Table of contents will be automatically generated here...
Introduction
Significant chest injury is
rare in paediatric trauma. Most cases
occur secondary to blunt chest trauma, with penetrating injuries accounting for
less than 10% or the total reported incidence worldwide.
Over a 5 year period to 2007
there were 204 cases of severe paediatric thoracic trauma in Victoria1. The most common injuries identified were
lung contusion (65%) and haemo/pneumothorax (37%). Blunt trauma accounted for 96% of injuries
and 75% were secondary to motor vehicle accidents (including pedestrian vs motor vehicle). Due to this frequent association
with motor vehicle accidents (MVAs) patients with chest trauma usually have concomitant injuries to other
major systems, most commonly the head and abdomen. In the above study 99% of patients had an
injury to one of more other body regions.
This underscores the high level of force involved in most paediatric
chest trauma.
Mortality
Mortality in children with
chest trauma has been quoted to be as high as 30% although death is not always
related directly to the chest injury. Death usually occurs soon
after the injury in a child, whereas an adult with comparable injuries tends to
survive longer.
How children are different
- A major difference between adults and children is the compliance of the chest wall, due to the greater elasticity of the ribs. This allows greater deformation of the chest wall before the ribs fracture. Thus major internal injuries may occur without any
external chest wall injury.
- Children have a greater cardiopulmonary reserve, and so compensatory mechanisms may mask hypovolaemia and respiratory distress.
- A drop in blood pressure in the paediatric population is a very late sign, signifying imminent death.
- The mobility of the mediastinum decreases the risk of major airway and vessel injury. However, ventilatory and cardiovascular compromise may occur rapidly, due to the mediastinal shift.
- A common response to injury in children is aerophagia, which is often associated with a reflex ileus. This can lead to acute gastric dilatation, which may further compromise respiratory function.
- There should be a high index in paediatric trauma for orogastric / nasogastric placement, with orogastric only indicated where head injury is a concern.
In all aspects of trauma
management, the primary survey is first
priority
Primary survey
The purpose of the primary
survey is to identify and manage life threats. The particular thoracic
injuries that are necessary to identify during the primary survey include:
-
Tension
pneumothorax
- Open
pneumothorax
- Massive
haemothorax
- Flail
chest
- Cardiac
tamponade
In these injuries frequent
reassessment of ABC is a necessary part of their assessment & management
Types of injuries
Tension Pneumothorax
- Accumulation
of air in the pleural space under pressure resulting in compression of the
ipsilateral lung
- Progressive
air accumulation causes mediastinal shift and development of compression to the
contralateral lung
- Impaired
venous return
- Compromised
cardiac output
Diagnosis
- Hypoxia
- Severe
respiratory distress
- Altered
level of consciousness
- Shift in
mediastinum or trachea to the contralateral side
- Distended
neck veins
- Absent
or decreased breath sounds bilaterally
- Hyper-resonance
to percussion
- Impaired
venous return to the heart
- Patient
will be tachycardic with peripheral vasoconstriction and in hypotensive shock
Treatment
(see also Management of Traumatic Pneumothorax and Haemothorax)
- High
flow oxygen
- Analgesia
- Immediate finger thoracostomy is the preferred management in the in-hospital environement. This is done in the 4th or 5th intercostal space, between the anterior and mid-axillary line, on the side of the pneumothorax, followed immediately by an intercostal catheter in the same location (Figure 1).
