See also
Iron deficiency
Patient Blood Management and surgery
Blood product prescription
The Australian Red Cross Blood Service anaemia and haemostasis overview
Key Points
- Iron deficiency is the most common cause of anaemia in children
- Consider admission and discussion with local paediatrician or haematologist for children with red flag features
Background
Anaemia is defined as haemoglobin (Hb) less than the lower limit of the reference range for age
| Age |
Lower limit of normal range Hb (g/L) |
2 months |
90 |
2-6 months |
95 |
6-24 months |
105 |
2-11 years |
115 |
>12 years |
Female: 120, male: 130 |
Assessment
History
- Lethargy
- Poor concentration
- Weakness
- Shortness of breath
- Ethnic background (can be helpful in guiding investigation for haemoglobinopathies and G6PD deficiency)
- Medication history: past and current, particularly those that may cause haemolysis in children with G6PD deficiency
- Dietary history: iron intake (with particular attention to iron-rich foods, breast feeding and cow milk intake), vitamin B12 intake, recent fava/broad bean ingestion (may precipitate haemolysis in children with G6PD deficiency)
- Family history: anaemia, jaundice, gallstones or splenomegaly
Examination
- Poor growth
- Listlessness or fatigue
- Pallor
- Pale conjunctivae
- Tachycardia
- Cardiac murmur
- Signs of cardiac failure
- Shortness of breath
- Weakness
- Signs of haemolysis (jaundice, scleral icterus, splenomegaly and dark urine)
Management
Investigations
- FBC and film
- Reticulocyte count
- Ferritin
- Iron studies or serum iron should not be requested to diagnose iron deficiency. Serum iron reflects recent iron intake and does not provide a measure of the iron stores
- For “Other features on the blood film appearance that prompt further investigation”, see Additional Notes below
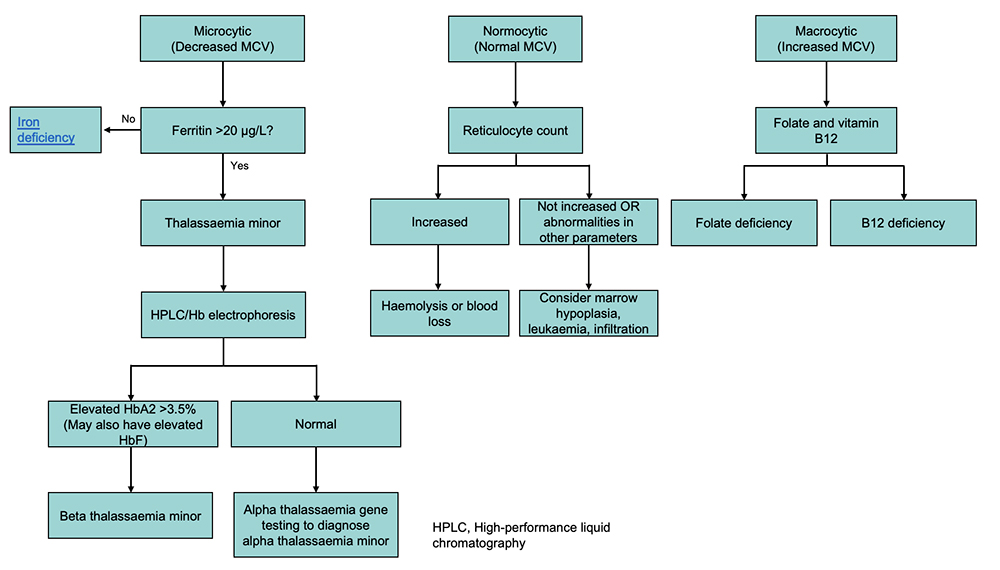
MCV classification of anaemia
The initial classification is based on the mean corpuscular volume (MCV)
Red flags (consider admission)
- Hb <60g/L (including iron deficiency)
- Tachycardia, cardiac murmur or signs of cardiac failure
- Features of haemolysis eg dark urine, jaundice, scleral icterus
- Associated reticulocytopenia
- Presence of nucleated red blood cells on blood film
- Associated thrombocytopenia or neutropenia, may indicate malignancy or an infiltrative disorder
- Severe vitamin B12 or folate deficiency
- Need for red cell transfusion (where possible defer transfusion until a definitive diagnosis is made)
Microcytic Hypochromic Anaemia
Iron deficiency
Beta Thalassaemia minor/trait
- Carrier of beta thalassaemia
- Frequently seen in South East Asian, Mediterranean, Arabic families
- There may be a positive family history
- Usually asymptomatic
- Microcytic hypochromic red cells with normal or borderline low Hb
- Diagnosed on high-performance liquid chromatography (HPLC) or Hb electrophoresis (HbA2 >3.5%, often elevated Hb F)
- HbA2 may not be elevated in the presence of concomitant iron deficiency, therefore give iron treatment (if ferritin low) before ordering test
- Red cell distribution width (RDW) is often normal
- Pre-pregnancy carrier testing of partner is important, ensure parents have been tested if likely to have more children
Alpha Thalassaemia minor/trait
- Carrier of alpha thalassaemia
- Commonly seen in South East Asian, African, Mediterranean, Arabic families
- Microcytic hypochromic red cells with normal or borderline low Hb
- Cannot be diagnosed on HPLC or Hb electrophoresis. DNA testing required for formal diagnosis (not a first-line investigation, exclude other causes first)
- Pre-pregnancy carrier testing of partner is important
Rare causes of microcytic anaemia
- Chronic inflammation
- Lead poisoning (high blood lead level)
- Sideroblastic anaemia
Normocytic normochromic anaemia
Haemolytic anaemia
- Acute haemolysis in childhood can be a life-threatening illness and all cases should be discussed with a haematologist
- Admit children with haemolytic anaemia for observation. Frequent heart rate monitoring is required to identify tachycardia which may indicate a further drop in Hb
