See also
Hypertension in children and adolescents
Key points
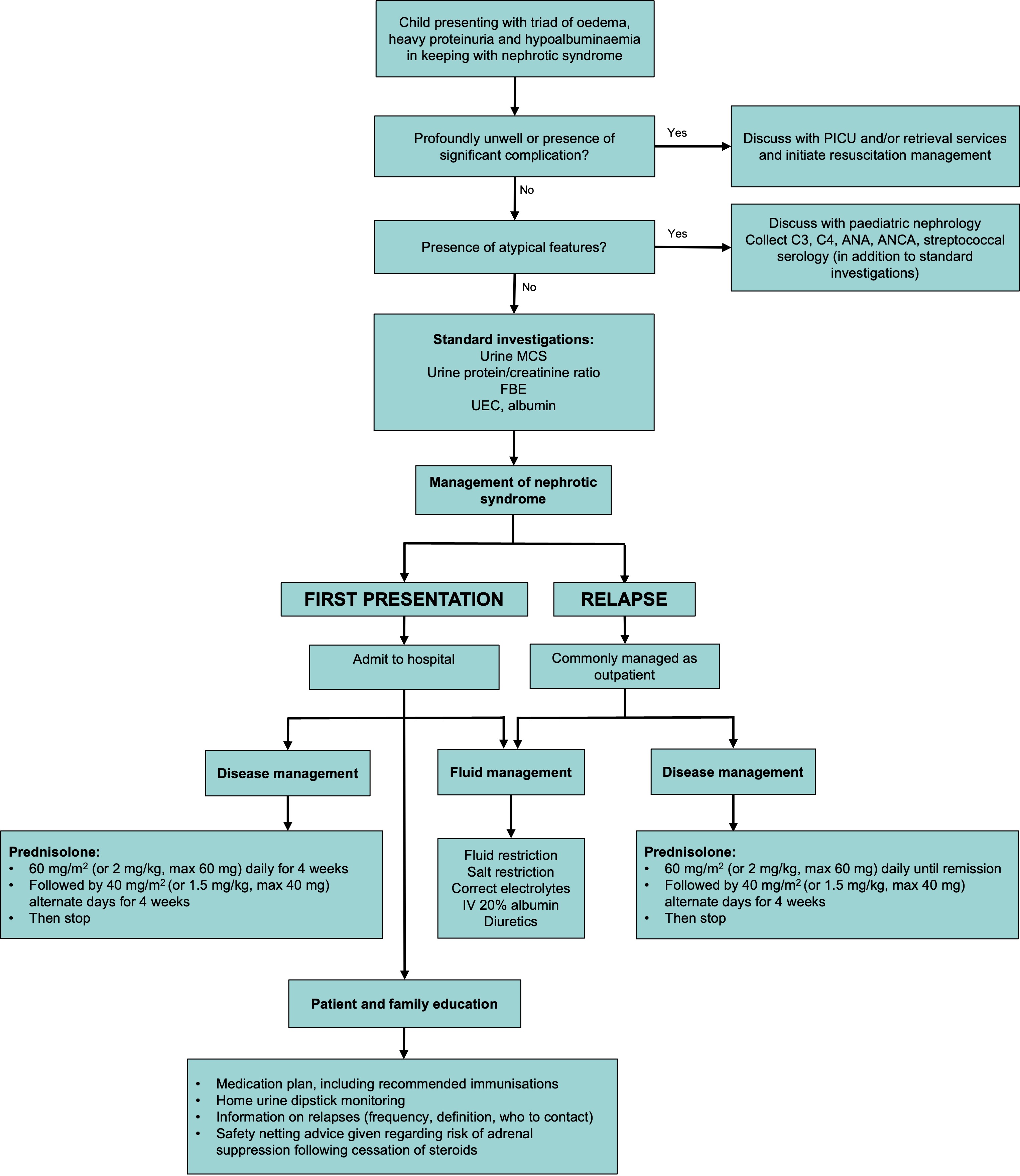
- Nephrotic syndrome (NS) is a clinical disorder characterised by the triad of proteinuria, hypoalbuminaemia and oedema
- Principles of treatment are:
- Treatment of underlying disease with steroids
- Early recognition and management of complications
- Management of oedema/fluid overload
- Discharge education is crucial following a first presentation due to the high risk of relapse
Background
- 90% of NS is idiopathic and the most common histological diagnosis in children is minimal change disease
- Most children with NS respond to prednisolone treatment, have a good prognosis and do not require renal biopsy
- It is important to identify children with atypical features, who should be discussed with Nephrology at presentation or early in the course of the disease
- Approximately 85% of children with steroid sensitive NS have at least one relapse and 50% have frequent relapses
Assessment
NS is diagnosed based on the triad of:
- Heavy proteinuria (dipstick >3+ or spot protein/creatinine ratio >200 mg/mmol)
- Hypoalbuminaemia (serum albumin <25 g/L)
- Oedema
Remission: resolution of proteinuria, defined by 3 consecutive days of negative or trace urine protein
Relapse: >3+ proteinuria for 3 consecutive days - often triggered by mild illnesses, but can occur spontaneously
History
- Oedema (can be dependent and/or non-dependent)
- Recent or intercurrent infections
- Presence of any significant complications (see below)
- Presence of any atypical features (see below)
- Immunisation history
- Family history of renal disease
Examination
- Growth parameters and comparison to pre-illness weight (may be an isolated sign of fluid overload in absence of oedema)
- Fluid and oedema assessment (degree of fluid overload and estimation of intravascular volume depletion)
- Blood pressure (use age and gender reference ranges); confirm with manual measurement (see Hypertension)
- Presence of extra-renal features (eg rash, joint involvement)
Significant complications
| Intravascular volume depletion |
Dizziness, abdominal cramps, poor perfusion, tachycardia, reduced urine output, transient hypertension, hypotension, shock |
| Severe oedema |
Discomfort, pulmonary oedema, pleural and pericardial effusions, ascites, scrotal/labial oedema, skin breakdown and generalised discomfort |
| Infection/sepsis |
Encapsulated bacterial infection due to loss of complement |
| Spontaneous bacterial peritonitis |
Abdominal pain with rebound tenderness, fevers, nausea/vomiting (signs can be masked by steroids) |
| Thrombosis |
Can be venous or arterial and located in any site eg central venous thrombosis, renal vein thrombosis, pulmonary embolism |
| Severe hypertension |
Headache, vomiting, blurred vision, change in mental state, seizures, chest pain, palpitations, shortness of breath, cardiac failure |
Atypical features
- Age <1 or >12 years
- Features of nephritic syndrome (renal impairment, macroscopic haematuria and hypertension)
- Persistent hypertension (can have mild elevation in first 1-2 days)
- Persistent renal impairment (can be related to intravascular hypovolaemia initially)
- Significant complications at first presentation
- Features (eg rash, arthritis, fevers) that may suggest a systemic disease eg SLE, HSP, sickle cell, HIV, hepatitis
- Dysmorphic features that may suggest a syndromic cause
Management
Investigations
Standard investigations:
- Urine dipstick
- Urine MCS
- Spot urine protein/creatinine ratio
- UEC, LFTs, albumin
- FBE
If raised creatinine, atypical history, or concern for systemic disease, consider further testing discussion with paediatric nephrology team:
