See also
Antibiotics
Invasive group A streptococcal infections: management of household contacts
Periorbital and orbital cellulitis
Sepsis
Key points
- Cellulitis is a spreading infection of the skin extending to involve the subcutaneous tissues. Many conditions present similarly to cellulitis — always consider differential diagnoses
- The typical presenting features of all skin infections include soft tissue redness, warmth and swelling, but other features are variable
- Allergic reactions and contact dermatitis are frequently misdiagnosed as cellulitis. If there is itch and no tenderness, cellulitis is unlikely
Background
Cellulitis
- The most common causes are Group A streptococcus (GAS) and Staphylococcus aureus. Predisposing factors include skin abrasions, lacerations, burns, eczematous skin, chickenpox, etc. although the portal of entry of organisms is often not seen
Impetigo (commonly called "school sores")
- Highly contagious infection of the epidermis, particularly common in young children. Causative organisms are GAS and S. aureus
- May be associated with scabies
Staphylococcal scalded skin syndrome (SSSS)
- Blistering skin disorder induced by the exfoliative (epidermolytic) toxins of S. aureus. Primarily affects neonates and young children
Necrotising fasciitis
- Rapidly progressive soft tissue infection characterised by necrosis of subcutaneous tissue
- Causative organisms include GAS, S. aureus, anaerobes and is often polymicrobial
- It causes severe illness with a high mortality rate (~25%)
- Recent infection with varicella is a risk factor
Cellulitis associated with water borne organisms
- Aeromonas species (fresh or brackish water, and mud)
- Mycobacterium marinum (fish tanks)
- Vibrio species (salt or brackish water)
- S. aureus, including MRSA
- GAS (coral cuts)
Infected animal/human bites
There are many other forms of skin infection that are not covered in this guideline
Assessment
Typical presentation of all skin infections
- Soft tissue redness
- Warmth and swelling
- Pain/tenderness
Mild Cellulitis
- Features above
- No systemic features
- No significant co-morbidities
Moderate Cellulitis
- Features above with moderate swelling and tenderness
- Systemic features (eg fever, tachycardia)
Severe Cellulitis
- Features above with severe swelling or tenderness
- Large body surface area involved (eg larger than the patient’s handprint)
- Marked systemic features (eg fever or hypothermia, tachycardia, tachypnoea, altered conscious state, unwell appearance, hypotension — this is a late sign). See Sepsis
Features suggestive of necrotising fasciitis include:
- severe pain out of keeping with apparent severity of infection
- rapid progression
- marked systemic features (eg high fever with rigors, tachycardia, tachypnoea, hypotension, confusion, vomiting). See Sepsis
Red flags
- Abscess or suppuration
- Animal or human bite
- Deep structure involvement
- Foreign body
- Immunosuppression
- Lymphangitis
- MRSA infection
- Multiple comorbidities
- Periorbital/facial/hand involvement
- Varicella associated infection
Differential Diagnosis
Large local reactions to insect bites are a common mimic of cellulitis. Features include:
- a punctum at the site
- itch as a prominent feature
- redness and induration, but rarely pain
Management
Investigations
- Swab for Gram stain (charcoal / gel / bacterial transport swab and slide) and culture if discharge present
- Blood culture is not useful in mild/moderate cellulitis
- Consider imaging (eg ultrasound) if abscess, deep infection or foreign body suspected
Treatment
- Manage
sepsis if features present
- Manage source if identifiable — ie remove foreign body, drain abscess
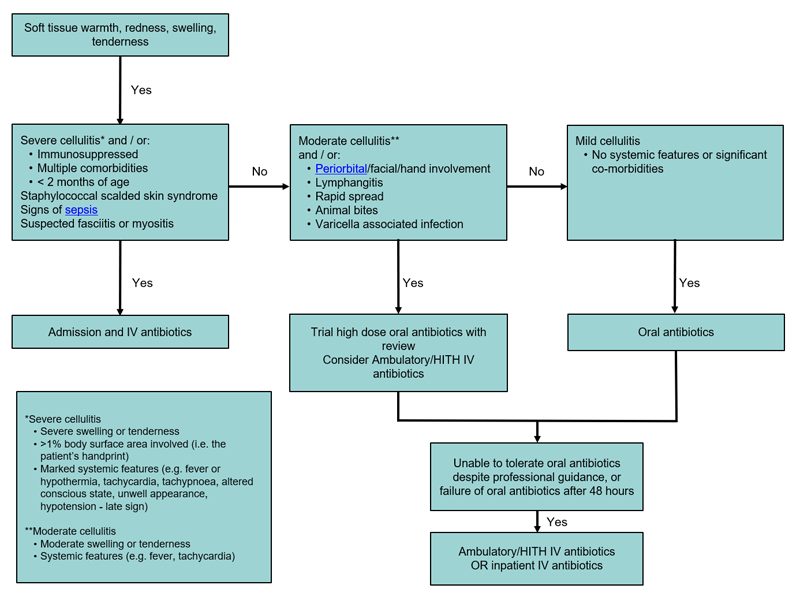
- For ongoing management refer to flowchart below
Summary of antibiotic therapy
Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns; please refer to local guidelines
Cellulitis frequently looks worse after 24 hours of treatment; consider waiting 48 hours to change therapies
