These clinical practice guidelines provide advice to assist decision-making in clinical situations when child abuse and neglect are considered. They do not serve to replace health services' procedural guidelines or restrict discretion and good judgement in complex situations.
Clinical Practice Guidelines for child abuse and neglect, vulnerable children and "at risk children" are considered within 4 categories, recognising that differing forms of child abuse often co-exist.
- Physical harm / Non-accidental injury
- Sexual harm / Sexual abuse
- Neglect
- Vulnerable child / at risk of abuse
Medical practitioners are encouraged to seek advice from the Victorian Forensic Paediatric Medical Service (VFPMS), senior medical staff and to always operate within jurisdictional legislative requirements.
Children who attend with an injury that might have been inflicted need a full assessment of their physical condition and psychosocial situation.
The priorities in dealing with child physical abuse are to:
- suspect physical harm / non-accidental injury
- diagnose, treat and document the child's injuries
- interpret a pattern of injury or findings leading to the suspicion of abuse
- notify and involve the Victorian Forensic Paediatric Medical Service (VFPMS)
- assess the child's psychosocial situation
- provide, when consent is given or legislation requires information sharing in the absence of guardian's consent , a verbal and/or written report to Child Protection and the Police. VFPMS may be responsible for this task
- plan for the child's safe discharge and ongoing medical /psychological care.
|
Victorian Forensic Paediatric Medical Service
(24 hours 7 days a week)
|
1300 66 11 42
|
Assessment of a child's psychosocial situation may be conducted as a multidisciplinary assessment by professionals within the health service, including social workers and mental health professionals, working in partnership with Child Protection, police and community-based professionals.
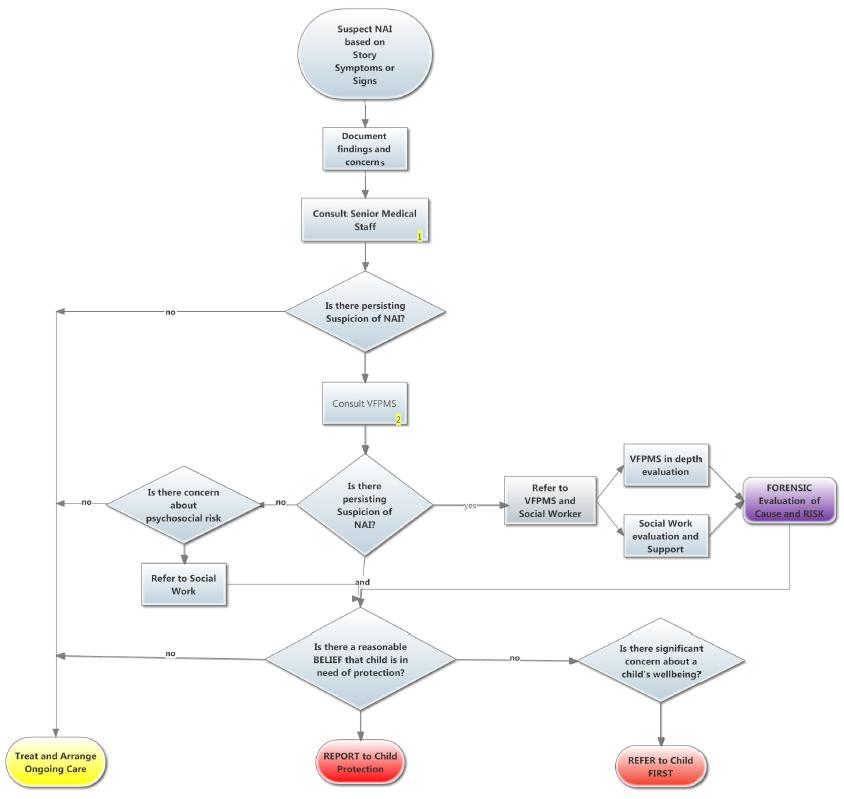
Admission to hospital should be arranged when it is medically necessary (head injury, fractures, failure to thrive etc) or when it is necessary for the child's safety.
A low threshold for admission is appropriate when dealing with an injured child.
Consider NAI in any infant who presents with an unexplained encephalopathy. Any infant with a cerebral injury, from shaking or direct trauma, should be admitted to ICU for monitoring overnight. Delayed deterioration may occur. (At RCH - ICU admission should only be declined following assessment by the ICU consultant).