- Complement C3, C4
- ANA, ANCA
- Anti-streptococcal antibodies: ASOT +/- anti-DNAse B (depending on laboratory availability)
Consider:
- Chest X-ray (if any concerns for pleural effusion or significant pulmonary oedema)
- Renal tract ultrasound (including doppler) in cases of unclear diagnosis, significant flank or abdominal pain, atypical history or poor response to diuretics eg congenital malformations, renal vein thrombus
- Blood culture (if febrile, or systemically unwell)
Treatment
- Admit all children to hospital on their first presentation
- Early identification and management of any complications is critical
- Main components of treatment are:
- Fluid and oedema management
- Disease management (corticosteroids). Note that the dose and length of corticosteroid treatment differs depending on whether it is the first presentation or a relapse
- Patient and family education. Due to the likelihood of relapse, and the need for home dipstick monitoring, it is important to start education early during the admission
- Children can have significant electrolyte derangements that require active management. Mild hyponatraemia will often correct with fluid restriction alone
- Elevated creatinine can be present initially, but should usually improve in the first few days
Fluid and oedema management
| Strict fluid balance |
Measure urine output and calculate in mL/kg/hr
Daily weights taken at the same time on same scales |
| Sodium restriction |
Limit to 2-3 mmol/kg (approx 40 mg/kg or 2 g/day)
Generally, low or no-added salt diet is sufficient to achieve this |
| Fluid restriction |
Particularly useful when hyponatraemic (Na <130 mmol/L)
Restrict to 50-70% of usual maintenance fluid in total across 24 hrs
Do not count albumin administration in this fluid allowance |
Intermittent concentrated albumin infusions
(+/- diuretics) |
5 mL/kg of 20% albumin (equivalent to 1 g/kg) administered over 4 hours
- Indicated when there is intravascular volume depletion and/or severe or symptomatic oedema
Monitor closely for hypertension and pulmonary oedema (infusions should occur during the day with adequate staffing)
Consider IV furosemide (0.5-1mg/kg max 40mg) at middle and/or end of infusions
- Diuretics should be used cautiously (usually only in combination with albumin infusions) as may precipitate intravascular volume depletion, acute kidney injury and increase risk of thrombosis
|
Disease management
- Prednisolone - dose should be rounded up to the easiest administrable dose; tablets are more cost effective and accessible (can be crushed)
- If unable to tolerate oral intake, give equivalent dose of IV methylprednisolone (80% of oral prednisolone dose)
- For first presentations, the initial dose of prednisolone continues for 4 weeks, regardless of how quickly remission is achieved
- For relapses, the initial dose of prednisolone is only continued until remission achieved
- Two consecutive relapses (on decreasing prednisolone dose), or relapse within 15 days of stopping prednisolone is deemed steroid dependent NS
| First presentation |
Relapse presentation |
Prednisolone 60 mg/m2
or 2 mg/kg (max 60 mg)
oral daily for 4 weeks |
Prednisolone 60 mg/m2
or 2 mg/kg (max 60 mg) oral
daily until remission achieved |
Followed by |
Prednisolone 40 mg/m2 or 1.5 mg/kg (max 40 mg) oral alternate days for 4 weeks If relapse occurs during this period, increase prednisolone dose to 60 mg/m2 or 2 mg/kg (max 60 mg) oral daily until remission achieved again, then repeat the step down to 40 mg/m2 or 1.5 mg/kg (max 40 mg) oral alternate days for 4 weeks
|
