Fracture Guideline Index
1. Summary
Major pelvic fractures often caused by a high degree of force and often occur in a patient with multiple traumatic injuries. They can be associated with significant haemorrhage from co-existing vascular injury or other associated injuries, and it is vital the patient is approached in a systematic fashion appropriate for trauma care, well before any radiological confirmation of injury.
This guideline will discuss management of specific pelvic injuries.
Click here to access the RCH Paediatric Trauma Manual
Click here for the guideline on Early Management of Pelvic Injuries in Children
For emergency advice in major trauma see
Retrieval Services
Pelvic avulsion injuries
2. How are they classified?
Pelvis fractures can be classified according to:
- Maturity (as a rough guide, look to see if the triradiate cartilage has yet closed)
 |
 |
| Open triradiate cartilage |
Fused triradiate cartilage |
- Stability (any displaced posterior ring injury, break in both anterior and posterior pelvic ring or misshapen pelvis represents an unstable injury)
- Fracture Classification Systems:
- Torode and Zieg classification for the immature pelvis (triradiate cartilage closed)
- Young-Burgess classification for the skeletally mature pelvis (triradiate cartilage closed)
Torode and Zieg classification (for Torode & Zieg Type I avulsion injuries see pelvic avulsion injuries
|
Fracture Pattern |
Description |
Stability |
|
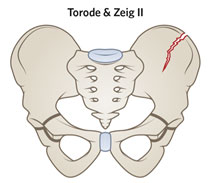 |
Torode & Zieg II
Fracture of Iliac Wing,
usually from direct
lateral force |
Stable |
|
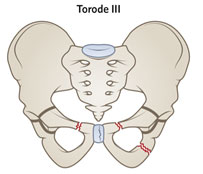 |
Torode & Zieg III
Simple ring fracture with either pubic symphysis disruption or pubic ramus fracture |
Usually Stable |
|
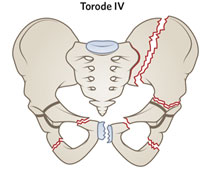 |
Torode & Zeig IV
Combined posterior and anterior ring fractures or joint disruption.
Can include combined ring and acetabular fractures, and straddle injuries with bilateral superior & inferior pubic ramus fractures |
Unstable |
Young & Burgess Fracture classification (adult injury patterns)
Fracture type |
ED management |
Follow-up |
|
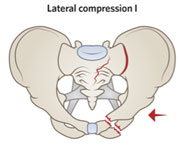
Ramus fracture with sacral ala compression fracture
Stable |
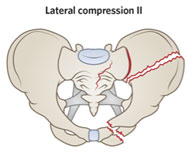
Ramus fracture with posterior iliac fracture-dislocation
Unstable |
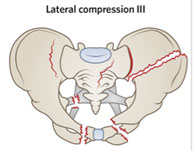
Lateral compression fracture with contralateral anterior compression pattern
Unstable |
|
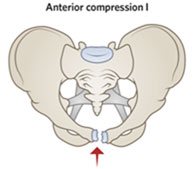
Some pubic symphysis widening
Stable |
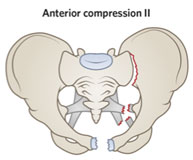
Gross pubic symphysis widening and anterior sacroiliac joint diastasis
Unstable |
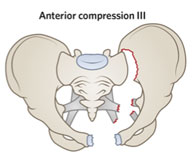
Disruption of posterior and anterior sacroiliac ligaments
High risk of associated vascular injury
Unstable |
|
|
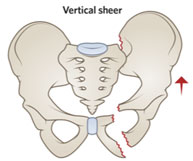
Complete disruption of SI joint and anterior ring fracture
High risk of associated vascular injury
Unstable |
|
3. How common are they and how do they occur?
Pelvic injuries in children are relatively uncommon. Fractures of the pelvic ring and acetabulum have an incidence of approximately 1 per 100000 children per year.
They are most often caused by a high-force mechanism such as a motor-vehicle accident or a fall from a height, hence the importance of managing these injuries within established trauma protocols.
They may also occur from straddle injuries.
4. What do they look like - clinically?
Pelvic fracture should be suspected in any polytrauma patient particularly where there is
-
hypotension,
-
pelvic or abdominal pain
-
lower limb deformity or neurological abnormality, or
-
the patient is obtunded.
Specific signs suggestive of pelvic fracture are
-
bruising or swelling over the pelvic prominences
-
leg length discrepancy
-
wounds over the pelvis
-
rectal or vaginal bleeding
-
blood at the urethral meatus
-
scrotal swelling.
5. What radiological investigations should be ordered?
An AP Pelvis X-Ray should be obtained as early as practical as part of the secondary survey in significant trauma.
CT will give more detail of any unstable pelvic fracture and will assist with operative planning as well as being useful for detecting other traumatic injuries.
Specialised radiological investigation may be required if a urethral injury is suspected or there is suspicion of open fracture via vaginal or rectal injuries.
6. What do they look like on x-ray?
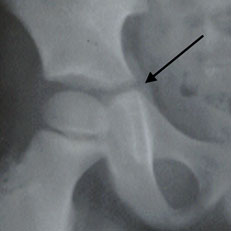
Immature Pelvis: Torode & Zeig II

