See also
Emergency drug and fluid calculator
Resuscitation
Key Points
- Aim to identify reversible cause and manage accordingly.
- Seizures lasting more than 5 minutes should be treated.
- EEG should not be routinely performed after a first afebrile seizure.
- Ensure parental education regarding safety and future seizures.
Background
Unprovoked seizures are common in children with around 8% having a seizure by 15 years of age. Most seizures are brief and self-limiting, generally ceasing within 5 minutes.
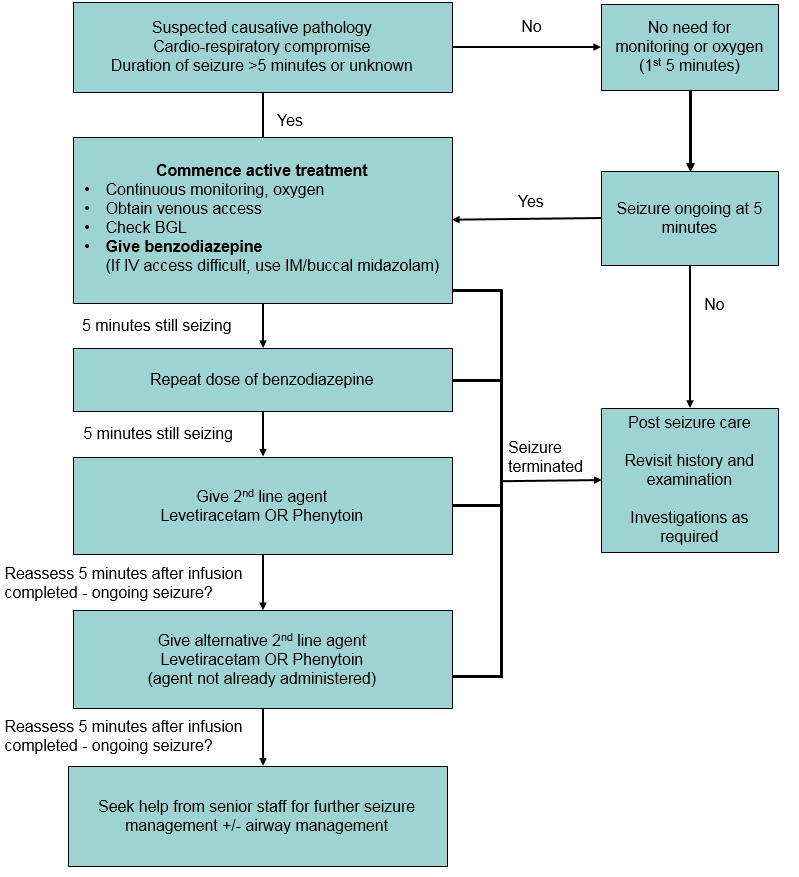
Seizures should be treated immediately in the following situations (see flowchart below):
- child actively seizing with duration unknown, or seizure for >5 minutes
- known pathology
- meningitis
- hypoxic injury
- trauma
- cardio-respiratory compromise
Assessment
Assessment and management should occur concurrently if the child is actively seizing.
Key
considerations in acute assessment
- Duration of seizure including pre-hospital period
- Past history: previous seizures and anti-seizure medication (management plan if in place), neurological comorbidity (eg VP shunt, structural brain abnormality) renal failure (hypertensive encephalopathy), endocrinopathy (electrolyte disturbance)
- Focal features
- Evidence of underlying cause that may require additional specific emergency management. Underlying causes include:
- hypoglycaemia
- electrolyte disturbances
- meningitis
- drug/toxin overdose
- trauma
- stroke and intracranial haemorrhage
- Age: treatable cause is more likely in children
<6 months
History
Detailed chronological history of events and behaviours before, during and after the seizure
History should be taken from the child if possible and obtain bystander account
Ask about:
- aura, focal features
- level of awareness
- recent trauma, consider non-accidental injury
- focality of limb or eye movement
- post-ictal phase/hemiparesis
Relevant
past history
- Family history of seizures or cardiac disorders/sudden death
- History suggestive of absence seizures or myoclonic jerks, nocturnal events
- Developmental history
Examination
- Full neurological examination looking for any abnormal neurological findings, signs of meningitis or raised intracranial pressure
- Cardiovascular examination including BP and look for any signs that suggest an underlying cause eg neurocutaneous stigmata, microcephaly
Red Flags
- Head injury with delayed seizure
- Developmental delay or regression
- Headache prior to the seizure
- Bleeding disorder, anticoagulation therapy
- Drug/alcohol use
- Focal signs
Differential diagnosis of seizure
- Arrhythmia
- Breath holding spell (episode occurs when the child is crying)
- Vasovagal syncope with anoxic seizure (postural change, preceded by dizziness and nausea)
- Non-epileptic paroxysmal disorder
Management
Initial
support
In most situations, observation for 5 minutes is appropriate whilst waiting for seizure to stop spontaneously
Treat the child the way the parents will at home – keep safe and observe
At this stage there is no need to check oximetry or apply oxygen
Active seizure flowchart
- Account for benzodiazepine doses given pre-hospital (eg by parents or paramedics)
- If available, refer to patient specific seizure management plan in children with a known seizure disorder
- Do not give a medication if the child
is allergic, has previously been unresponsive, or if he/she already taking it
Active seizure flowchart
Medications
used in acute seizures
| Medication |
Dose |
Comments |
| 1st
line |
| Midazolam |
0.15 mg/kg IV/IM (max 10 mg)
0.3 mg/kg buccal/IN (max 10 mg) |
|
| Diazepam |
0.3 mg/kg IV/IO (max 10 mg)
|
IV dose preferable. Do not give IM |
| 2nd
line |
| Phenytoin |
Loading dose:
20 mg/kg IV/IO
|
