Key points
- Crying is normal physiological behaviour in young infants
- With typical history and normal examination, no investigations are required
- Parental education and close follow-up are vital to managing the unsettled or crying infant
- Excessive crying is associated with higher rates of parental post-natal depression
Background
At 6–8 weeks age, a baby cries on average 2-3 hours per 24 hours. “Colic” is an out-dated term used to describe excessive crying. The parents are often distressed, exhausted, and confused and often have received conflicting advice.
Assessment
Clinical characteristics of normal crying
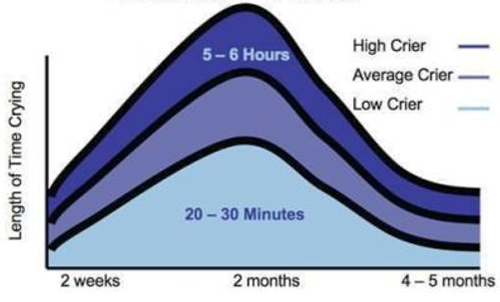
- Increases in the early weeks of life and peaks around 6-8 weeks of age and usually improves by 3-4 months of age
- Usually worse in late afternoon or evening but may occur at any time
- May last several hours
- Infant may draw up legs as if in pain, but there is no good evidence that this is due to intestinal problems
Red flags
- Sudden onset of irritability and crying
- Parental post-natal depression (PND) may be a factor in presentation
- Excessive crying is a strong risk factor for abusive head trauma (previously known as shaken baby syndrome)
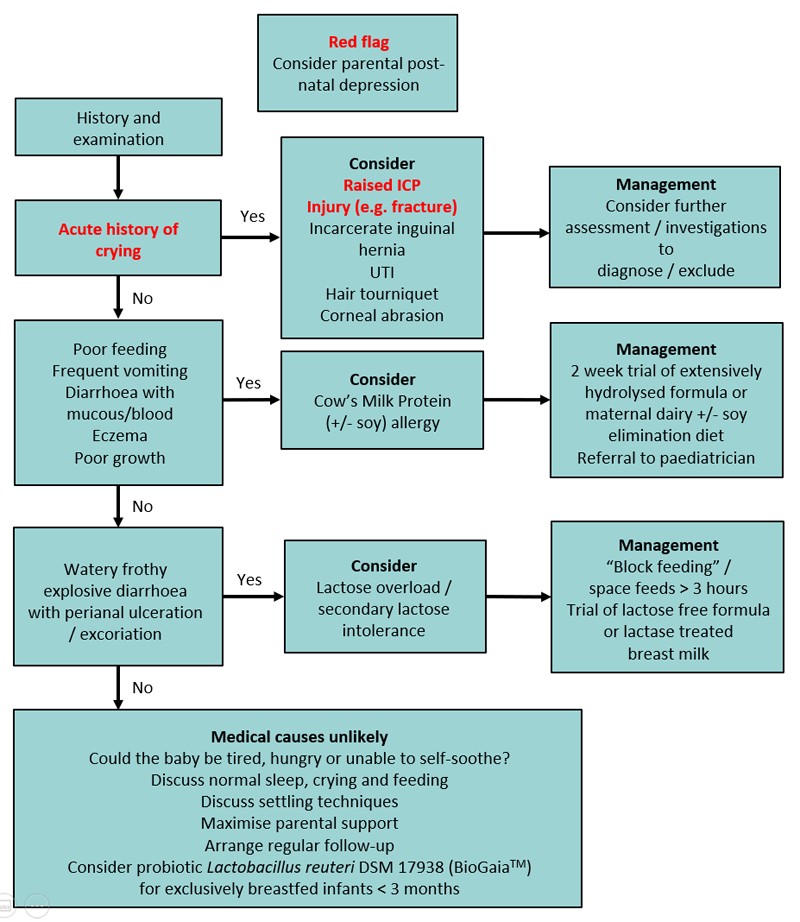
Consider if crying is acute onset
- Raised intracranial pressure (ICP)
- Injury eg clavicle fracture, non-accidental injury
- Incarcerated inguinal hernia
- Urinary tract infection
- Hair tourniquet
- Corneal foreign body/abrasion
Common non-pathological causes of
crying
- Excessive tiredness — consider if the infant's total sleep duration per 24 hours falls more than an hour short of the "average" for their age
- Average sleep requirements:
- at birth: 16 hours
- at 2–3 months: 15 hours
- a 6 week old baby generally becomes tired after being awake for 1.5 hours
- a 3 month old baby generally becomes tired after being awake for 2 hours
- Hunger — more likely if there is poor weight gain
Differential diagnoses to consider
Non-IgE cow milk / soy protein allergy
- Both can be found in human breast milk if in the mother’s diet
- Goat milk protein is as allergenic as cow milk protein
- Suspect if there is:
- significant feeding problems that persist day and night
- frequent vomiting
- diarrhoea with blood or mucus
- poor weight gain
- wide-spread eczema
- Clinical diagnosis by trialing eliminating cow / soy milk for 2 weeks:
- modifying the mother's diet
- or changing to an extensively hydrolysed formula (requires paediatrician consultation)
- and requires resolution of symptoms or re-emergence of symptoms on rechallenge
Lactose overload / malabsorption
- Consider lactose overload if infant has very frequent breastfeeds and frothy, watery diarrhoea with perianal excoriation
- Primary lactose intolerance is extremely rare
Gastro-oesophageal reflux disease (GORD)
- No causal relationship between gastro-oesophageal reflux (GOR) and infant crying and irritability has been demonstrated
- Gastro-oesophageal reflux disease is rare
- Proton pump inhibitors have been shown to be ineffective in reducing crying
Acute management
Investigations
If the history is typical and examination normal, no
investigations are required.