The safe discharge of the child is the responsibility both of the hospital and Child Protection.
SCAN (Suspected Child Abuse and Neglect) multi-disciplinary professionals' meetings
All admitted patients should be the subject of a SCAN meeting held within 24 hours of admission.
The SCAN protocol is designed to help coordinate early discussions with Paediatric medical staff, Victorian Forensic Paediatric Medical Service, Child Protection and police.
See
SCAN meeting resources.
|
First line investigation of bruising
-
FBE
-
APPT
-
PT
-
Fibrinogen
-
Calcium
-
LFT (proteins)
-
U&E, Creatinine
Extended clotting profile
-
Factor VIII, IX, XI, XIII
-
Von Willebrand’s screen (and blood group)
-
Platelet function tests
-
+/- Lupus anticoagulant (+/-additional tests for lupus)
-
+/- Inflammatory markers (if vasculitis suspected)
|
Forensic investigation of suspected intra-abdominal trauma
- Amylase and lipase
- LFT
- FBE
- Fibrinogen
- Dipstick urine (blood)
- Ultrasound
- CT abdomen if significant concerns about paralytic ileus, intra-abdominal haemorrhage and elevated amylase (> 3 hours post trauma)
- Consider radiological imaging (MRI and/or CT brain scan) of the brains of infants and young children who might have been shaken.
- Consider MRI cervical spine
- Investigate as for fracture
- Consult with an ophthalmologist (and arrange for examination by the ophthalmologist)
- Investigate as for bruising when intracranial haemorrhage exists
- Urine Metabolic screen
- Admission to ICU should be considered whenever altered conscious state has occurred after suspected shaking because of the high risk of further neurological deterioration caused by progressive brain swelling
Forensic investigation of suspicious fractures
Radiological
investigation
Infants
and Toddlers aged < 2 years
The optimal method for radiological investigation of occult fracture has not been determined for children aged less than two years. Protocols vary between regions.
The following guidelines have been developed mindful of the need to minimise a child’s exposure to radiation (ALARA principle) balanced with the need to adequately investigate concerns regarding occult fracture in the context of suspected child abuse.
As a general principle, order investigations only when a positive result might result in intervention that increases a child’s safety or might result in additional action of some sort.
As a general guide we recommend the combination of Skeletal Survey and Bone Scan for children aged less than two years when there is a reasonable suspicion that the child has suffered an occult fracture.
Recommendation: < 2
years old – Skeletal Survey and Bone Scan
Exceptions
However, if one of the following fractures is detected as the only injurythen additional radiological investigation is not necessary.
- Distal radius/ulna fracture in a toddler aged > 9 months AND a history of a fall
- Distal tibia/fibula fracture in a toddler aged > 11 months AND fall while walking. “Toddler fracture”
- Single linear skull fracture in a child aged > 12 months AND a history of a fall or adult landing on child
- Clavicle fracture in the newborn
- Clavicle fracture in 2nd year of life AND a history of a fall
In regions where Bone Scan is not available or when parents refuse consent for Bone Scan then a second Skeletal Survey performed 2 weeks after the first Skeletal Survey may be considered. Note that this process is likely to miss some occult fractures (particularly rib fractures in
infants). Strategies will need to be put in place to ensure safe care for the infant between Skeletal Surveys and safe plans to ensure that the second Skeletal Survey is performed and the infant is not lost to follow up.
“Double reporting” of Skeletal Surveys (reporting by two independent radiologists) is encouraged.
Children
aged > 2 years
Most children aged > 2 years will develop symptoms and signs of injury when a fracture is present. We recommend X-rays of the site(s) of suspected fracture with coned views if required.
Recommendation: > 2 years : Radiograph (x-ray)
sites of clinically suspected fracture(s).
However, Skeletal Survey might be indicated because of a strong suspicion of occult fracture in a child aged > 2 years. Bone Scan might be considered as an adjunct to Skeletal Survey under such circumstances.
Occasionally MRI or ultrasound might also be considered.
Notes
- Skeletal Surveys must be performed according to recommended protocols.
- X-rays might fail to detect rib fractures and some long bone fractures.
- Bone Scan is not a sensitive tool for the detection of skull fractures. If skull fracture is suspected, obtain a skull radiograph or CT scan. Note that the dose of irradiation must be weighed against the need to determine whether a skull fracture exists.
