majority of injuries involves the ‘RICER’ principle (Rest, Ice, Compression, Elevation and referral / Rehab), with gradual re-strengthening exercises. Specialised follow up is required for ‘High’ ankle sprains (syndesmosis injuries).
2. How are they classified
Classification by severity:
Grade I: Stretching of the lateral ligament, no ankle joint instability
Grade II: Partial tear of the lateral ligament/s, no joint instability
Grade III: Complete tear of lateral ligaments, unstable ankle joint.
Classification by location:
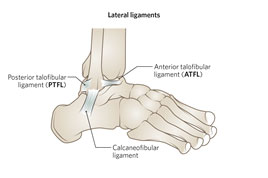
Lateral Ligament (Any combination of Anterior talo-fibular, calcaneo-fibular or Posterior talo-fibular ligaments - usually tears occur in that order with TFL being the least injured)
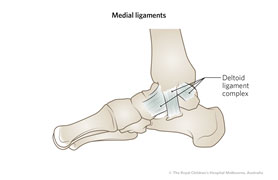
Medial (Deltoid Ligament)
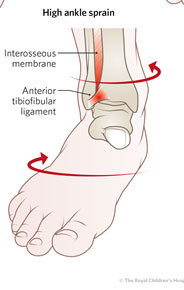
‘High’ (distal tibio-fibular syndesmosis)
3. How common are they and how do they occur?
Ankle sprains are very common injuries presenting to both Emergency Departments and Primary Care physicians. Many occur during sports.
(Most common: >95%)
|
|
|
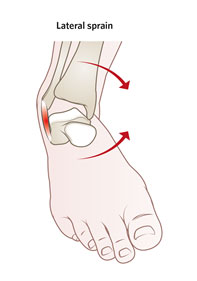
- Combination of ankle inversion and external rotation.
|
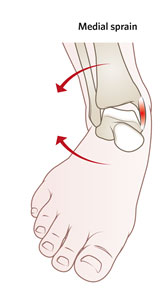
- Forced plantar-flexion and eversion
|
Forced dorsiflexion with eversion and external rotation |
- Lateral swelling
- Tenderness over the ATFL (shown above)
- Pain with ankle inversion
|
- Medial swelling and tenderness
- Pain with ankle eversion
|
Swelling may be subtle
Inability to bear weight, and especially to walk on toes
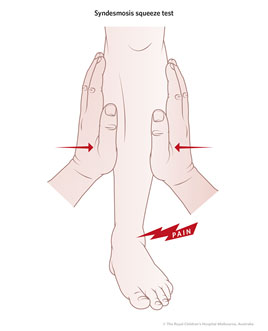
Positive syndesmosis squeeze test (see below) |
4. What do they look like - clinically?
Children will present with a painful ankle, with swelling with or without bruising. Generally patients can walk at least a few steps even if they have initial reluctance to.
Findings particular to each type of ankle sprain are listed in the table above
Though swelling and tenderness are also present in fractures of the ankle or foot, the Ottawa Ankle Rules discussed in point 5 can be used with confidence in the ambulant paediatric population to determine where this needs to be investigated.
Presence of syndesmosis injury (‘High’ ankle sprain) is assessed using a syndesmosis squeeze test. The tibia and fibula are compressed toward one another proximal to the ankle: when this produces pain distally (at the distal tibio-fibular joint) the test is considered positive and the patient should be referred for specialised follow up as outlined in point 10 below.
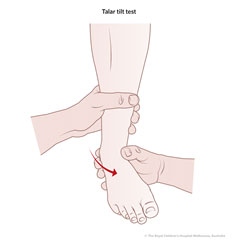
At some point sprained ankles should have joint stability assessed to detect Grade III injuries, using the anterior draw test and the Talar Tilt test. Most children find these difficult to tolerate due to the acute pain of the injury so they are discussed in the follow-up section (point 10) below. As well as ankle instability, Grade III injuries will often show significant swelling and bruising, and weight bearing acutely is often not tolerated.
5. What radiological investigations should be ordered?
Many ankle sprains do NOT require radiological investigations. There are a number of studies demonstrating that the Ottawa ankle rules perform well in children provided they can communicate clearly and were able to walk normally before the injury.
Plain films of the ankle looking for an ankle fracture should be performed if the child has any one of:
- Tenderness of the medial malleolus
- Tenderness at the posterior aspect of the lateral malleolus
- Inability to bear weight both at the time of the injury and for four steps at the time of evaluation
Plain films of the foot should be performed if the child has any one of:
- Tenderness at the navicular
- Tenderness at the base of the 5th metatarsal
All other children presenting with findings suggestive of ankle sprain can be treated without the need for imaging. |
MRI plays no role in acute diagnosis, and only has a role in evaluating children with:
- Chronic ankle instability or persistent pain and swelling persisting beyond a month after the injury, or
- Suspicion of a syndesmosis injury at early follow-up.
