The two settings that help you work out how much rapid acting insulin (NovoRapid® or Humalog®) you need for boluses across the day are called;
Carbohydrate ratio: which is the insulin that is needed for food
Correction factor (or sensitivity): which is the insulin needed to help correct your glucose down to the target range
Carbohydrate ratio
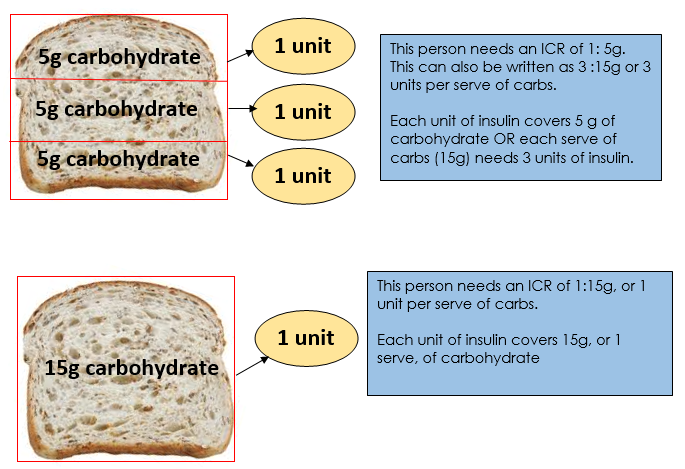
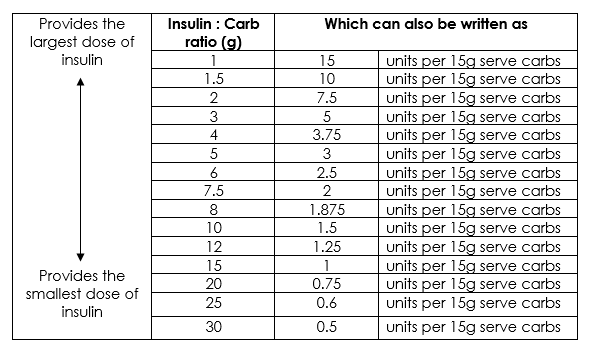
The Insulin to Carbohydrate Ratio (ICR) is the number of grams of carbohydrates that is covered by 1 unit of insulin. For people who prefer to count carbs in serves (instead of grams) the carb ratio can also be written as units of insulin per serve of carbohydrate.
Carb ratios vary amongst people and can be affected by the time of the day, and other factors like changes in weight, age or exercise.
Below is an example of two different ICR’s applied to the same food.
To calculate the ICR the 500 rule is sometimes used. You take the number 500 and divide it by the current total daily dose (TDD) of insulin. For example, if you usually have 20 units of glargine and 10 units of NovoRapid® with each of your three meals then your TDD is 50.
- 500 divided by 50 = 10, thus your ICR would be 1:10g
- This could also be written as 1.5 units per 15g serve of carbs
Often younger children with a lower TDD and older children (if the TDD is less than 1 unit of insulin per kilogram of body weight) need to use the 300 rule, rather than 500. This can all be discussed with your treating team.
To assess if your ICR is correct you need to check your BGL 2-3 hours after eating. Ideally the BGL will be within 3mmol of the pre meal BGL. If it rises more than 3 mmol/L, you need to consider making your carb ratio stronger.
Correction factor
The correction factor (CF) is sometimes called the Insulin Sensitivity Factor (ISF). It is a measure of how much one unit of insulin will lower your BGL and is used when your BGL is above a certain target level - often around 6 mmol/L.
For example, a CF of 2 means that extra 1 unit of insulin will be given to lower your BGL by 2mmol/L. So if your BGL is 8mmol/L and you give 1 unit of insulin, the aim would be for your BGL to be ~ 6mmol/L in the next 2-3 hours.
To calculate your correction factor, divide 100 by your TDD. So for the example above of a TDD of 50 units, your correction factor would be set to 2.
To assess if your correction factor is right, you need to check your BGL 2-3 hours after giving a correction. Ideally the BGL will be close to your target BGL. If not, your correction factor might need to change.
What about snacking?
Snacks are not compulsory if using MDI. If you want to snack between meals then aim to keep it less than 15 grams of carbohydrate. If you want to eat more, you may need to give extra rapid acting insulin.
If you are consistently feeling hungry in between your meals then consider increasing the size of your main meal or including more low GI carbohydrates with your meals such as wholegrain breads, grains, dairy foods, legumes, vegetables and some fruits to improve your feeling of fullness.
Getting the most out of flexible bolusing
- Check your BGLs before each meal and at bedtime as a daily minimum.
- Check your BGLs 2-3 hours after your main meal (without snacking in between) to assess if your insulin dose and food are well matched. If your BGL is more than 3mmol/L higher or lower than your pre-meal reading on 3 occasions (at that same meal) then your insulin dose may need to be adjusted.
- Check if your background insulin (e.g. glargine or Levemir®) dose is correct by comparing your pre bed BGL with your overnight or morning fasting BGL. If these readings are more than 4mmol higher or lower than the previous night, you need to change the dose by 1-2 units. If you change the background insulin, always give it at least 3 days to see the new pattern before making any further changes.
- Stay in touch with your diabetes team, especially during the first few weeks of changing over to MDI.
Click here for more information about what tools are available for flexible bolusing
RCH acknowledges the Children’s Diabetes Centre, at Perth Children's Hospital, WA for their permission to adapt their resource “Guide to Flexible Insulin Therapy for Families”