- Bone Scan might not detect CML.
- Bone Scan is unlikely to detect most fractures that occurred > 12 months previously.
Blood tests to
investigate suspicious fracture
First line tests:
- Calcium
- Phosphate
- LFT
- U&E Creatinine
- Vit D
- FBE
Second line tests:
- Magnesium
- Copper
- Parathyroid hormone
- Syphilis serology
- Urine Metabolic Screen
- Inflammatory markers
Also consider genetic tests for OI.
If suspicions exist about intentional thermal injury such as scalds and contact burns in children aged
< 3 years, then skeletal survey, bone scan and additional investigations for other forms of child abuse should be considered.
Toxicology tests might be considered when ingestion or poisoning is possible as a result of care-giver neglect or intentional exposure/ ingestion. Also consider toxicology tests in children with unexplained altered conscious state, head injury, thermal injury and sexual assault.
- Consult with forensic experts before collecting samples.
- Ensure chain of evidence procedures if sending samples to forensic laboratory
- Collect blood and urine if ingestion or poisoning was within prior 24 hours
- Collect urine if ingestion or poisoning was more than 24 hours previously
- Consult with VFPMS if considering sampling hair for toxicological analysis.
Forensic toxicology laboratories and hospital biochemistry laboratories differ significantly in the analytical techniques used for drug detection and in the way that results are reported. Send samples to the laboratory that can perform the required tests.
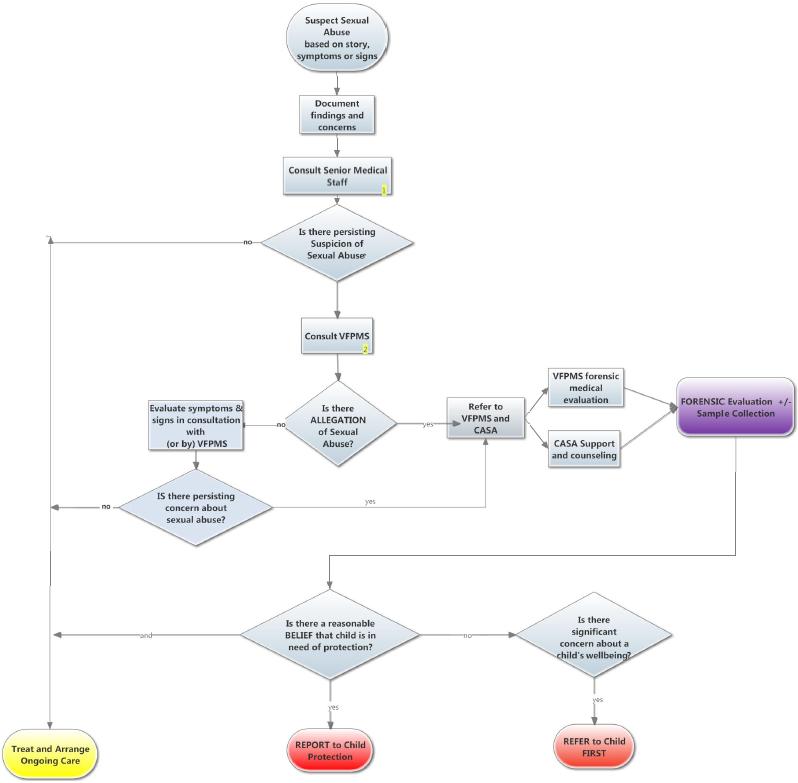
All children about whom there are suspicions of sexual abuse should be discussed with the
VFPMS in the first instance. This will facilitate exclusion of the diagnosis of sexual assault in children who have not been sexually assaulted but who have conditions such as genital symptoms that are sometimes confused with sexual assault. This will reduce angst and suffering in children and their caregivers when there is an unreasonable suspicion of sexual assault.
In general, genital examinations for forensic purposes will only be performed by appropriately trained and experienced consultants.
The priorities in dealing with child sexual abuse are to:
- suspect sexual harm
- consult with the Victorian Forensic Paediatric Medical Service (VFPMS) to determine the best person, place and time for forensic evaluation.