- If unable to do an immediate finger thoracostomy, an immediate needle thoracocentesis – midclavicular line, 2nd intercostal space,
on the side of the pneumothorax (Figure 2 & 3). This should be followed as soon as possible by a finger thoracostomy and intercostal catheter insertion – 4th or 5th
intercostal space anterior axillary line
Figure 1 - surface marking for left sided finger thoracostomy and intercostal catheter insertion
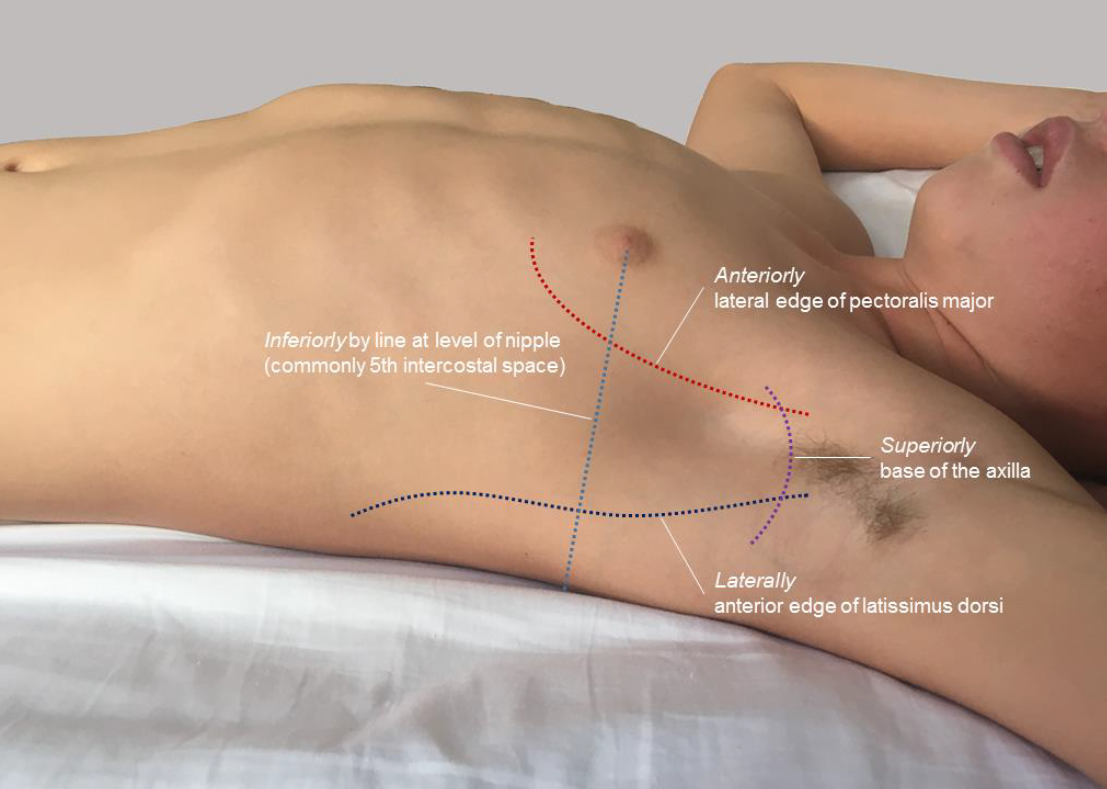
Figure 2 – surface marking for needle
thoracocentesis

Figure 3 – needle thoracocentesis insertion

There is a 10-20% chance of causing a
pneumothorax if thoracocentesis is attempted in the absence of a pre-existing
pneumothorax. This procedure must be
followed up by a chest x-ray and insertion of an intercostal catheter.
Open Pneumothorax
- This
injury occurs secondary to penetrating wounds of the chest. It occurs where the wound is greater than two thirds the diameter of the trachea. At this size and above, the negative pressure generated through excursion of the chest in inspiration, will lead to the preferential influx of air via the wound into the pleural space, rather than via the upper airway. If air fails to escape with expiration, a tension pneumothorax will develop.
Diagnosis
- Respiratory
distress
- Hypoxia
- Decreased
chest movement
- Decreased
air entry
- Hyper-resonant
to percussion
- Chest
wound through which air may be heard passing with inspiration & expiration
Treatment
- High
flow oxygen
- Analgesia
- In hospital, cover
with occlusive dressing (small wounds) or suture/staple the wound closed (larger wounds)
- Immediate
insertion of intercostal catheter
- The use of a 3 sided occlusive dressing - to act as a one way valve - is no longer recommended as treatment for an open pneumothorax once the patient has arrived in hospital. If may be applied when the patient is being managed in the pre-hsopital environment and there will be a delay to insertion of an intercostal catheter. However, they can be hard to apply to a bleeding wound, and they have variable efficacy.