Management
- Exclude medical cause
- Parental education and reassurance. It is often helpful to explain to caregivers the potential causes of crying that have been excluded and the reasons for excluding each condition
- Assess parental emotional state and mother-baby relationship:
- invite the parent/s to talk about how stressful it is to care for a baby who cries persistently
- ascertain whether the parent is worried that she/he is depressed
- screen for postnatal depression using the
Edinburgh Postnatal Depression Scale
Parental
Education
- Engage in a partnership with the parent/s
- This includes acknowledging their concerns, taking time to observe the baby-parent interactions and offering follow-up. Observing the baby feed is helpful for parents who are concerned about their baby’s feeding
- Explain normal crying and sleep patterns
- Use the normal crying curve to explain the natural history of infant crying (taken from Purple Crying - see parent information below)
- Use a sleep/cry diary to explain the infant's cry/sleep/feeding patterns
- Encourage parents to recognise signs of tiredness (frowning, clenched hands, jerking arms or legs, crying, grizzling)
- Assist parents to help their baby deal with discomfort and distress
- Establish pattern to feeding/settling/sleep
- Aim to settle the baby for daytime naps and night-time sleep in a predictable way (eg, quiet play, move to the bedroom, wrap the baby, give the baby a brief cuddle, then settle in the cot while still awake)
- Avoid excessive stimulation - noise, light, handling. Excessive quiet should also be avoided. Most babies find a low level of background noise soothing.
- Darken the bedroom for daytime sleeps
- Carry baby in a papoose in front of the chest
- Baby massage/rocking/patting
- Gentle music
- Respond before baby is too worked up
- Give the primary carer permission to rest once a day without the need to carry out household chores. Have somebody else care for the baby for brief periods to give the parent/s a break
- Provide
printed information as parents are unlikely to remember much given their state of mind at the time
Medications
and other treatment options
Medication is not indicated, this includes:
- Anti-reflux medications — ineffective in reducing crying compared with placebo
- Anticholinergic medications — due to risk of serious adverse events eg apnoeas, seizures
- Colic mixtures (eg gripe water) – no proven benefit
- Simethicone (eg Infacol™) - no effect on crying compared with placebo
- There is limited evidence to support probiotic use
- Only in exclusively breastfed infants under 3
months, the probiotic Lactobacillus reuteri DSM17938 (BioGaia™)
has been shown to be effective with excessive crying (colic)
- To be given as 5 drops per day orally to the infant for 21 days only
- It should not be given to formula-fed infants
- The probiotic has not been shown to be effective in both breastfed and formula-fed infants in Victoria, Australia
- Probiotic effects are strain-specific; Lactobacillus reuteri DSM17938 is the only probiotic strain with some evidence of efficacy in exclusively breastfed infants with excessive crying (colic)
- Formula changes are usually not helpful unless there is proven cow milk allergy. Weaning from breast milk has no benefit
- Spinal manipulation is not indicated and has associated risks
Consider consultation with local
paediatric team when
- Medical cause of crying identified or suspected
- Baby clinically unwell
- Admission to hospital — if infant considered at risk of non-accidental injury or parental exhaustion
Consider transfer when
Infant requiring care beyond the comfort level of the hospital
For emergency advice
and paediatric or neonatal ICU transfers, see Retrieval Services.
Follow up
Referral for early (within days) ongoing support is essential. Options include:
Parent information
Parent resources
Purple Crying
Raising
Children’s Network
Additional notes
REducing MEDications in Infants (REMEDI)
|
Information specific to RCH
Unsettled Babies Clinic — for unsettled infants
<6 months old
General medicine clinic
Social work referral (consider if presenting to Emergency Department)
Sleep Clinic — for unsettled infants >6 months old with sleep issues |
Last updated August, 2019