See also
Sepsis
Acute pain management
Invasive group A streptococcal infections: management of household contacts
Acute upper airway obstruction
Key points
- Viral pharyngitis is the most common cause of sore throat in children
- Group A streptococcus (GAS) is the most frequently implicated bacterial pathogen. It is usually self-limiting, difficult to distinguish from viral infection and empiric antibiotic therapy is not required for most patients
- Children identified to be at high-risk for acute rheumatic fever (ARF) should be treated with antibiotics if they develop a sore throat (irrespective of other clinical features)
Background
- Viral infections are the most common cause of sore throat in children
- GAS pharyngitis is uncommon under 4 years of age
- GAS can cause non-suppurative complications (acute rheumatic fever, post-streptococcal glomerulonephritis) and suppurative complications (peritonsillar abscess, retropharyngeal abscess)
- Despite periodic surges in the incidence of invasive GAS (iGAS), there is no current evidence that treatment of suspected GAS pharyngitis with antibiotics will prevent invasive disease. However, clinicians are encouraged to consider iGAS in children who present with more severe illness and provide appropriate treatment (see Sepsis)
Assessment
Any patient with impending airway obstruction should have minimal handling and be referred early to an experienced clinician for definitive airway management, see Acute upper airway obstruction
History
Examination
Children with signs of acute upper airway obstruction should have minimal examination to not upset the child further
- Hydration status
- Fever
- Oral/pharyngeal ulcers
- Tonsillar exudates, hypertrophy, asymmetry
- Uvula deviation
- Tender anterior cervical lymphadenopathy
- Hepatosplenomegaly (EBV, CMV)
- Features of scarlet fever (GAS toxin response):
- blanching, erythematous, sandpaper-like rash, usually more prominent in skin creases
- flushed face/cheeks with peri-oral pallor
- red strawberry tongue
- confluent petechiae in skin creases (Pastia lines)
Red flags
- Unwell/toxic appearance
- Respiratory distress
- Stridor
- Trismus
- Drooling
- “Hot potato” voice (muffled voice associated with pharyngeal/peritonsillar pathology)
- Torticollis
- Neck stiffness/fullness
In the acutely unwell child consider alternative diagnosis and/or complications of GAS pharyngitis
Management
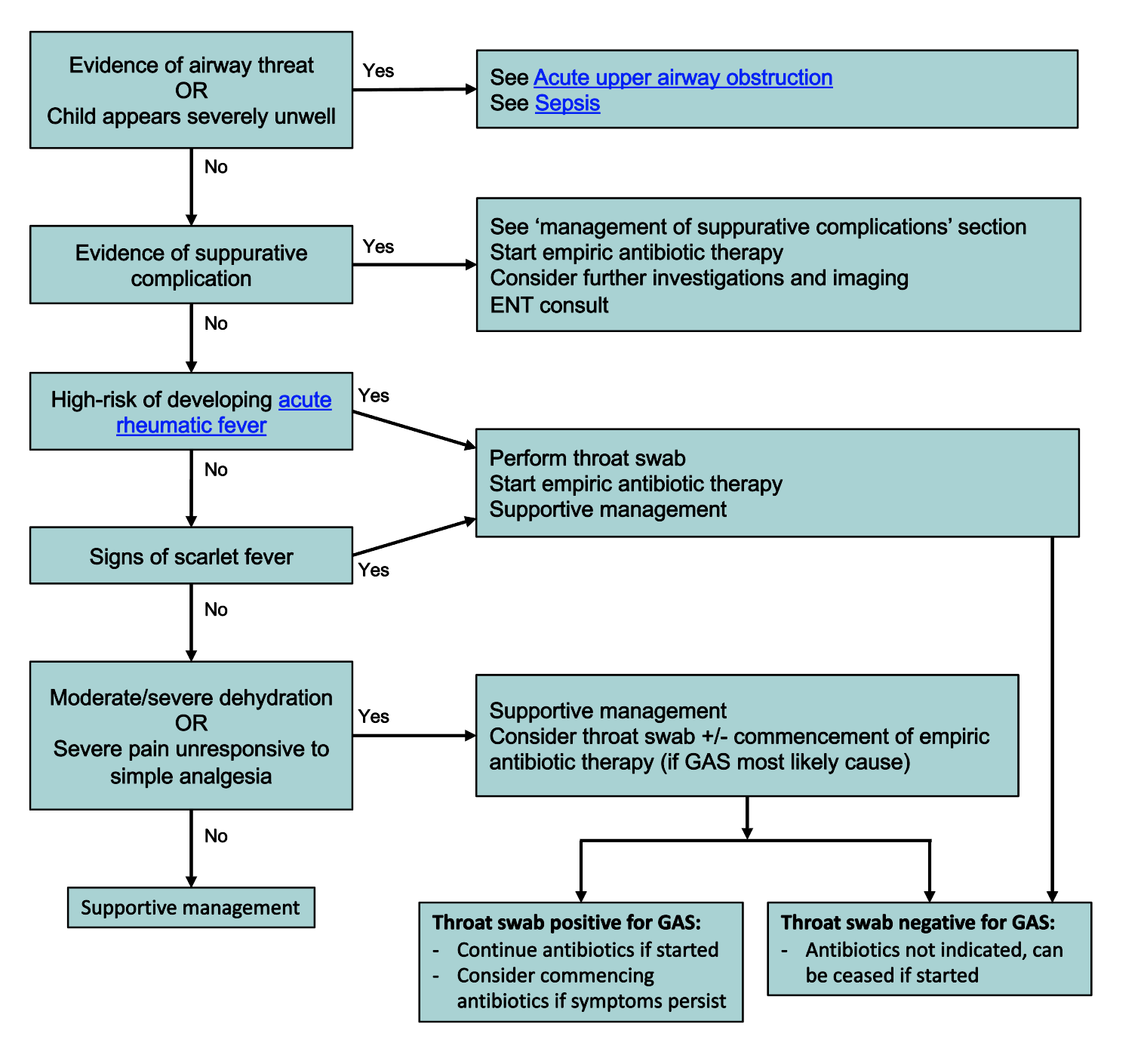
*Supportive management: see treatment section below
Investigations
- Throat swab is not routinely recommended for sore throat
- Consider other investigations if:
- suspected suppurative complications (eg relevant imaging)
- hepatosplenomegaly (FBE, EBV serology, +/- monospot)
- Streptococcal serology has no role in diagnosis of GAS pharyngitis
Treatment
Supportive management is adequate for most sore throats
| Supportive management |
Details |
Simple analgesia |
See Acute pain management |
Corticosteroids |
Consider in children with severe pain unresponsive to simple analgesia
- dexamethasone 0.15 mg/kg (max 10 mg) oral/IV/IM as a single dose, or
- prednisolone 1 mg/kg (max 50 mg) oral as a single dose
|
Hydration |
See Dehydration |
Antibiotic therapy for suspected GAS pharyngitis
Empiric antibiotic treatment of all children presenting with a sore throat is not recommended (see management flow chart above). Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns. Refer to local guidelines
Antibiotic |
Route |
Dose |
Duration |
Phenoxymethylpenicillin |
Oral |
15 mg/kg (max 500 mg) BD |
10 days |
Amoxicillin (second line therapy for improved oral adherence) |