Ultrasound is generally not useful as it does not change management.
6. What do they look like on X-ray?
There will be no fracture shown on X-ray, but may be significant soft tissue swelling overlying the lateral malleolus. NB small avulsions injuries of the tip of the lateral malleolus should be treated like a sprain.
Salter Harris 1 injuries of the distal fibula are uncommon and generally if the patient is tender over the lateral malleolar growth plate this is related to an ankle sprain of distal epiphyseal fracture.
7. When is operative treatment required?
There is no role for surgical treatment of the acute injury, including rupture of Anterior tibiofibular ligament.
8. Do I need to refer to orthopaedics now?
No
9. What is the usual ED management for this condition?
Emergency Management of this condition consists of excluding other injuries, with the mainstays of treatment being
- Rest - crutches may be required particularly for Grade III sprains until the patient can walk properly. A backslab may be used for pain relief and comfort for up to a week but mobilisation is then recommended.
- Ice - intermittently, thrice daily for the first 2-3 days after injury for 15-20 mins.
- Compression - with a bandage or tubigrip.
- Elevation - as much as possible, as this will help improve the oedema
- Referral - for physiotherapy or specialist review (sports physician)
The child can weight bear as tolerated starting a few days after the injury to gradually re-strengthen the affected ligaments. (A slightly longer period of immobilisation would be indicated in Grade III injuries)
10. What follow up is required?
A program of rehabilitation is important for prevention of recurrent injuries or chronic instability. This consists of a series of exercises aimed at improving proprioception, single-leg balance and muscular control.
Almost all children with Grade I or II ankle sprain have good long-term outcome. Initial steps for a home-based recovery program are well described in the RCH Kids Health Info sheet on Ankle Sprains. Referral to physiotherapy for oversight of follow up is worthwhile particularly where the child is an athlete keen to return to sport, or if there is a pattern of recurrent injury.
Suspected ‘High’ ankle sprains of the distal tibio-fibular syndesmosis should be referred for specialist follow-up with either sports medicine or orthopaedics.
Testing for Ankle Instability suggestive of Grade III injury:
This assessment has two major components.
- Anterior draw test: Lie the patient on the bed with a support under the knee to bring it into 20-40 degrees of flexion. Cup the heel in one of your hands with the sole resting on your forearm, and stabilise the distal tibia with your other hand. Draw the heel anteriorly, testing for anterior laxity compared with the noninjured side, suggesting instability

- Talar Tilt Test: Sit the patient with the leg hanging over the bed and sit facing the patient. If examining a right ankle injury, grasp the calcaneus in your right hand and stabilise the distal tib-fib with your left.
Starting in full plantar flexion, inversion will test the anterior talofibular ligament.
Starting in full dorsiflexion, inversion will test the posterior talofibular ligament.
Starting in the anatomical position, inversion of the foot will test the calcaneofibular ligament. Eversion from this position will test the deltoid ligament medially.
|
Significant laxity compared with the uninjured ankle is diagnostic for joint instability (Grade III). Sports Medicine or Physiotherapy follow up for these injuries is particularly important, as it often takes 5-10 weeks to make a recovery sufficient to return to sports even with therapy.
11. What advice should I give to parents?
The importance of a graded return to exercise should be emphasised, and the Kids Health Info sheet should be provided.
Early weight bearing as tolerated and participation in rehabilitation exercises produces much better outcomes than a prolonged immobilisation.
Apparently severe ankle sprains should be encouraged to attend follow up for an assessment of stability after the acute injury has settled.
Strapping of ankle brace should be used for return to sport in Grade II or III for at least a 6 month period. This should be in conjunction with a home exercise program.
12. What are the potential complications associated with this injury?
Repeat injury with premature return to competitive sport.
Chronic pain if period of immobilisation following the injury is excessive.
13. References
Browne G and Barnett P. Common Sports-related musculoskeletal injuries presenting to the emergency department; Journal of Paediatric and Child Health 52(2016) 231-236
Boutis, K et al, Radiograph-Negative Lateral Ankle Injuries in Children: Occult Growth Plate fracture or Sprain? JAMA Pediatr 2016;170(1):e154114
Clark, K and Tanner, S. Evaluation of Ottawa ankle rules in children Pediatr Emerg Care 2003; 19(2): 73-8
Gravel, J et al. Prospective validation and head-to-head comparison of 3 ankle rules in a pediatric population, Ann Emerg Med 2009; 54(4):534-540
Myers, Are the Ottawa Ankle Rules helpful in ruling out the need for X-Ray examination in children, Arch Dis Child 2005;90:1309-1311
Runyon, MS. Can we safely apply the Ottawa Ankle Rules in Children?. Acad Emerg Med, 2009;16(4):352-354.