See also
Acute eye injury
Eye examination
Key points
- An open globe, or penetrating eye injury is a serious threat to vision
- In penetrating eye injury, avoid any pressure on the eyeball through examination or padding, as eye contents may be extruded
- Ensure prompt and adequate analgesia. Do not give any eye drops
- If identified or suspected, stop examination, place an eye shield over the eye, keep nil by mouth and urgently refer to ophthalmology. Urgent imaging may also be required
Background
- An open globe injury is defined as a full thickness injury to the cornea or sclera resulting in either globe rupture or laceration
- Globe rupture is more common in blunt injury, and laceration as a result of trauma from a sharp object or high velocity projectile
- Most injuries occur at home away from parental supervision
- Open globe injuries are associated with poor visual outcomes
- Open globe injuries may accompany multiple trauma or serious head injury
Assessment
History
- Full history of event including timing and witnesses
- Mechanism of injury eg blunt force/sharp object/projectile
- Composition of any possible intraocular foreign body eg soil/dirt/metal
- Pain
- Decrease in vision
- Associated injuries (may accompany multiple trauma or serious head injury)
Examination
- Examination may only need to be cursory but should include an attempt at determining visual acuity and assess for a Relative Afferent Pupillary Defect
-
Primary survey
- Avoid pressure on the globe if perforation is suspected and examine with the utmost care
- In young children examination facilitated by procedural sedation or general anaesthesia should be performed by an ophthalmologist whenever the mechanism of injury is highly suggestive of an open globe
- See Eye Examination
Signs suggestive of globe perforation
- Missile protruding from the eye: do not remove it or touch it
- Severe loss of vision
- Loss of red reflex
- Relative Afferent Pupillary Defect
- Squashed or distorted appearance to globe
- Swollen, haemorrhagic eyelids
- Chemosis (bulging of the conjunctiva)
- 360 degree subconjunctival haemorrhage
- Distorted, irregular or peaked pupil
- Ocular contents extruding from globe (iris and retina are pigmented, vitreous is a clear jelly)
- Increased or decreased anterior chamber depth
|
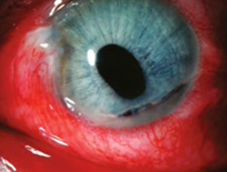
Penetrating eye injury with 360 degree
subconjunctival haemorrhage, irregular
shaped iris, hyphaema and extrusion of ocular contents |

Penetrating eye injury with prolapse of iris
|
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240.
Available here
Management
Suspected penetrating eye injury
- Do not force eyelids open - pressure on the lids may cause extrusion of ocular contents
- Do not attempt to remove a protruding foreign body from the globe
- Urgently notify ophthalmology for all suspected penetrating eye injuries
- Place an eye shield
- Fast the child from the time they are seen
- Do not give any eye drops
- Use appropriate analgesia. Consider NSAIDs. Consider concurrent antiemetic (eg ondansetron) as vomiting increases intraocular pressure and may cause expulsion of ocular contents
- Place the child on bed rest with head of bed elevated to 30 degrees if haemodynamic condition allows
- Check tetanus status
- Give antibiotics:
- If prophylaxis without signs of infection: oral ciprofloxacin 20mg/kg (maximum 750mg) BD
- If endophthalmitis is suspected or signs of infection: give IV ceftazidime 50mg/kg (maximum 2g) 8 hourly and vancomycin 15mg/kg (maximum 750mg) 6 hourly
After discussion with ophthalmology, image the orbit (X-ray or CT) in cases where an intraocular foreign body is suspected
Consider consultation with local paediatric team when
A child with suspected child abuse
Consider transfer when
A child with penetrating/open globe injury and management beyond the capability of local services
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- Penetrating or open globe injury has been treated or excluded AND
- The child is symptom free, or clear follow up plan in place with criteria for early review identified
Last updated October 2022