Oral |
50 mg/kg (max 1 g) daily |
10 days |
Poor adherence or oral therapy not tolerated |
Benzathine benzylpenicillin
(for administration, see Pain management information for health professionals) |
IM |
<10 kg 450,000 units (0.9 mL)
10-20 kg 600,000 units (1.2 mL)
>20 kg 1,200,000 units (2.3 mL) |
Single dose |
Hypersensitivity to penicillins (excluding immediate hypersensitivity) |
Cefalexin |
Oral |
20 mg/kg (1 g) BD |
10 days |
Immediate hypersensitivity to beta-lactams |
Azithromycin |
Oral |
12 mg/kg (max 500 mg) daily |
5 days |
Management of suppurative complications
Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns. Refer to local guidelines
Features |
Management |
Peritonsillar abscess (Quinsy)
Fever, odynophagia, dysphagia (pooling/drooling), “hot potato” voice, trismus, peritonsillar swelling/erythema, uvula deviation |
Refer to ENT for consideration of drainage
Antibiotics:
- Benzylpenicillin 50 mg/kg (max 1.2 g) IV 6 hourly
Switch to oral therapy:
- Phenoxymethylpenicillin 15 mg/kg (max 500 mg) oral BD to complete a total of 10 days of therapy (IV + oral inclusive)
|
Retropharyngeal/parapharyngeal abscess
Fever, odynophagia, dysphagia, neck swelling/tenderness
(particularly in young infants), torticollis, limitation of neck extension, retropharyngeal bulge |
Refer to ENT for consideration of imaging and ongoing management
Investigations:
- Lateral neck X-ray: normal X-ray does not exclude the diagnosis
- CT with IV contrast is the imaging modality of choice when required. (Should only be performed with advanced airway management available)
Antibiotics:
- Amoxicillin with clavulanic acid 25 mg/kg (max 1 g) IV 8 hourly (dosing based on amoxicillin component)
Switch to oral therapy:
- Amoxicillin with clavulanic acid 22.5 mg/kg (max 875 mg) oral bd (dosing based on amoxicillin component)
|
Epiglottitis/Bacterial tracheitis
Abrupt onset, respiratory distress, high grade fever, toxic looking, odynophagia, dysphagia, stridor, muffled “hot-potato” voice, tripod position with neck extension, cervical lymphadenopathy
Increased risk in children unimmunised to Haemophilus influenzae type B (HiB)
|
Minimising distress:
- Defer all unnecessary examination/procedures/imaging until advanced airway management available
- Early ICU/anaesthetic/ENT review
Antibiotics:
- Ceftriaxone 50 mg/kg (max 2 g) IV/IM daily for 5 days
Consider:
- Dexamethasone 0.15 mg/kg (max 10 mg) oral/IV/IM/ stat, repeat in 24 hours prn
|
Consider consultation with local paediatric team when
- Systemically unwell
- Suppurative complications are present
- Evidence of moderate/severe dehydration
- Significant pain poorly responsive to supportive management (including analgesia and steroids)
Consider consultation with paediatric/ENT outpatient follow-up when
- 7 episodes of sore throat/tonsillitis in 1 year
- 5 infections/year for 2 consecutive years
- 3 infections/year for 3 consecutive years
- Recommendations may differ, please refer to local referral guidelines
Consider transfer when
- Evidence of acute suppurative complications eg abscess formation
- Evidence of upper airway obstruction
- Significant comorbidities are present, eg immunosuppression (after discussion with relevant treating team)
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Pain relief is adequate
- Tolerating appropriate oral intake
Parent information
Kids Health Info: Tonsillitis
Australian Commission on safety and Quality in Health Care: Sore Throat: Should I take antibiotics?
What every parent should know about colds, coughs, earaches and sore throats
Last updated October 2024