Iliac wing fracture , left;
Torode & Zeig III
 *
*  *
*
L: undisplaced superior ramus # R (Torode & Zeig III) R: displaced R and L inferior and superior rami# (Torode&Zeig III)
Torode & Zeig IV

Fracture near left SI joint and fracture through left superior and inferior pubic rami
 Torode IV injury with pubic diastasis and SI joint disruption
Torode IV injury with pubic diastasis and SI joint disruption
Mature Pelvis: Lateral Compression type

Lateral Compression fracture with fracture through right Iliac wing and the right pubic rami (obscured by pelvic binder)

Another Lateral Compression fracture with diastasis right SI joint, fracture left superior and inferior SI joints.
The lateral force has also caused contralateral Left SI joint diastasis and pubic rami fractures, with the shape leading to the term “windswept pelvis”.
AP Compression type

Anterior Compression fracture type II
Vertical Shear type

Fracture of Acetabulum:

Fracture of left acetabulum with intact pelvic ring.

More subtle non-displaced left acetabular fracture after minor trauma
7. When is reduction (non-operative and operative) required?
Where a fracture is displaced or unstable as outlined above, surgical management is highly likely to be necessary. This may be with a staged approach with emergent external fixation on the day of injury to stabilise the fracture and the patient and later definitive fixation, when the clinical situation has stabilised.
Nonoperative management is likely to be appropriate for simple nondisplaced fractures of the anterior ring, and avulsion fractures, but this should be arranged in close consultation with the orthopaedic service.
Any displaced fractures of the acetabulum will also require careful orthopaedic surgical management (with any fracture-dislocations being reduced urgently). Undisplaced acetabular fractures managed conservatively will require a non-weight-bearing period under close radiological supervision.
8. Do I need to refer to orthopaedics now?
Indications for prompt consultation include:
- Unstable pelvic fracture
- Complex polytrauma in which pelvic fracture is suspected
- Suspected open fracture
- Any suspicion of acetabular injury (these may not be evident on plain X-ray, but will be suggested by pain with attempts to walk)
! Observing the patient walking independently is an important part of the tertiary trauma survey |
9. What is the usual ED management for this fracture?
Again it must be emphasized that these injuries should be approached using a team-based complex trauma algorithm due to the chance of major coexisting injuries or associated haemorrhagic shock. This approach, along with the appropriate early use of a pelvic binder
are addressed in the RCH guideline on the early management of pelvic injuries in children, and should be commenced before the diagnosis is confirmed.
Pelvic binders are less useful in a lateral compression pelvic fracture: if this injury is identified, it is reasonable for the binder to be gradually released and then removed under haemodynamic monitoring if there is consensus between the trauma team leader and the orthopaedic surgeon.
If there is suspicion of a urethral injury, liase with a paediatric surgeon or urologist before attempting any catheterisation.
If an open fracture involving tears to the vagina or rectum are suspected, antibiotics will be required and tetanus status checked, along with management of those injuries.
10. What follow-up is required?
- Stable fractures such as most Torode-Zieg I, II and III, isolated pubic ramus fractures or minimally displaced diastasis of symphysis pubis may be able to return to weight bearing relatively early. Discharge timing will depend on stability for other injuries, and completion of a tertiary survey. Follow up will be required in orthopaedic outpatients as well as physiotherapy.
- Any unstable fractures or acetabular fractures will have follow up arranged by the orthopaedic service after inpatient management. This will often need to take place over many years to monitor for long term complications.
11. What advice should I give to parents?
Unstable pelvic fractures usually occur along with other injuries; parents will need to be informed that their child will be managed in a tertiary trauma hospital by multiple specialties and that surgical management is likely to be required.
Highly detailed information about long term follow up may overwhelm parents at this early stage; it is often better to check that they have adequate supports in place and arranged for other children to be cared for by a relative.
Stable pelvic fractures may not require surgical management, but any child with traumatic injury to the pelvis should still be admitted for inpatient surveillance, orthopaedic consultation and tertiary survery. (The exception to this is simple avulsion fracture in the athlete)
12. What are the potential complications associated with this injury?
Immediate morbidity or mortality from haemorrhagic shock or coexisting injuries
Co-existing injury of the urethra, bladder, rectum or vagina
Long term complications including malunion, leg-length discrepancy, osteoarthritis or acetabular dysplasia
13. References (ED setting)
Silber J. & Flynn J. Changing Patterns of Pediatric Pelvic Fractures with Skeletal Maturation: Implications for Classification and Management. J Pediatr Orthop 2002;22:22-26
Torode I & Zieg D. Pelvic Fractures in Children J Pediatr Orthop 1985;5(1)76-84
Amorosa, L. High Energy Pediatric Pelvic and Acetabular Fractures Orthop Clin N Am 2014;45(4);483-500
DeFrancesco, C et al, Traumatic pelvic fractures in children and adolescents Seminars in Pediatric Surgery 26 (2017) 27-35
Victorian State Paediatric Trauma Guideline
Last updated November 2020