See also
Immigrant Health Guideline – Low Vitamin D
Sun Protection
Vitamin D supplements photoboard
Key points
- Vitamin D is essential for bone and muscle health. Low vitamin D and low calcium and/or phosphate can cause nutritional rickets
- Sunlight is the most important source of vitamin D at all ages
- Vitamin D deficiency is common in risk groups and should be self-managed wherever possible - through education, behaviour change and supplementation as required
- In Australia, nutritional rickets is generally only seen in infants and children with dark skin
Background
- Sunlight (UVB) is the most important source of vitamin D (>90%) through skin synthesis of D3. This varies with
- Skin colour: people with dark skin (
Fitzpatrick types V and VI) require greater UVB exposure compared to people with light skin
- Skin exposure: covering clothing may result in low vitamin D levels
- Season/UVB availability: during winter there may not be enough UVB to maintain adequate vitamin D levels in southerly latitudes. Sunscreens do not result in low vitamin D with normal use
- Only small amounts of vitamin D are available from diet:
- the main natural food source is fish
- breastmilk, despite its other benefits, contains almost no vitamin D
- infant formula is fortified with vitamin D
- In the absence of sun exposure, recommended intakes of vitamin D are:
- 0–12 months old: 400 units daily
- 1–18 years old: 400–600 units daily
- 25-OH-D is used to measure vitamin D status
- The recommended 25-OH-D level is ≥50 nmol/L at all ages and during pregnancy
|
Definitions of vitamin D status |
|
Severe deficiency |
<12.5 nmol/L |
|
Moderate deficiency |
12.5–29 nmol/L |
|
Mild deficiency |
30–49 nmol/L |
|
Sufficient |
≥50 nmol/L |
|
Elevated |
≥250 nmol/L* |
*Toxicity is defined as serum 25-OH-D >250 nmol/L with hypercalcaemia and suppression of parathyroid hormone (PTH)
Assessment
Risk factors
- Lack of skin exposure to sun (time inside, covering clothes)
- Dark skin
- Medical conditions affecting Vitamin D metabolism (obesity, liver/renal failure, severe malabsorption, medications)
Infants: exclusive breastfeeding AND any of: the above risk factors, maternal deficiency or prematurity
History
- Time outdoors and covering clothing
- Dietary history (calcium intake, breastfeeding/formula in infants)
- Previous vitamin D levels and treatment
- a wide range of formulations are available
- check dosing (photoboard) and adherence
- Family understanding
- Non-specific bony/muscular pain, fatigue with exercise
- Poor growth, motor delay and irritability (infants)
- Symptoms of low calcium: muscle cramps, tetany, stridor, seizures (rare beyond 6–12 months of age)
Examination
- Growth parameters, exclusion of other musculoskeletal pathology
-
Fitzpatrick skin type
- Delayed dentition (no teeth by 9 months, no molars by 14 months)
- Rickets:
- long bone deformity (eg genu varum/valgus - if weight bearing)
- widening of wrists/ankles
- delayed anterior fontanelle closure (normally closed by 2 years)
- frontal bossing
- rosary (widening of ribs at costochondral junction)
- increased risk of fracture
Management
Investigation and treatment of low vitamin D
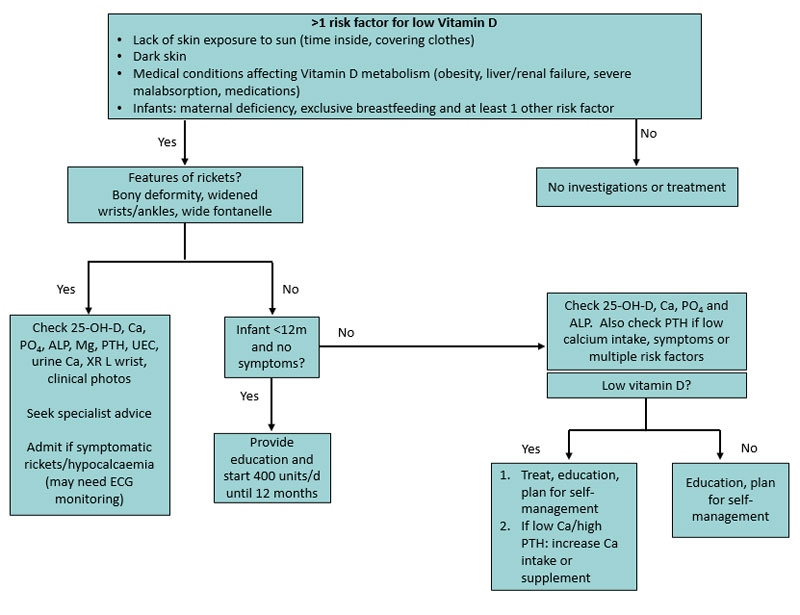
- Breast fed infants
<12 months with other risk factors can usually start supplements (400 units daily) without investigations, provided they do not have symptoms/signs
- Consider admission: symptomatic hypocalcaemia (including tetany, stridor, seizures) or severe rickets
