|
Head and face |
- Face, scalp and skull: bleeding, lacerations, bruising, swelling, depressions / irregularities in the skull (to suggest skull fracture), bruising behind the ears (Battle’s sign: may indicate base of skull fracture), periorbital bruising (“Racoon eyes”: may indicate base of skull fracture)
- Eyes: Palpate bony margins of orbit for fracture. Test eye movements, pupillary reflexes and vision. Inspect for penetrating injury (see
Penetrating eye injury), irregular iris, foreign bodies, subconjunctival haemorrhage, hyphaema
- Ears: bleeding, blood behind tympanic membrane (suggestive of base of skull fracture), tympanic membrane perforation (in blast injuries). Assess hearing
- Nose: bleeding, septal haematoma, CSF leak, palpate for bony crepitus or deformity
- Mouth: wounds to the lips, gums, tongue or palate
- Teeth: subluxed, missing or fractured teeth
- Jaw: identify pain, trismus or malocclusion and palpate for bony step
|
|
Neck |
Inspect neck whilst maintaining manual in-line stabilisation of spine. Open collar to do this
Examine anterior neck for blunt or penetrating trauma by looking/feeling for the following (TWELVE-C):
- Tracheal deviation
- Wounds
- Emphysema (subcutaneous)
- Laryngeal tenderness/crepitus
- Venous distension
- OEsophageal injury (unlikely if child can swallow easily)
- Carotid haematoma/bruits/swelling
Assess c-spine (See
C-spine assessment) |
|
Chest |
- Observe work of breathing and effectiveness of breathing, assess for any asymmetrical or paradoxical chest wall movement
- Inspect for signs of injury such as bruising, seatbelt marks, wounds
- in cases of stabbing or other assault, look for ‘hidden’ wounds by checking areas such as axillae (assess back and buttocks with log roll)
- Palpate for bony tenderness over ribs, crepitus (indicating subcutaneous emphysema)
|
|
Abdomen |
- Inspect for bruising (eg from seatbelt or handlebar injury), abdominal distension
- Palpate for signs of peritonism such as guarding or rigidity
- Palpate for tenderness over the liver, spleen, kidneys and bladder
|
|
Pelvis and perineum |
- Inspect for grazes over iliac crests, bruising, deformity
- Feel for pain or crepitus on gentle palpation of bony prominences
- Assessment for pelvic instability is performed by gentle compression of the iliac crests
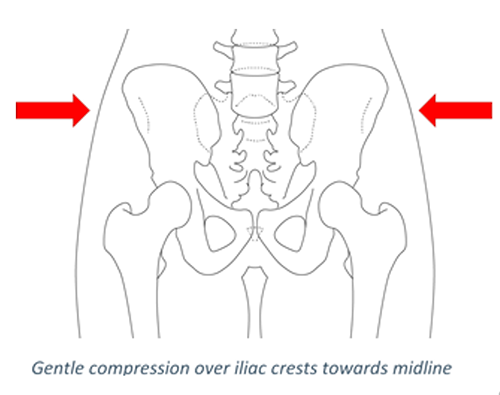
- stressing/springing the pelvis is not recommended
- See
Early management of pelvic injuries in children
- Inspect urinary meatus/introitus for blood
- Examine for priapism, which may indicate a spinal injury
|
|
Limbs |
- Inspect for wounds, bruising, open fractures, burns, abrasions
- Feel for soft tissue and bony tenderness or swelling, joint movement and stability
- Examine pulses and perfusion
- Examine sensory and motor function of any nerve roots or peripheral nerves that may have been injured
|
|
Back and spine |
- A log roll should be performed, but only once
- Inspect entire length of back and buttocks
- Inspect anus when indicated
- Palpate then percuss spine for tenderness
- Palpate scapulae and sacroiliac joints for tenderness
- Digital rectal examination should be limited to children with neurological deficits concerning for spinal injury, and should only be performed once if required
|