See also
Anaemia
Iron deficiency
Blood product prescription
The Australian Red Cross Blood Service anaemia and haemostasis overview
Key Points
- Patient Blood Management (PBM) aims to improve clinical outcomes by avoiding unnecessary exposure to blood components
- Assess all children undergoing surgery for risk of requiring RBC transfusions intra- or post-operatively
Background
- Anaemia and iron deficiency may be seen prior to paediatric surgery and are risk factors for adverse clinical outcomes and red blood cell (RBC) transfusion
- Identify and treat pre-operative anaemia prior to elective surgery associated with significant blood loss, with the aim of reducing a child’s risk of needing RBC transfusion
Three pillars of PBM applied to the surgical setting
Pre-operative
- Optimise a child’s red cell volume and red cell mass
- Identify and treat iron deficiency with or without anaemia prior to surgery
- Review medications and consider ceasing prior to surgery
Intra-operative
- Minimise intra-operative blood loss
- Surgical/anaesthetic techniques; use of antifibrinolytics and cell salvage where appropriate
- Maintenance of normothermia
- Minimise unnecessary blood tests
- Avoid unnecessary transfusions
Post-operative
- Minimise post-operative blood loss
- Minimise unnecessary blood tests
- Optimise a child’s tolerance of anaemia
- Optimise oxygen delivery to tissues
- Avoid unnecessary transfusions
Assessment
Any child undergoing elective surgery and at risk of requiring a RBC transfusion intra- or post- operatively should be assessed with regard to PBM. Assess pre-operatively for anaemia and iron deficiency
Red flags: See
Anaemia and
Iron deficiency
Considerations:
- Nature and length of surgical procedure
- Concurrent anti-platelet or anticoagulant medications
- Bleeding risk of surgery
- Previous operative history
- Previous RBC transfusion audit data
Management
Pre-operative
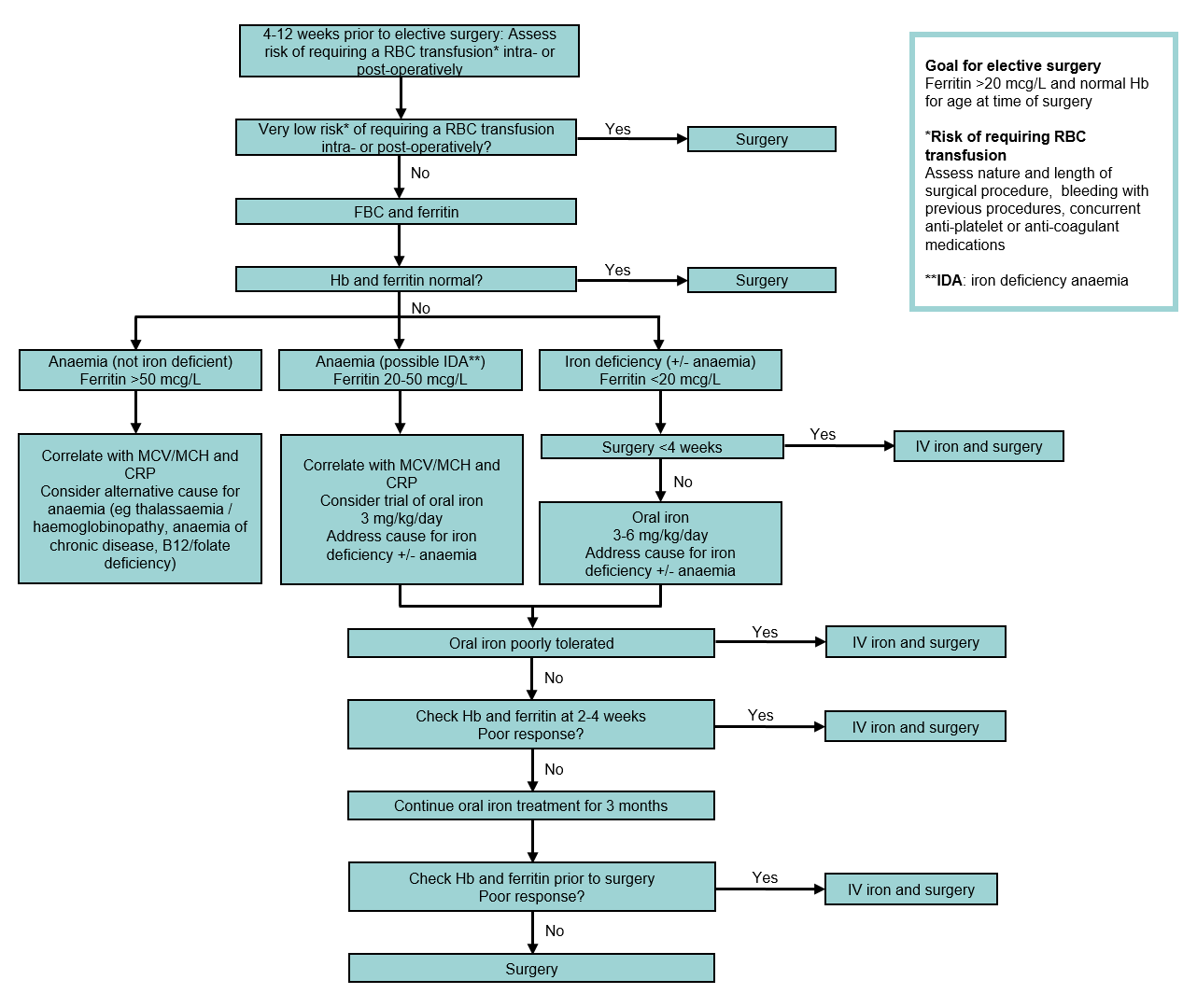
Pre-operative anaemia and iron deficiency assessment and optimisation
Intra-operative principles
- Maintenance of normothermia (temperature >36°C)
- Meticulous surgical and perioperative haemostasis to minimise blood loss
- Intravenous antifibrinolytics (eg tranexamic acid or aprotinin)
- Cell salvage
- Acid base balance status (pH >7.2 and ionised calcium >1.1 mmol/L)