Figure 4 - A 3 sided occlusive dressing

Massive
Haemothorax
- This is
a rare injury in the paediatric population
- Rapid,
large volume accumulation of blood in the pleural space
- May
result secondary to a blunt or penetrating injury – cardiac or great vessel
injury
- Potential
to lose up to 40% of blood volume in each hemithorax
Diagnosis
- Respiratory
distress
- Decreased
chest movement
- Decreased
air entry
- Dullness
to percussion
Treatment
- High
flow oxygen
- Analgesia
- Ventilatory
support
- Rapid
fluid resuscitation
- Insertion
of intercostal catheter – 4th or 5th intercostal space,
anterior axillary line (Figure 1)
- Urgent
surgical review for possible thoracotomy if ongoing haemorrhage with inability
to stabilise circulation despite aggressive fluid resuscitation
Flail Chest
- This occurs secondary
to blunt injury - it is less common in children than in adults due to the greater elastic properties of the paediatric ribcage - which permits far greater plastic deformation on impact without resultant broken ribs. However, the underlying lung parenchyma is susceptible to contusion
- A flail chest is the
result of 2 or more fractures in two or more adjacent ribs interrupting the
bony continuity of the thoracic wall (Figure 5)
Figure 5 – Flail chest with pulmonary
contusions
Diagnosis
- “Paradoxical
movement” – the flail segment is seen to collapse with inspiration and bulge
with expiration while the rest of the chest wall moves in the opposite way
- Respiratory
distress
- Possible
decreased air entry due to associated pulmonary contusion and splinting
- Possible
subcutaneous emphysema
Treatment
- Aggressive
analgesia
- High
flow oxygen with ventilatory support as necessary
- Stabilisation
of flail segment. Patient may be placed
injured side down
- Positive pressure ventilation improve ventilation, and intubation may be necessary to help with analgesic demands.
- Referral to cardiothoracic surgeons for consideration of rib fixation
Cardiac Tamponade
- Bleeding
into the pericardium secondary to blunt or penetrating injury
- Blood
may originate from cardiac chamber, a great vessel or from the myocardium in
the presence of a myocardial contusion
- Results
in decreased filling of the heart and thus reduced stroke volume and shock
Diagnosis
- Respiratory
distress
- Hypotension
- Narrow
pulse pressure
- Distended
neck veins
- Soft
heart sounds
- Refractory
shock
Investigations
- Bedside
USS for confirmation if time permits
Treatment
- ECG
monitoring
- High
flow oxygen
- Fluid
resuscitation (to increase preload and minimise right ventricular collapse)
- The optimum treatment for a pericardial tamponade secondary to blunt or penetrating trauma is open surgical drainage in theatre.
- In the situation where there is severe shock and no surgical facilities available, needle pericardiocentesis can be performed as a temporising measure.
- A long needle is inserted at a left sub-xiphoid position, and directed posteriorly at a 45° angle and towards the left shoulder - this is better performed under ultrasound guidance where skills and equipment permit.