- when a child has made an allegation of sexual assault, notify and involve local Centre Against Sexual Assault (CASA) counsellor
- diagnose, treat and document the child's injuries
- assess the child's psychosocial situation,
- provide, when consent is given or legislation requires information sharing in the absence of guardian's consent, a verbal and/or written report to Child Protection and the Police. VFPMS is usually responsible for this.
- plan for the child's safe discharge and ongoing medical / psychological care.
After consultation with the VFPMS, when an urgent forensic examination by VFPMS is deemed to be unnecessary, limited inspection for a specific purpose such as determination of the amount of bleeding or the extent of a rash or discharge may be performed with the cooperation of the child.
After a recent sexual assault (
< 72 hours) rapid evaluation is required. Contact the VFPMS, and speak to the consultant on-call. Collection of forensic evidence is an important consideration. You may be advised to assess and treat any urgent medical problems (eg. bleeding), being careful to collect any clothing that is removed in the process. Ensure the child is as comfortable as possible and has appropriate emotional support. Await the on-call VFPMS consultant who will perform the forensic examination as a joint response with the CASA counsellor.
STI prophylaxis : Azithromycin 1 g stat
Pregnancy prophylaxis: Postinor (post coital contraception) within 72 h of sexual contact. Arrange for a follow-up pregnancy test
HIV prophylaxis: NPEP (according to ASHM post exposure prophylaxis guidelines)
Post sexual assault sexually transmissible infection screen
|
At time of examination (optional)
- First pass urine
- Gonorrhea and Chlamydia PCR
|
|
Baseline tests (2weeks post assault)
- First pass urine (unless test performed when child examined and results negative)
- Gonorrhea and Chlamydia PCR
- Blood serology for:
|
|
At 3 months blood serology
|
|
At 6 months blood serology
|
The priorities in dealing with a vulnerable child are to:
- suspect and identify vulnerability
- assess the child's psychosocial situation
- conduct a multi-disciplinary assessment of vulnerabilities and protective factors using an ecological framework that focusses on the child, their caregivers, family, community, support systems and agencies that might better support children and their caregivers
- refer to services to modify risk and promote resilience / protection.
- Plan ongoing monitoring of the child's safety, wellbeing and vulnerability to harm
After a multi-disciplinary assessment, when significant concerns exist about a child's wellbeing, referral to Child FIRST should occur.
All medical staff working in the Emergency Department & Wards must be aware of the possibility of child abuse, and be able and prepared to act appropriately if it is suspected.
Medical and Nursing staff are mandated reporters who must notify Child Protection after forming a belief, on reasonable grounds, that a child has been, or is likely to be, physically or sexually abused and the parents have not protected, or are unlikely to protect, the child from such harm. There is an obligation upon all hospital staff to notify Child Protection if they have formed a belief that a child is in need of protection. See Children, Youth and Families Act 2005 - SECT 162
For Victorian Health Professionals:
The Victorian Forensic Paediatric Medical Service is available 24/7 for forensic medical advice and consultation.
As well as regular clinics each Monday to Friday, the VFPMS provides a 24 hour service for evaluation of possible causes of injury and advice for professionals regarding evaluation of suspected child abuse. They can also advise on good medical report writing, provide peer review of medico-legal reports and can liaise with the external agencies.
|
Victorian Forensic Paediatric Medical Service
(24 hours 7 days a week)
|
1300 66 11 42
|
In Melbourne
The Victorian Forensic Paediatric Medical Service is situated at RCH and MMC
- At RCH - at Clinic C on the 1st floor of the East building at RCH (9345 4299)
- At MMC - opposite radiology on the ground floor at MMC, Clayton (9594 2155).
Refer to Department of Social Work for psychosocial assessment when there are concerns about risk of harm to a child.
- At Royal Children's Hospital contact
Social Work Department 9345 6111 and after hours via RCH switchboard 93455522
- At Monash Children's Hospital contact
Social Work Department 95942290 and after hours via MMC switchboard 95946666
Refer children and their family members for counselling to a Centre Against Sexual Assault when an allegation of sexual abuse has been made.
- At Royal Children's Hospital contact
Gatehouse 93456391 and after hours via RCH switchboard 93455522
- At Monash Children's Hospital contact
SECASA 03 9594 2289 and after hours via MMC switchboard 95946666 or Sexual Assault Crisis Line (SACL) 1800 806 292 (Freecall Victoria).