See also
Emergency medication and resuscitation resources
Resuscitation
Asthma
Urticaria
Acute upper airway obstruction
Key points
- Anaphylaxis is a severe allergic reaction characterised by an acute onset of cardiovascular (eg hypotension) or respiratory (eg bronchospasm) symptoms. It may be associated with typical skin features (urticarial rash or erythema/flushing and/or angioedema) and/or persistent severe gastrointestinal symptoms
- Treatment of anaphylaxis is intra-muscular adrenaline 10 microgram/kg or 0.01 mL/kg of 1:1000 (maximum 0.5 mL), into lateral thigh which should be repeated after 5 minutes if the child is not improving
- In children with possible anaphylaxis and known asthma, always give adrenaline first, then asthma medicines
- Do not allow children with anaphylaxis to stand or walk
Background
Most reactions occur within 30 minutes of exposure to a trigger but can occur up to 4 hours later
Causes of anaphylaxis in children include:
- Foods: Peanut, tree nuts, cow milk, eggs, soy, shellfish, fish, wheat
- Bites/stings: Bee, wasp, jack jumper ants, ticks
- Medications: Beta-lactams, NSAIDs
- Other: Exercise, idiopathic, rubber latex (bottle nipples, pacifiers, toys)
Newer monoclonal
antibody therapies may produce delayed anaphylactic reactions and rebound
symptoms that occur more than 12 hours after the initial reaction
NB: a cause is not identified in 20% of cases
Assessment
Identify risk factors for fatal anaphylaxis
- Delay to administration of adrenaline or emergency response services
- Poorly controlled asthma (see
Asthma)
- Allergy to nuts, shellfish, drugs and insect stings
- Adolescence
- Pre-existing cardiac and respiratory conditions
Anaphylaxis is a clinical diagnosis made in the setting of the acute onset of either criteria:
- Typical skin features (urticaria, flushing and/or angioedema) plus involvement of:
- Respiratory system
and/or - Cardiovascular system
and/or - Persistent severe gastrointestinal symptoms (especially after exposure to non-food allergens eg insect sting)
OR - Hypotension, bronchospasm or upper airway obstruction where anaphylaxis is possible, even if typical skin features are not present
A detailed history of pre-hospital events is vital to confirm anaphylaxis and its associated trigger(s)
Clinical features
| System |
Features of anaphylaxis |
|
Respiratory (most common in children) |
Persistent cough
Wheeze, stridor, hoarse voice, difficulty talking or change in character of cry
Tongue swelling
Chest pain or dyspnoea
Subjective feeling of swelling, tightness or tingling the throat or mouth |
|
Cardiovascular |
Pale and floppy (infant)
Palpitations, tachycardia, bradycardia
Hypotension, pallor
Collapse with or without unconsciousness
Cardiac arrest |
|
Neurological |
Dizziness
Altered consciousness, confusion, sudden behaviour change |
|
Gastrointestinal |
Nausea, vomiting, dysphagia
Diarrhoea
Abdominal or pelvic pain |
|
Dermatological |
Urticarial rash
Erythema, flushing, tearing
Angioedema
Pruritus (skin, eyes, nose, throat, mouth) |
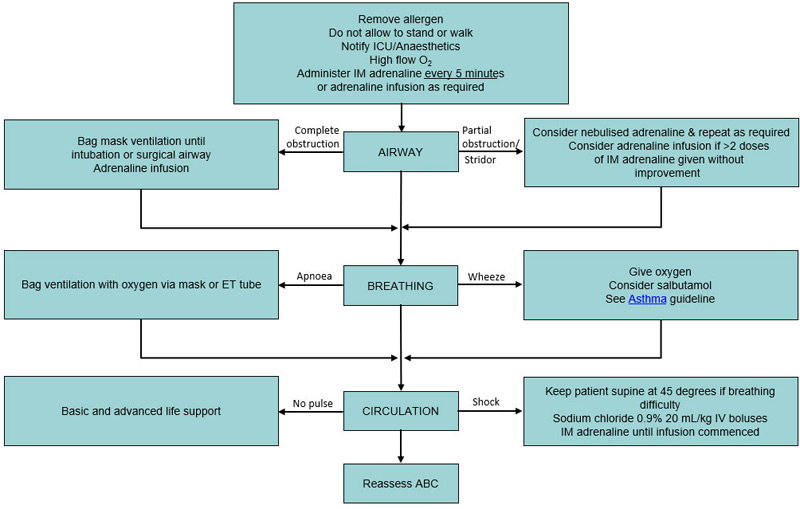
Management
Investigations
Anaphylaxis is a clinical diagnosis. A serum tryptase has no role in acute management of anaphylaxis. It should only be ordered after consultation with a paediatric allergy specialist in special circumstances.
