See also
Fractures
Bone and joint infections
Acutely swollen joint
Child abuse
Key points
- Most children presenting with a limp do not require investigations
- Observing the child's gait may help localise the problem and narrow the differential diagnosis
- Acute inability to walk or weight-bear is a red flag
- Septic arthritis is an orthopaedic emergency and should be considered in all limping children with severe localised joint pain and fever
Background
- Transient synovitis, acute myositis and minor trauma are common causes of limp in children, but serious pathology should be excluded
- Pain causing limp can be referred. Therefore, a thorough assessment of joints above and below (including the spine and other relevant body systems) is essential to accurately localise the source
Assessment
Red flag features in red
History
• Duration of symptoms >7 days
• History of trauma, falls or injury
• Pattern and severity of pain and limp: severe localised joint pain should raise suspicion for septic arthritis
• Change to urinary or bowel habit
• Functional limitations: complete inability to walk or weight-bear may indicate significant pathology
• Nocturnal pain and symptoms
• Systemic symptoms: fever, night sweats, chills, rigors, rash
• Constitutional symptoms eg unplanned weight loss, lethargy/easy fatigue, anorexia (consider malignancy/haematological cause)
• Recent viral infection (acute myositis, transient synovitis)
Examination
- Generalised wasting, pallor, interaction with carer
- Fever
- Assess gait if possible – walking +/- running
- Joint examination using "Look, Feel, and Move" including joints above and below area of pain
- Identify location if possible — bone vs joint vs soft tissue
- Look: resting limb position, leg length disparity, swelling, deformities, skin changes e.g. rash, wound, bruising, erythema, pallor
- Feel: heat, cold, tenderness (including calf), crepitus, fluctuance
- Move:
- active: facilitate by placing toy or parent out of reach
- passive: assess for limitations and asymmetry in all planes of motion
- compare both sides, as well as active and passive range of movement. A marked reduction in range of motion is suggestive of more serious pathology such as septic arthritis
- tone, power, and reflexes
- Neurovascular assessment of affected limb
- Abdomen, scrotum, back/spine
- Petechiae/purpura/ecchymosis (consider HSP, malignancy/haematological cause)
Common differential diagnoses:
|
Toddler (0-4 years) |
Child (5-10 years) |
Adolescent (>10 years) |
|
|
- Transient hip synovitis
- Acute myositis
- Developmental dysplasia of hip
- Perthes disease
|
- Stress fractures & sprains
- Traction apophysitis (Osgood Schlatter – tibial tuberosity, Severs – calcaneus)
- SUFE
|
|
All ages:
- Infections:
osteomyelitis/septic arthritis, bursitis, discitis, epidural collection
- Trauma (see
Fractures)
-
Non accidental or inflicted injury
- Malignancy: haematological, bone, soft tissue
- Rheumatological/immunological disorders: reactive arthritis, autoimmune arthritis, Henoch Schonlein Purpura, vasculitis, serum sickness, post infectious arthritis, Guillain-Barre syndrome