There is limited evidence for the role of an ED thoracotomy in the paediatric population who have sustained a blunt injury, it should be considered in the event of penetrating trauma
Pulmonary Contusion
- The most
common thoracic injury in children
- Often
associated with other injuries such as fractures and haemothorax
- May
occur in absence of obvious chest wall injury
- Haemorrhage
and oedema within affected lung segment
Diagnosis
- Hypoxia
– degree of compromise will depend on size of contusion
- Respiratory
distress – may very in severity
- Decreased
air entry on ipsilateral side
Investigations
- Chest
x-ray – patchy consolidation, may be bilateral (Figure 5) - may initially be unremarkable with changes
evolving over 24-72 hours
Treatment
- High
flow oxygen
- Analgesia
- Pulmonary
toilet including regular suction and chest physiotherapy
- Ventilatory
support
- Contusions
may evolve clinically & radiologically over first 24-72 hours
Rib Fractures
- The
paediatric chest wall can sustain more deformation before rib fractures occur
compared with the adult chest wall
- Despite
this rib fractures are still common in paediatric chest trauma
- Indicative
of significant injury and greater likelihood of comcommitant multisystem
injuries
- Almost always
associated with pulmonary contusions
Diagnosis
- Chest
wall bruising/abrasions
- Respiratory
distress
- Hypoventilation
secondary to splinting
- Decreased
chest expansion
- Hyper-resonance
or dullness to percussion (depending on associated pneumothorax or contusion)
- Normal
or decreased air entry
Investigations
- Chest
x-ray – fractures & consolidation may be evident - may be
unremarkable initially
Treatment
- High
flow oxygen
- Aggressive
analgesia
- Ventilator
support as necessary
- Inpatient
monitoring as deterioration may occur due to associated pulmonary contusions
Simple Pneumothorax
- Accumulation
of air in the pleural space
- Degree
of compromise related to the size of the pneumothorax and other associated
injuries
Diagnosis
- Respiratory
distress
- Pleuritic
chest pain
- Decreased
chest wall movement ipsilateral side
- Decreased
air entry
- Ipsilateral
hyper-resonance to percussion
- May be
asymptomatic
Investigations
- Chest
x-ray – collapse of lung parenchyma on ipsilateral side with slightly increased
expansion of chest wall
- Ultrasound
– absence of lung sliding and B-lines, presence of A-lines; presence of a lung point. This should be performed
by experienced clinician
Treatment:
- Supplemental
oxygen
- Analgesia
- Ventilatory
support as necessary
- If
patient has respiratory compromise or the pneumothorax is >20% on chest
x-ray insertion of intercostal chest catheter is required
- If the
patient does not meet above criteria and thus doesn’t require immediate chest
drain insertion, admission and intensive monitoring is required as a simple
pneumothorax may enlarge and become symptomatic or even convert to a tension
pneumothorax
Haemo-Pneumothorax
- A
combination of the accumulation of both blood and air in the pleural space
Diagnosis
- Respiratory
distress
- Decreased
chest wall movement
- Decreased
air entry
- Dullness
to percussion
Investigations
- Chest
x-ray – collapse of ipsilateral lung, pleural effusion with air/fluid level in
pleural space
Treatment
- High
flow oxygen
- Analgesia
- Ventilatory
support as necessary
- Fluid
resuscitation
- Insertion
of intercostal chest drain
Pulmonary Laceration
- Most
commonly secondary to penetrating injury but may occur with blunt trauma
- Typically
associated with pulmonary contusions and haemopneumothorax on the ipsilateral
side
Diagnosis
- Signs of
trauma to chest wall ie. Bruising/abrasions
- Respiratory
distress
- Hypoxia
- Decreased
chest expansion
- Dullness
to percussion
- Decreased
breath sounds
Investigations
- Chest
x-ray - collapse of ipsilateral lung, pleural effusion with air/fluid level in pleural
space
Treatment
- High
flow oxygen
- Analgesia
- Ventilatory
support as required
- May
require surgical intervention if persisiting air leak or bleeding
Traumatic Rupture of the
Aorta
- Very
rare injury in the paediatric population
- Typically
occurs in rapid deceleration injuries such as that sustained in high-speed
motor vehicle accidents
- Commonly
occurs at, or very close to, the ligamentum arteriosum which attaches to the
proximal descending aorta just beyond the left subclavian artery. The ascending aorta and aortic arch are much
more mobile compared with the descending aorta and it is probable that at the
time of impact a major torsional inury occurs at this junction
- In many
cases this injury will result in immediate massive blood loss into the left pleural
cavity and death occurs at the scene of the accident.