Treatment
- Remove allergen if still present (eg insect stinger, food debris in mouth)
- Lay patient flat. Do not allow the child to stand or walk. Fatality can occur within seconds if the child stands or sits suddenly. Treat the child in the supine position or lying on their side. If a vomiting child is sat upright, monitor for hypotension
- Intramuscular adrenaline 10 microgram/kg or 0.01 mL/kg of 1:1000 (maximum 0.5 mL), into lateral thigh which should be repeated after 5 minutes if the child is not improving
- Do not use subcut adrenaline, as absorption is less reliable than the IM route
- Do not use IV bolus adrenaline unless cardiac arrest is imminent
- Use an adrenaline autoinjector if unable to calculate exact dose or to avoid delay, including in children
<1 year old
The following doses of adrenaline may be used
| Adrenaline doses |
|
|
Age (years) |
Weight (kg) |
Volume of 1:1000 adrenaline (mL) |
Adrenaline autoinjectors |
|
<1 |
<7.5 kg |
0.1 mL |
Not available |
|
<1 - 2 |
7.5 – 10 |
0.1 mL |
150 microg device
|
|
2 – 3 |
15 |
0.15 mL |
|
4 – 5 |
18 |
0.18 mL |
|
5 – 6 |
20 |
0.2 mL |
300 microg device
|
|
7 – 10 |
30 |
0.3 mL |
|
10 – 12 |
40 |
0.4 mL |
| >12 and adults | >50 | 0.5 mL | 300 microg or 500 microg device |
Example autoinjectors
| Brand name |
Indications |
Image |
|
EpiPen Jr® 150 microg |
Children
<5 years old and 7.5 – 20 kg |
(Green) |
|
EpiPen® 300 microg |
Children >5 years or >20kg |

(Yellow) |
|
Anapen®
|
Children <5
years old and 7.5 – 20 kg: 150 microg
Children >20 kg: 300 microg
Children >50 kg: 500 microg
|

(White) |
- Give oxygen
- If not improving, give a second dose of adrenaline, consult senior staff and consider adrenaline infusion (0.05 - 0.5 microgram/kg/min)
- Continue giving IM adrenaline every 5 minutes until IV access is obtained
Other treatments to consider
Repeated doses of IM adrenaline together with
- Nebulised or MDI salbutamol is recommended if the child has respiratory distress with wheezing. Also consider other anti-asthma medications. See Asthma
- Antihistamines may be given for symptomatic relief of pruritus. Second generation antihistamines are preferred (eg cetirizine). Avoid promethazine as it can cause hypotension
- Corticosteroids and leukotriene antagonists have no proven benefit in anaphylaxis
- Avoid NSAIDs
Observation and admission
All children with anaphylaxis should be observed for at least 4 hours in a supervised setting with facilities to manage deterioration
Admission for a minimum 12-hour period of observation is recommended if:
- Further treatment is required within 4 hours of last adrenaline administration (biphasic or prolonged reaction)
- Previous history of biphasic reaction
- Poorly controlled asthma
- The child lives in an isolated location with delay to emergency services
- Anaphylaxis
to monoclonal antibody
The acute care setting should provide resources, education and follow up options to the family including:
- Update the medical record highlighting suspected allergen to avoid, and health department notification if applicable
(see additional notes below)
- Anaphylaxis action plans for home, school and/or other care settings if applicable
- Two EpiPens®/ EpiPens Jnr®/ Anapens® and training in correct use with an Epipen/Anapen trainer. Current dose recommendations are:
7.5 - 20 kg = EpiPen Jnr® or Anapen® (150 microgram)
>20 kg = EpiPen® or Anapen® (300 microgram)
>50 kg = EpiPen® or Anapen® (300/500 microgram)
EpiPen® / EpiPen Jnr® / Anapen® are available on PBS for all children with a history of acute anaphylaxis.
See Guidelines for the prescription of an EpiPen for more information
They require authority prescription or can be purchased without a prescription at full cost.
See PBS authority indications
- Consider provision of a
Medicalert bracelet
- Print parent and patient information sheets from
ASCIA
- All children with anaphylaxis should be referred to a paedatrician or
paediatric allergy specialist. Review is ideal as soon as possible after the episode
- Ensure that asthma control is addressed including diagnosis, action plan, and preventers, as asthma is an independent risk factor for fatal anaphylaxis (see
Asthma)
Peripheral IV adrenaline infusion
This should only be done in consultation with a senior staff member. Avoid high infusion rates for more than two hours as it may cause fluid overload
Check local health service adrenaline infusion guidelines. Below is an example guideline:
- Mix 1 mL of 1:1000 adrenaline in 1000 mL of fluid
- Suitable fluids are glucose 5%, glucose 10%, sodium chloride 0.9% saline and glucose with sodium chloride combinations
- Start infusion at 0.1 microgram/kg/minute (6 mL/kg/hr)
- A dedicated line, infusion pump and anti-reflux valves should be used when possible
- Titrate dose according to response and side-effects
- Monitor continuously (all vitals, 12-lead ECG and conscious state)
- If possible, insert a second IV as fluid boluses may be needed
- If hypotensive, resuscitate with fluid; use boluses of 20 mL/kg of sodium chloride 0.9% for shock
- Nebulised adrenaline is not recommended as first-line therapy, but may be a useful adjunct after IM adrenaline if upper airway obstruction or bronchospasm is present
- If airway oedema is not responding to parenteral (IM, IV) and nebulised adrenaline, early intubation is indicated
Consider consultation with local paediatric team when
- High risk of fatal anaphylaxis
- More than one dose of adrenaline required
- First diagnosis of anaphylaxis
- Anaphylaxis
to monoclonal antibody
Consider transfer when
- Inadequate adrenaline response
- Multiple doses of adrenaline
- Adrenaline infusion
- Immediate life-threatening situation
- A child requiring care beyond the comfort level of the hospital
NB: Also consider consultation with paediatric allergy/immunology team
Consider discharge when
See
Observation and Admission section above
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Parent information sheets
Allergic and anaphylactic reactions
Autoinjectors (epipen) for anaphylaxis – an overview
Allergyfacts.org.au
www.allergy.org.au
Additional notes
In Victoria it is a requirement to
notify all cases of anaphylaxis presenting to hospital, to the Department of Health and Human Services (this does not include cases arising in hospital)
Where the suspected cause is the consumption of a packaged food, notifications are required to be made immediately (within 24 hours of diagnosis) by telephone (1300 651 160, which is staffed 24 hours a day, seven days a week)
Where the suspected cause is anything other than packaged food, notifications are required to be made within five days of initial diagnosis of anaphylaxis and electronically via the
online form through the department's website
Last updated January 2021