This guideline applies to all patients requiring
intubation in ED, and all patients with respiratory failure in paediatric and
neonatal ICU requiring airway management. It must be read in conjunction with
the Emergency airway management CPG
See also
Resuscitation
Emergency airway management (non COVID-19)
Intubation checklist
Key points
- Airway management in patients with COVID causes aerosolisation of virus
- Use airborne precautions and the highest level of isolation available
- The most experienced airway team available should manage the airway
Background
Airway management in patients with COVID-19 is associated with aerosol generation that carries the risk of virus transmission to healthcare workers, and in turn other patients.
|
Aerosol Generating Procedures (AGPs)
|
|
Face mask ventilation
|
Oropharyngeal suctioning |
Ventilation via a supraglottic airway (SGA)
eg laryngeal mask airway (LMA) |
CPR on patient prior to intubation |
Intubation including insertion of an SGA |
Extubation including removal of an SGA |
Open suctioning of endotracheal tube (ETT) (in-line suction is preferred) |
Non-invasive ventilation / high flow nasal
cannula therapy (HFNC) / nebuliser therapy |
Continuous nitrous oxide sedation |
Bronchoscopy |
Management
Prepare environment
- Management must occur in the highest level of isolation available: negative pressure room if available and appropriate
- Personnel should be kept to a minimum and physical distancing should be maintained if possible; restrict personnel to those with most expertise
- Ensure that the child’s accompanying support person is wearing appropriate PPE
- Minimise equipment in the room during the AGP by only selecting equipment necessary for airway plans. Induction agent, muscle relaxant and other necessary medications should be drawn up and kept in room
- Place Heat and Moisture Exchanger (HME) filters in the circuit on the ventilator side of any potential site for circuit disconnection including ventilator side of the face mask
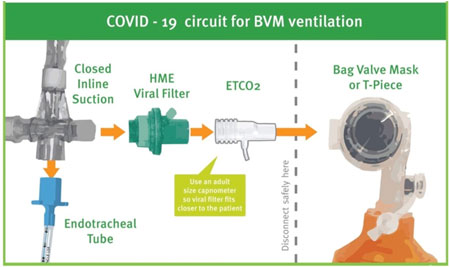
Image used with permission from Children's Health Queensland Hospital and Health Service
- Have a staff member outside the room to pass equipment that was not initially inside, and prevent unnecessary staff from entering the environment (consider using communication devices)
- Limit unnecessary thoroughfare into the procedure room. Minimise repeated entry and exit of staff
- Have appropriate waste bins available, including a clear plastic bag or bin liner to place soiled reusable equipment temporarily until cleaned
- Sedative premedication and topical anaesthetic cream are only applicable in the conscious child (but do not delay for emergency airway management)
Airborne PPE must be used when treating high risk patients during AGPs
- N95 mask
- Eye protection (face shield if available)
- Gown
- Gloves (preferably 2 pairs)
- Ensure sufficient PPE is stored outside the room for staff who may need to enter to assist emergently
Airway Management
- Most experienced clinician airway team available should manage airway
- Minimise interval between removal of patient’s PPE and application of facemask
- Ensure facemask is the appropriate size, use two person techniques when possible

Image used with permission from Children's Health Queensland Hospital and Health Service
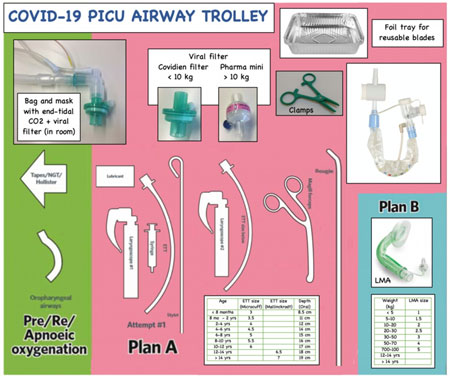
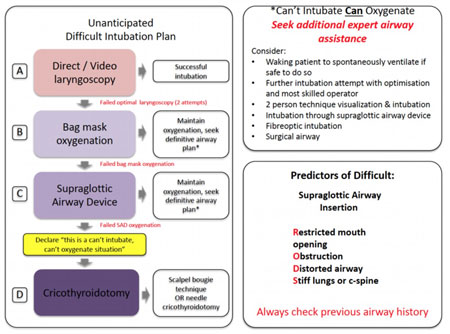
- An emergency intubation checklist and other cognitive aids should be used during emergency airway management. Please see examples below of a COVID-19 Airway Trolley Template and Emergency Intubation Plan
- Minimise aerosolisation of virus by:
- Avoid HFNC - use acceptable oxygen flow (eg 2L / min)
- Consider using video assisted laryngoscopy if available to increase the likelihood of first pass success, and to maintain distance from the oropharynx
- NB C-MACTM preferred over using the GlideScopeTM (latter only if difficult laryngoscopy is anticipated)
- Intubate with a cuffed ETT. Inflate cuff as per unit guideline prior to commencement of IPPV
Example COVID-19 Airway Trolley Template
Example Emergency Intubation Plan
Post intubation
- Avoid contamination from the laryngoscope blade. Place blade and handle (and C-MACTM lead) into an open plastic bag or bin liner
- Clamp ETT during circuit disconnections for transfer, unless apnoeic, or leave filter attached to ETT
Extubation
- Ideally done in PICU, NICU or operating theatre rather than ED
- Minimise staff in the room
- After airway patency and spontaneous ventilation confirmed, place a Hudson mask or nasal prongs with a surgical mask on top
- Consider emergence delirium prophylaxis to minimise crying / screaming
- Consider additional anti-emesis to avoid vomiting
- If upper airway obstruction is anticipated, early insertion of SGA (LMA or oropharyngeal airway) should be considered
After airway management
- Immediately dispose of single use equipment in an appropriate clinical waste bin
- Reusable equipment must be thoroughly cleaned
- Dispose of ventilating circuits if saturated with condensation or visibly soiled
Difficult laryngoscopy in COVID-19 patients
Unanticipated difficult laryngoscopy is rare in infants and children. If an experienced clinician has been unable to successfully intubate a child on the first attempt, the situation should be considered a difficult laryngoscopy. To ensure safety of the child and staff, do not perform repeated attempts at direct laryngoscopy. Consider bag mask oxygenation or insert LMA and call for help. Pay attention to not contaminating the environment further. The next attempt should be the best attempt and involve an advanced intubation technique using video laryngoscopy or flexible intubating bronchoscopy
For anticipated difficult laryngoscopy, advanced intubation equipment should be in the room or consider moving to operating theatre
In-line suction sizing
If ongoing suctioning required, use closed in-line suctioning systems (come in different types depending on the size). Choose the size of suction catheter based on the size of the ETT
See the video here for more information
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services.
Additional resources
NSW airway management resources
Queensland airway management checklist
Last updated January 2022