Young, unvaccinated children are at risk of
Haemophilus influenzae type B (Hib)
|
Diagnosis |
Antibiotic |
Total duration |
Comments |
|
Impetigo |
Topical Mupirocin 2% ointment or cream to crusted areas tds OR
Cefalexin 33 mg/kg (max 500 mg) oral bd if widespread or large lesions |
5 days |
|
|
Mild cellulitis |
Cefalexin 33 mg/kg (max 500 mg) oral tds |
5 days |
|
|
Moderate cellulitis |
A trial of high-dose oral antibiotics with close review may be considered: Cefalexin 33 mg/kg (max 1 g) oral tds
Consider Ambulatory/Hospital-in-the-Home (HITH) if available:
Ceftriaxone 50 mg/kg (max 2g) IV daily
Cefazolin 50 mg/kg (max 2g) IV bd |
5–10 days |
If oral antibiotics not tolerated or no improvement after 48 hours, manage as per severe cellulitis
When improving, switch to oral antibiotics as per mild cellulitis |
|
Severe cellulitis
or
Staphylococcal scalded skin syndrome |
Flucloxacillin 50 mg/kg (max 2 g) IV 6H
(if rapidly progressive consider adding Clindamycin 10 mg/kg (max 600 mg) IV 6H)
|
5–10 days |
Consider early discharge to HITH once stable. When improving, switch to oral antibiotics as per mild cellulitis |
|
Necrotising fasciitis |
Vancomycin and Meropenem 20 mg/kg IV (max 1 g) 8H
AND
Clindamycin 10 mg/kg (max 600 mg) IV 6H |
|
Urgent referral to surgical team for debridement
Seek specialist advice for antibiotics
Consider IVIg |
|
Mammalian bites (uninfected / prophylactic) |
Often do not need prophylactic antibiotics. When indicated*:
Amoxicillin/Clavulanate
80 mg/mL amoxicillin oral liquid (7:1)
22.5 mg/kg (max 875 mg) oral bd |
5 days |
|
|
Animal/human bites (established infection) |
Amoxicillin/Clavulanate
80 mg/mL amoxicillin oral liquid (7:1)
22.5 mg/kg (max 875 mg) oral bd
If unable to tolerate oral antibiotics:
25 mg/kg (max 1g) IV 6–8H |
5 days (extend if severe, penetrating, involving deep tissues) |
Seek specialist advice |
|
Waterborne skin infections – seawater or fresh water |
Cefalexin 33 mg/kg (max 1 g) oral tds and Ciprofloxacin 10 mg/kg (max 500 mg) oral bd OR
Trimethoprim/sulfamethoxazole 8/40 mg/kg (max 320/1600 mg) oral bd |
5–10 days |
Clean and debride wound as needed
Prophylactic antibiotics are not recommended |
*Indications for prophylactic antibiotics in a animal/human bite
- Presentation delayed by >8 hours
- Puncture wound unable to be adequately debrided
- Bite on hands, feet, face
- Involves deep tissues (eg bones, joints, tendons)
- Involves an open fracture
- Immunocompromised patient
- Cat bites
Suggested antibiotic therapy where MRSA is suspected
Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns; please refer to
local guidelines
|
Diagnosis |
Antibiotic |
Total duration |
Comments |
|
Mild cellulitis |
Trimethoprim/sulfamethoxazole 4/20 mg/kg (max 160/800 mg) oral bd
OR
Clindamycin 10 mg/kg (max 450 mg) oral qid |
5 days |
|
|
Moderate cellulitis |
A trial of oral antibiotics with close review may be considered
OR
Vancomycin IV |
|
When improving, switch to oral antibiotics as per mild cellulitis |
|
Severe cellulitis
or
Staphylococcal scalded skin syndrome |
Vancomycin IV
OR
Clindamycin 10 mg/kg (max 600 mg) IV 6H |
When improving, switch to oral antibiotics as per mild cellulitis |
|
Risk factors for MRSA infection
- Residence in an area with high prevalence of MRSA, eg Northern Territory, remote communities in northern Queensland
- Previous colonisation or infection with MRSA (particularly recent)
- Aboriginal and Torres Strait Islander or Pacific Islander child
Consider consultation with local paediatric team when
- No improvement or deterioration after 24–48 hours of therapy
- Deep abscess or necrotising fasciitis suspected — consider surgical opinion
Consider transfer when
Child requires care above the level of comfort of local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
Able to tolerate oral antibiotics
Parent Information
Cellulitis
Impetigo
Staphylococcal infections
Bleach Baths
Last Updated March 2020