Pierre Robin (Pee-air Roe-bahn) sequence, also called Pierre Robin syndrome, or PRS, is a condition where babies are born with a small lower jaw, have difficulties breathing (airway obstruction) and often (but not always) have a cleft of the palate (an opening in the roof of the mouth). The breathing problems start either from or shortly after birth and are often also associated with feeding difficulties and problems gaining weight.
About a third of PRS cases occur as part of another syndrome, which may have other features. Your child's doctor will discuss this with you.
Signs and symptoms of PRS
Your baby may have a small jaw and cleft palate, along with breathing difficulties, which can be present from birth. These may show in one or more of the following ways:
- Your baby may appear to be working hard to take breaths and look worn out and tired with breathing
- Their chest appears to be sucking in with each breath
- A grey or blue colour appears around their lips, even if your baby is still breathing
- Their breathing may be noisy (especially when breathing in)
If you see any of these signs of breathing difficulty, call an ambulance immediately.
Children with PRS can have poor weight gain due to the cleft palate causing feeding problems, but also because their breathing problems become harder to manage when they try to breathe and feed simultaneously.
You might notice some of the following signs in your baby:
- they take a long time to feed, get tired easily and don't take all the milk
- difficulty attaching to the breast
- coughing, choking or arching the back when feeding
- poor weight gain
- reflux (milk coming back up) from the nose and mouth
If your baby does not receive the appropriate medical treatment, they may have ongoing problems with nutrition and weight gain, or they may stop breathing.
When to see a doctor
Because PRS is quite rare, it is sometimes not diagnosed at birth – especially if there do not appear to be immediate breathing problems.
If your baby has a small jaw, and/or a cleft palate, feeding issues or difficulty gaining weight, it is important they are investigated by your GP and referred on to a paediatrician if appropriate.
Please note: if your baby has a cleft of the palate (irrespective of whether they have a small jaw) you should contact your local Cleft Service as soon as possible as they will be able to link you in to all the services your child requires.
What causes PRS?
The cause of PRS is still not fully understood. It is thought to start as a small jaw, which causes the tongue to stop the roof of the mouth (palate) closing during normal development. Why the jaw is small in the first place is not known, but it may be genetic.
Some babies have a family history of PRS or similar problems, although most don't.
Babies with PRS are screened for other possible problems such as eye, kidney, bone and occasionally heart conditions. However, for most babies, no other problems are found.
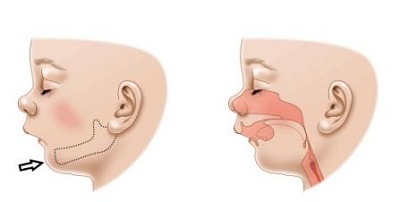
Difficulty breathing can occur after birth because the small and recessed jaw makes the tongue sit further towards the back of the throat, narrowing or blocking the airway. The breathing problems may be better or worse at different times, and may be worse when your baby is in certain positions
(e.g. lying flat on their back), or when feeding or crying.
Treatment for PRS
The treatment will depend on the level of breathing and feeding difficulties. Your baby may need to stay in hospital for observation and treatment, including:
- nutrition and feeding support
- close observation of weight gain
- monitoring of vital signs (e.g. heart rate) and ongoing breathing assessments
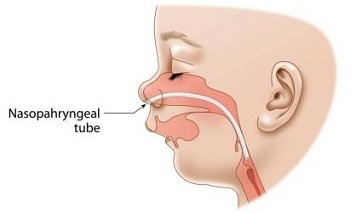
Sometimes, assistance to keep the airway clear is required. This involves the insertion of a tube known as a nasopharyngeal (nay-so-faran-jeel) tube.
The majority of babies with PRS outgrow the breathing problems within three to six months as their airway grows. Occasionally breathing problems persist, or the airway obstruction becomes severe and life threatening. In these cases, your baby may need surgical treatment, such as jaw
distraction or, rarely, a tracheostomy. See our fact sheets
Jaw distraction surgery and
Tracheostomy.
Follow-up
Babies with PRS need to have follow-up appointments with neonatologists (doctors specialising in newborn babies) and the respiratory team to ensure that any breathing and feeding problems are getting better.
If your baby has a cleft of the palate, consultation with the cleft team, including plastic and ENT (ear, nose and throat) surgeons, speech pathologists and a paediatrician will be required. Repair of the cleft palate in babies with PRS is often delayed until around 18 months of age and is planned in consultation with the whole cleft care team. See our fact sheet
Cleft lip and palate.
Your baby will need to have regular hearing assessments, as hearing difficulties often occur due to fluid in the middle ear that does not drain out in the usual way. It is common for an ear, nose and throat (ENT) surgeon to insert ventilation tubes in the ears (called grommets) during the
operation to close the palate. These tubes help fluid drain from the middle ear.
All babies with PRS should have at least one appointment with a children's eye doctor for a review.
If problems other than a small jaw and cleft palate are found, or if there is any family history of such problems, consultation with a genetics team will be arranged.
Key points to remember
- A baby with a cleft palate and small jaw should be evaluated for breathing and feeding complications
- In most cases, failure to gain weight combined with a cleft palate and small jaw is a sign of upper airway obstruction, and needs specialist medical attention
- Most babies with PRS outgrow the breathing problems as their airway grows
- Babies with PRS need follow-up appointments to monitor their feeding and breathing problems, hearing and eyesight. They will need to see a plastic surgeon for cleft palate repair
For more information
Common questions our doctors are asked
Why is PRS called a sequence?
It is referred to as a sequence because a sequence of events happens during pregnancy that leads to the condition. The baby's jaw doesn't grow as much as it should (around the nine-week mark of gestation), which causes the tongue to sit high in the mouth, which in turn prevents the palate
from closing properly.
What other genetic conditions are linked with PRS?
The two most common syndromes associated with PRS are velocardiofacial (Shprintzen) syndrome and hereditary arthro-ophthalmopathy (Stickler) syndrome. Velocardiofacial syndrome is also commonly associated with heart defects. Your child's doctor will evaluate your
child for any other features that might suggest their PRS is linked with another condition.
Developed by The Royal Children's Hospital Neonatal Medicine and Respiratory and Sleep Medicine departments. We acknowledge the input of RCH consumers and carers.
Reviewed September 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.