- Specialist review: infants with symptoms/signs, clinical rickets, abnormal serum calcium, or vitamin D deficiency not responding to high dose supplements
Investigations
- Breastfed babies can usually be started on supplements without testing
- Screen children/adolescents with one or more risk factors for low vitamin D (25-OH-D, Ca, PO4, and ALP)
- Also check PTH if low calcium intake, symptoms, or multiple risk factors
- Infants and children with rickets need additional investigations:
- 25-OH-D, Ca, PO4, ALP, Mg, PTH, UEC, urine Ca, PO4, creatinine; X-ray L wrist, clinical photos
- X-ray changes of rickets - osteopenia, metaphyseal widening/splaying/fraying
Treatment
- Children with low vitamin D should be
treated (see table below) to restore their levels to the normal range (≥50 nmol/L)
- There is limited evidence to support high dose treatment in infants
<3 months
- Ensure
adequate calcium intake (see calcium intake table below). Cheese, yoghurt and fortified soy dairy are useful sources of calcium in children who dislike cow milk. Consider supplements if poor intake
- Education on sun protection and
exposure (see sun exposure table below). Children/young people with dark skin can tolerate intermittent sun exposure without sunscreen, although hats/sunglasses are still recommended
- Children with nutritional rickets should be managed under specialist guidance. The minimum recommended dose of vitamin D is 2000 units daily for minimum of 3 months, together with oral calcium 500 mg daily (either via diet or supplements). Phosphate supplements may also be needed
Treatment of low vitamin D
|
Age |
Level (deficiency) |
Treatment
Oral doses D3/colecalciferol
1 microgram = 40 units |
Maintenance/prevention in children with ongoing risk factors |
|
Preterm |
Mild
30–49 nmol/L |
200 units/kg/day, maximum 400 units/day |
200 units/kg/day,
maximum 400 units/day |
|
Moderate or severe
<30 nmol/L |
800 units/day, review after 1 month |
|
<3 months
(term) |
Mild
30–49 nmol/L |
400 units/day for 3 months |
400 units daily |
|
Moderate or severe
<30 nmol/L |
1,000 units/day daily for 3 months |
|
3–12 months |
Mild
30–49 nmol/L |
400 units/day for 3 months |
400 units daily |
|
Moderate or severe
<30 nmol/L |
1,000 units/day for 3 months OR
50,000 units stat and review after 1 month (consider repeating dose) |
|
1–18 years |
Mild deficiency
30–49 nmol/L |
1,000-2,000 units/day for 3 months OR 150,000 units stat |
400–600 units daily, OR
3000–4000 units once weekly, OR
150,000 units at start of Autumn |
|
Moderate or severe
<30 nmol/L |
1,000–2,000 units daily for 6 months OR 3,000–4,000 units daily for 3 months OR 150,000 units stat and repeat at 6 weeks |
- Many hospital pharmacies compound 100,000 units/ml of colecalciferol (Vitamin D3) in oil
- 50,000 units tablets are available for authorised prescribers, community compounding pharmacies or via the Special Access Scheme
- Most adult tablets are 1000 units, the strength of liquid formulations/drops varies widely
Calcium intake
| Age
|
Adequate intake (AI) |
Estimated average requirement (EAR) |
Recommended dietary intake (RDI) |
|
0–6 months |
200 mg |
|
|
|
7–12 months |
270 mg |
|
|
|
1–3 years |
|
360 mg |
500 mg |
|
4–8 years |
|
520 mg |
700 mg |
|
9–11 years |
|
800 mg |
1000 mg |
|
12–18 years |
|
1050 mg |
1300 mg |
See
common food sources of calcium - calcium content
Ongoing monitoring and self-management
- Breastfed infants at risk of low vitamin D should be given 400 units vitamin D daily for at least the first 12 months
- Supplementation is usually not required in fully formula fed infants