- Repeat FBC within 6-12 hours to detect ongoing haemolysis
- Monitor reticulocyte count and bilirubin
- Additional investigations will be guided by blood film findings eg Coombs test (direct antiglobulin test), blood group and antibody screening (BGAB), G6PD assay and Eosin-5 maleimide red cell staining (diagnosis of hereditary spherocytosis)
Sickle cell anaemia
See Sickle cell disease
Hypoplastic/aplastic anaemia
- Causes
- Acute leukaemia, aplastic anaemia, infiltrative disorders
- Drugs (eg cytotoxics, chloramphenicol, sulfonamides)
- Viral infection
- Severe nutritional deficiencies (vitamin B12 or folate deficiency), however usually children present with macrocytic red cells
- Reticulocyte count is usually low
- Differential diagnosis based on FBC results
- Consider bone marrow infiltration if neutrophils and/or platelets also decreased
- If isolated anaemia with low reticulocyte count with normal platelet and neutrophil counts, consider transient erythroblastopenia of childhood (TEC) or congenital forms (eg Diamond-Blackfan anaemia)
- Bone marrow aspirate is usually required for diagnosis
Chronic disease
- Normochromic normocytic anaemia can be seen with chronic inflammation and chronic disease such as renal disease
- Reticulocyte count may be low
- Platelet count may be elevated
- Further investigation (eg UEC, LFT and ESR) may be indicated depending on clinical features
Blood loss
- Normochromic normocytic anaemia can be seen with acute blood loss
- Reticulocyte count may be normal or elevated
- Correlate with any bleeding symptoms
Macrocytic anaemia
Vitamin B12 and folate deficiency
- Can be associated with failure to thrive or neurodevelopmental problems (regression, seizures, irritability, poor feeding)
- Vitamin B12 deficiency may be seen in exclusively breast-fed infants of mothers with vitamin B12 deficiency, children with a vegan or vegetarian diet, pernicious anaemia and metabolic disorders
- Characteristic blood film findings include teardrop red cells and hypersegmented neutrophils and often neutropenia or thrombocytopenia
- Requires urgent investigation with red cell folate and active vitamin B12
- If low active vitamin B12 suggest serum homocysteine and urine methylmalonic acid
- Treatment must be commenced urgently, particularly if neurological symptoms or regression
Other causes of red cell macrocytosis with or without anaemia
- Myelodysplasia
- Medications eg anticonvulsants, immunosuppressants and zidovudine
- Liver disease
- Hypothyroidism
Consider consultation with local paediatric team when
Children have red flag features
Consider transfer when
Children require care beyond the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
Cause for anaemia is identified and follow up is arranged
Parent information
Iron intake (Royal Children’s Hospital Melbourne)
Iron for children (Queensland Health)
Additional notes
Other features on the blood film appearance that prompt further investigation.
| Film features |
Cause |
Investigation |
Target cells |
Iron deficiency anaemia
Haemoglobinopathies |
Ferritin Haemoglobinopathy testing (HPLC/Hb Electrophoresis) |
Elliptocytes or pencil cells |
Iron deficiency anaemia
Haemoglobinopathies |
Ferritin Haemoglobinopathy testing (HPLC/Hb Electrophoresis) |
Spherocytes |
Hereditary spherocytosis Autoimmune haemolysis |
Direct antiglobulin test (DAT)(Coombs test) Blood group and antibody screening (BGAB) Eosin 5 maleimide (E5M) |
Fragmented red cells |
Haemolysis |
Platelet count Bilirubin, Reticulocyte count Urea + Creatinine Coagulation profile |
Bite and blister cells |
G6PD deficiency |
G6PD assay |
Nucleated red blood cells |
Bone marrow infiltration
Haemolysis |
Consider bone marrow examination Thalassaemia testing (HPLC/Hb Electrophoresis) |
Sickle cells |
Sickle cell anaemia |
Haemoglobinopathy testing (HPLC/Hb Electrophoresis) |
Tear drop cells |
Bone marrow infiltration
Vitamin B12 deficiency |
May need bone marrow examination Active vitamin B12 |
Last updated November 2023