- Optimise tissue oxygenation and perfusion, as well as cardiac output
- Minimise frequency and volume of blood sampling
- Point of care testing including viscoelastography
- ‘Restrictive’ transfusion triggers
- Single unit RBC transfusion in stable, non-bleeding children with reassessment of Hb between units
Post-operative principles
- Maintenance of normothermia (temperature >36°C)
- Optimise tissue oxygenation and perfusion, as well as cardiac output
- Acid base balance status (pH >7.2 and ionised Ca2+ >1.1 mmol/L)
- Tranexamic acid
- Single unit RBC transfusion with reassessment of Hb between RBC units
- Minimise frequency and volume of blood sampling
- Early removal of sampling lines when child is stable and frequent sampling no-longer required
- Clinical pathways for surgical specialities that inform clinicians of routine post-operative blood tests
- Consider iron supplementation in children who are anaemic after surgery (see
Iron deficiency)
Post-operative RBC transfusion triggers
Hb <70 g/L |
RBC transfusion is often indicated, however lower thresholds may be acceptable in children without symptoms and where specific therapy (eg iron) is available |
|
Hb <70-90 g/L |
RBC transfusion may be indicated, depending on the presence of bleeding and clinical signs or symptoms of anaemia |
|
Hb >90 g/L |
RBC transfusion is often unnecessary and may be inappropriate |
|
Note: higher thresholds may be indicated for specific situations, eg pre-term neonates, children with cyanotic congenital heart disease and extracorporeal life support (ECLS) |
Blood conservation strategies
- Reducing laboratory ordering, rationalising and consolidating laboratory blood testing
- Use of neonatal collection tubes
- Strict adherence with minimum volume analyte volumes for pathology tests
- Early removal of sampling lines
- Returning of discard volumes
- Point of care testing devices
- Extended expiry blood group and antibody screen in neonates
<4 months and surgical patients
Consider consultation with local paediatric team when
Iron deficiency and/or anaemia are identified
Consider transfer when
Children requiring care beyond the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Parent information
Blood product transfusion
Additional resources
Blood safe eLearning Australia
RCH Blood transfusion
RCH Blood Transfusion additional links
Updated November 2023