- Follow up bloods (25-OH-D, Ca, PO4, ALP, and PTH if previously elevated)
- Not usually required in mild deficiency
- Check at 1 month in infants, at 3 months if older
- Children with risk factors for low vitamin D require ongoing monitoring and a plan to maintain vitamin D and calcium status with behavioural change and supplementation as required
- Provide education and a plan for self-management: consider 400–600 units daily OR 3000–4000 units once weekly over the cooler months (May–August) to avoid need for blood testing and the need for high dose therapy
Consider consultation with local paediatric team
- All children with symptomatic hypocalcaemia or severe rickets (will require admission)
- Children presenting with clinical rickets, abnormal serum calcium, or vitamin D deficiency not responding to high dose supplements (require specialist consultation and should be referred to endocrinology)
Consider transfer when
Care required is beyond the comfort level of the local hospital
Parent information
Additional notes
Vitamin D medications
There are a number of
Vitamin D preparations on the market
Some preparations are highly concentrated (up to 1000 units per drop) and overdose is possible
Check which supplement the family are taking
High dose therapy
- Many local community health centres have high-dose prescribers
- Medical practitioners can obtain Therapeutic Good Administration authorisation to treat patients with high dose Vitamin D (usually 50,000 units D3 capsules)
Authorised prescriber form
Sun exposure
|
Skin colour
|
Light to olive skin
Fitzpatrick type I-IV
|
Naturally dark skin
Fitzpatrick type V-VI
|
|
Infants, children, adolescents
|
Summer or UV index >= 3
|
Avoid sunburn, full sun protection with sunscreen/hat/clothing/shade and sunglasses recommended
|
Avoid sunburn, able to tolerate intermittent sun exposure without sunscreen, hat and sunglasses still recommended
|
|
Encourage active outside play or physical activity during and after school/preschool
|
|
Winter
|
Sun protection recommendations vary with latitude/UV index.
If UV index <3, sun protection not required unless in alpine regions, outside for extended periods or near highly reflective surfaces such as snow/water
|
Sunscreen not needed in Southern states/New Zealand unless near highly reflective surfaces such as snow or water.
It may not be possible to maintain vitamin D levels through sun exposure alone in southern states of Australia/New Zealand
|
|
Encourage active outside play or physical activity during and after school/preschool
|
|
Pregnancy/
Adults
|
Summer
|
6-7 minutes with arms (or equivalent area) exposed mid-morning or mid-afternoon most days of the week, avoid sunburn,
Full sun protection with sunscreen/hat/clothing/shade and sunglasses recommended
|
15-50 minutes with arms (or equivalent area) exposed mid-morning or mid-afternoon most days of the week.
Avoid sunburn.
Intermittent sun exposure without sunscreen can be tolerated but hat and sunglasses still recommended.
|
|
Winter
|
7-40 minutes exposure (depending on latitude) with face arms, and hands exposed at lunchtime most days of the week.
If UV index <3, sunscreen not required unless in alpine regions, outside for extended periods or near highly reflective surfaces such as snow/water
|
Depends on latitude.
Sunscreen not needed in Southern states/New Zealand unless near highly reflective surfaces such as snow or water.
It may not be possible to maintain vitamin D levels through sun exposure alone in southern states of Australia/New Zealand
|
Last Updated September 2020