See also
Management of tetanus prone wounds
Cellulitis and other bacterial skin infections
Key points
- Rabies is a vaccine-preventable disease
- Post-exposure prophylaxis treatment with thorough washing of wounds with soap, as well as the appropriate vaccine ± immunoglobulin regimen, prevents virus entry into the central nervous system
- In Australia, exposure is from bats and travellers who have returned from rabies endemic areas
Background
- Rabies virus primarily causes disease in wild or domestic mammals, eg monkeys and dogs. Australian Bat Lyssavirus (ABLV) is closely related to rabies and is found in bats (including flying foxes and microbats)
- These viruses are shed in the saliva of animals
- The clinical disease caused by rabies virus and the other lyssaviruses are indistinguishable and is termed “rabies”
- Rabies is not endemic in Australia. See
The global distribution of rabies for information on other regions
- Transmission from animals to humans can occur as a result of bites or scratches from animals, or from direct viral contact with a mucosal surface. Transmission between humans has not been proven
- Incubation period varies from 5 days to many years
- The virus infects the nervous system resulting in encephalitis and brain stem dysfunction causing death
- Advising families on prevention by avoiding contact with wildlife and undertaking vaccination prior to travelling to rabies endemic areas is extremely important
- Symptoms, investigations and management of suspected rabies cases are not discussed in this guideline
Assessment
History and examination
- History of exposure
- Nature of exposure: bite, scratch, mucous membrane exposure
- Location of bite: head and neck, highly innervated areas eg fingers
- Animal source of exposure (note: within Australia if a bat is the source, and it is possible without placing others at risk, keep the bat to be sent for ABLV testing)
- Country of exposure
- First aid administered
- Immunisation history of the child (pre-exposure rabies prophylaxis, tetanus)
- Information on any rabies treatment given overseas; date, volume, type, route
Management
Investigations
- No investigations are required for asymptomatic children
Treatment
- First aid: wash wound with soap or detergent then flush wound for 15 minutes. Apply an iodine-containing solution on top of the wound after flushing. Appropriate first aid substantially reduces the infection risk
- If the wound is open: clean ± debride, do not suture
Post-exposure prophylaxis from mammals overseas and bats in Australia
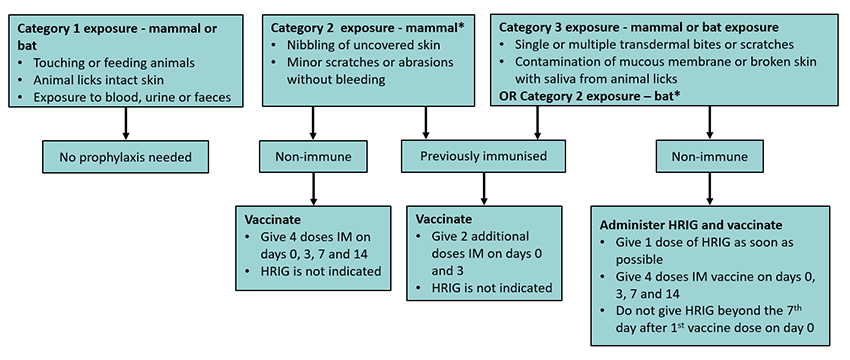
* Management of category 2 bat exposure is different to category 2 mammal exposure as superficial wounds from bats are a higher risk for infection
Note:
- If unsure whether treatment is required, discuss with local public health unit/health department or infectious diseases team
- The first dose of vaccine should be given as soon as possible after exposure
- Check child’s allergies: the vaccine Rabipur® contains egg protein
- Must be administered away from the site of HRIG eg contralateral deltoid or anterolateral thigh
- Rabies immunoglobulin (HRIG) dose 20 IU/kg
- Infiltration of HRIG is painful, ensure adequate analgesia +/- sedation
- Topical and local anaesthetic (LA) infiltration into the wound is contraindicated
- Infiltrate as much of the dose as possible in and around all wounds if feasible
- Give the remainder of the dose IM in a different limb from the rabies vaccine injection site
- Consult the
immunisation handbook and infectious diseases team for treatment and serological follow-up of immunocompromised children
- Post-exposure prophylaxis commenced overseas:
- If there is clear documentation of an appropriate vaccine course, complete treatment with the standard post-exposure prophylaxis regimen
- If there is unclear documentation or in other scenarios, consult the
immunisation handbook as to whether the schedule should be restarted at Day 0
Provision of treatment varies by state, check local information
Any confirmed cases of rabies or ABLV requires urgent notification to the Department of Health
Consider consultation with local paediatric team when
Consider consultation with local infectious diseases team or state department of health if unsure how to proceed
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services.
Consider discharge when
Plan is in place for completion of vaccination schedule and review of wounds
Parent information
Rabies and Australian Bat Lyssavirus infection
Rabies
Australian Bat Lyssavirus
Last updated December 2021