Then stop |
Prophylactic and additional treatments
| Antibiotics |
Not indicated unless there is a risk of pneumococcal infection (eg gross oedema, unimmunised) |
Acid suppressing treatment eg proton pump inhibitors |
Not indicated unless there are upper gastrointestinal symptoms while on steroid therapy |
| Immunisations |
- Additional meningococcal and pneumococcal vaccines
- Yearly influenza vaccine
- Live vaccines need to be delayed until 1 month off steroid treatment
- Consider varicella immunoglobulin for children unimmunised against varicella, who are in relapse or on steroids, and have had an exposure to chickenpox
see Australian Immunisation Handbook
|
| VTE prophylaxis |
Mechanical prophylaxis (above-knee TED stockings) is usually all that is required for children >12 years who are mobile and do not have any other risk factors for VTE |
| Stress-dose steroids |
- Following cessation of steroids, there is a risk of adrenal suppression
- Adrenal stimulation testing should be considered in those children at risk of adrenal insufficiency (eg cushingoid appearance or frequent relapses)
- Consider discussion with endocrinology if relapses are frequent and there is concern for adrenal suppression
See Adrenal crisis and acute adrenal insufficiency
|
| Vitamin D, thyroid hormone, lipid lowering medication |
- Abnormalities transient and related to proteinuria
- Supplementation is not usually required if remission is achieved and maintained
|
Consider consultation with local paediatric team when
Any child with nephrotic syndrome
Consider consultation with local paediatric nephrology team when
- Atypical nephrotic syndrome features present
- Any significant complications present
- No resolution of proteinuria after 4 weeks of prednisolone
- Oedema refractory to management strategies
- Development of more complex disease phenotypes or steroid toxicity
- In some centres, all first presentations of confirmed/suspected NS
Consider transfer when
Complications of nephrotic syndrome are present that are unable to be managed locally
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Oedema can be managed without regular IV albumin infusions and weight is not increasing
- Appropriate steroid treatment has been commenced
- Discharge education has been provided and follow up arranged
Note: Liquid prednisolone only comes in 30 mL bottles. Consider using prednisolone tablets and rounding to easily administered dose (usually only 25 mg and 5 mg tablets are required). If liquid is preferred, provide the child with an authority prescription
Discharge education
- Family should be counselled on the high recurrence rate of NS (approximately 85% will have at least one relapse), what constitutes a relapse and who to contact
- Home urine dipstick testing should continue daily until proteinuria resolves (3 consecutive days of negative or trace urine protein). This is best collected first thing in the morning
- After resolution of proteinuria, recommend dipstick testing at least twice weekly in the first year (individualised thereafter)
- Revert to daily testing if ≥1+ protein, intercurrent infections, oedema, suspected relapse
- Following cessation of steroids there is a risk of adrenal suppression, and this should be explained to families and written information given about the potential need for steroids in the case of acute illness or trauma
- Plan made for additional immunisations, to be administered as an inpatient, in an immunisation clinic, or by general practitioner
Parent information
Nephrotic syndrome | infoKID
Nephrotic syndrome information and record book | RCH
Proteinuria record
Last updated July 2025