Infuse undiluted into a large vein over 20 min (max rate 50 mg/min) in a monitored patient
Do not give in age
<1 month |
| Levetiracetam |
40 mg/kg IV/IO (max 3g) |
Dilute to 50 mg/mL and infuse over 5 mins |
| Phenobarbitone |
20 mg/kg IV/IO (Max 1g) |
Dilute to 20 mg/mL or weaker and infuse over 20 mins (max rate 30 mg/min) in a monitored patient.
Stop infusion when seizure ceases
Commonly used in
neonatal seizures |
| 3rd line |
| Propofol |
2.5 mg/kg IV/IO stat followed by infusion at 1-3 mg/kg/hr |
For refractory seizures requiring rapid sequence induction and ventilation. Use only with involvement of senior staff confident with airway management. Beware hypotension. |
| Thiopentone |
2-5 mg/kg IV/IO slowly stat followed by infusion at 1-4 mg/kg/hr |
| Midazolam infusion |
1 mcg/kg/min |
|
| Ketamine |
1-2 mg/kg |
|
| Pyridoxine |
100 mg IV |
Consider in children up to 6 months with seizures refractory to standard anticonvulsants |
Post seizure care
Position child in recovery position, maintain airway
Monitor for further seizure activity
Consider investigations as appropriate
Investigations
Bloods
Blood glucose should be performed as soon as possible
Consider electrolytes, calcium and venous gas in the following circumstances:
- any seizure needing a second line agent
- children
<6 months
- medical comorbidity such as metabolic disorder, diabetes, dehydration
- child has not returned to baseline once the post-ictal phase and the effect of any medication has passed
Imaging
Consider in the following circumstances:
- focal seizure
- patients requiring 3rd line agent
- children
<6 months
- signs of elevated ICP
- bleeding disorder/anticoagulation
- child has not returned to baseline once the post-ictal phase and the effect of any medication has passed
EEG
- rarely required in the acute setting
- not indicated as a routine test following all first seizures
- benign focal epilepsy of childhood (BFEC) (also known as benign childhood epilepsy with centrotemporal spikes or benign rolandic epilepsy) and idiopathic generalised epilepsy (IGE) are the most common causes of afebrile seizures in children. Diagnosis of either cannot be confirmed
without EEG. BFEC and IGE may not require treatment, so EEG confirmation is usually not urgent. An EEG should generally be performed if a child has a second seizure. A positive diagnosis can avoid the need for neuroimaging
Consider consultation with local paediatric
team when
- Children
<6 months
- Prolonged seizures
- Incomplete recovery
- Focal seizures or post-ictal findings
- Recurrent seizures without a diagnosis of epilepsy
- Frequent/uncontrolled seizures in a child with known epilepsy
- Developmental delay
- Existing comorbidities
Consider admission for observation in children
<6 months
Consider transfer to
tertiary centre when
Children anticipated to require ICU level care (cardiorespiratory compromise).
For emergency advice
and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
In older children, when the child is back to baseline function with no red flags on history, examination or presumed cause
All families should receive education prior to discharge which includes:
- explanation of risk of recurrence
- seizure first aid and management plan
- advise parents to video events if safe to do so and keep a record
- provide written information
- consider need for emergency medication (buccal midazolam)
Follow-up after a first afebrile seizure
- All children who have a first afebrile seizure should have medical follow up
- EEG should not be routinely performed after a first afebrile seizure
Parent information sheet
Kids
Health Info (Vic)
Seizures – safety issues and how to help
Epilepsy
Midazolam for seizures
Electroencephalography
PENNSW First seizure pack and video
Last updated August 2020