- Intra-abdominal pathology or genitourinary conditions eg appendicitis, ovarian or testicular torsion
- Haematological: vaso-occlusive crisis (sickle cell), haemophilia
- Functional limp
|
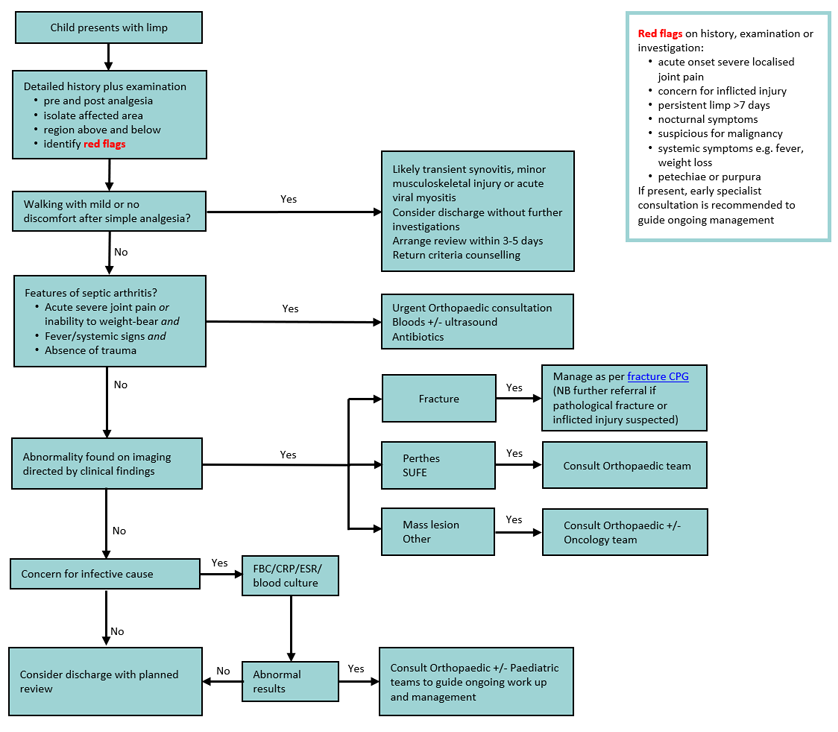
Management
Investigations
- No investigations are indicated if all of the following apply:
- no red flags in the history and physical examination
- ambulating with mild or no discomfort with simple analgesia
- a clear working diagnosis and/or a plan for review within 7 days of onset of limp
- Imaging
- X-ray (area of suspicion)
- pelvis AP or frog leg view is useful for identifying SUFE, DDH (>6 mo), Perthes disease and common pelvic avulsions
- normal x-ray does not exclude septic arthritis or early osteomyelitis
- Ultrasound (hip)
- assess for presence of drainable effusion when septic arthritis is suspected
- presence of an effusion often does not differentiate between septic arthritis and transient hip synovitis
- Other eg bone scan or localised MRI if still limping at 7 days, consult local paediatric, orthopaedic or radiology services
- Laboratory
- Raised inflammatory markers (platelets, WCC, CRP +/- ESR) may suggest infective or inflammatory picture. These may be normal in contained or chronic infections
- Blood cultures (pre-antibiotics if possible) if osteomyelitis, septic arthritis or septic bursitis are suspected
- FBE and film if any concern for haematological malignancy
Treatment
- Definitive management is determined by the working diagnosis
- Simple analgesia - paracetamol +/- NSAID. Escalation of analgesia may be required but should prompt reassessment for
red flags
- Child-directed limitation of activity
- Splint suspected
fractures and manage accordingly
- Septic arthritis is an orthopaedic emergency - consult local orthopaedic specialist ASAP
- For infective causes, refer to the appropriate sub-specialist team and consult
local antibiotic guidelines. If the child is stable and access to surgery will not be delayed, obtaining a surgical sample prior to antibiotic treatment is preferable. If the child is unwell do not delay treatment
Consider consultation with local paediatric team when
- There is possible
non-accidental injury
- There are clinical or laboratory features of malignancy
- Systemically unwell
- Symptoms last more than 7 days, or child unable to weight-bear or permit movement after analgesia
- Suspecting septic arthritis - consult with orthopaedic team
Consider transfer when
Child requires care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- The cause of the limp has been identified and adequately managed
OR
- Child is ambulating comfortably with or without analgesia AND
- High risk diagnoses have been considered AND
- Adequate follow up plan in place
Parent information
Additional notes
Kocher Criteria
In a child with hip pain, presence of the following 4 criteria increases the likelihood of septic arthritis:
- fever >38.5°C
- non weight-bearing
- leucocytosis >12.0 x 109/L
- ESR >40 mm/h (or CRP >20 mg/L)
| No of predictors |
Probability of septic arthritis |
| 0 |
Very low |
| 1 |
Low |
| 2 |
Moderate (refer) |
| 3 |
Very high (refer) |
| 4 |
Very high (refer) |
Last updated July 2020