Diagnosis
- Respiratory
distress
- Decreased
air entry and dullness to percussion on the left
- Tachycardia
- Hypotension
If
suspected on plain radiography further investigation is required – CT chest,
aortogram or trans-oesophageal echocardiogram.
Investigations
- Chest
x-ray – suspect with any of the following features
- Widened
mediastinum on erect film
- Pleural
cap over the apex of the left lung (due to haemoatoma tracking upwards)
- Loss of
the aortic knuckle
- Deviation
of trachea or oesophagus to the right
- Depression
of left main stem bronchus
- If
diagnosis suspected on plain radiography further investigation required
- CT chest
- Aortogram
(Gold Standard)
- Trans-oesophageal
echocardiogram
Treatment
- Analgesia
- Fluid
resuscitation
- Supplemental
oxygen
- Ventilatory
support as needed
- If
diagnosis confirmed will require aortic surgery to resect the site of injury
with either aortic repair of replacement
Tracheo-Bronchial Injury
- Rare
injury
- Potentially
life threatening
- Almost
exclusively occurs due to penetrating injury
- Results
from trauma to region between larynx and segmental bronchus
Diagnosis
- Respiratory
distress
- Hypoxia
- Partial
airway obstruction
- Subcutaneous
emphysema
- Decreased
air entry
- Continuous
air leak after insertion of intercostal catheter
Investigations
- Chest
x-ray – pneumothorax (may be bilateral), pneumomediastinum, subcutaneous
emphysema
Treatment
- High
flow oxygen – adequate oxygenation may be difficult to achieve
- Analgesia
- ETT
placement beyond level of injury
- Ventilatory
support
- Referral
to thoracic surgeon for definitive management
Oesophageal Injury
- Rare
- Most
commonly due to penetrating injury but may occur following blunt injury to the upper
abdomen causing forceful ejection of stomach contents into the oesophagus
resulting in a linear tear in the lower oesophagus
Diagnosis
- Respiratory
distress
- Fever
may be present
- Subcutaneous
emphysema
- Peritonism
- guarding, rigdity
- Decreased
air entry
- Intercostal
catheter may drain gastric contents
Investigations
- Chest
x-ray – pneumomediastinum, pneumothorax, pleural effusion, subcutaneous
emphysema
Treatment
- Supplemental
oxygen
- Analgesia
- Insertion
of nasogastric tube
- Broad
spectrum antibiotic cover
- May be
managed conservatively or require insertion of intercostal chest drain
- Surgical
intervention may be required
Myocardial contusion
- Typically
occurs following direct blunt trauma to the sternum
- Most
often involves the anterior wall of the heart
- Should
be suspected in any patient with injury over the sternum, in particular if
there is a sternal fracture
Diagnosis
- Anterior
chest wall bruising/tenderness
- Tachycardia
- Tachypnoea
- Prolonged
capillary refill time
- Hypotension
- May have
arrhythmia
- May be
asymptomatic
- May be
complicated by cardiac tamponade
Investigations
- ECG –
monitor for changes similar to those of myocardial infarction or arrhythmias
- Cardiac
enzymes
- Echocardiogram
to detect impaired myocardial function (dyskinesis or akinesis)
Treatment
- Supplemental
oxygen
- Analgesia
- ECG
monitoring
- Serial
cardiac enzymes
- Follow
up echocardiogram
Diaphragmatic Rupture
- Rare
injury but well recognised
- Occurs
due to forceful blunt abdominal injury causing a sudden, major increase in
intra-abdominal pressure
- Usually
left sided
- May
result in abdominal viscera being displaced into thoracic cavity
Diagnosis
- Tachypnoea
- Possible
hypoxia
- Evidence
of abdominal trauma – contusion/abrasion
- Decreased
chest wall movement
- May have
decreased air entry on left with potential for bowel sounds in chest
- Mediastinal
shift may occur
Investigations
- CXR –
difficult to identify diaphragm, abdominal contents in hemithorax, tip of NGT
in chest (Figure 6 & 7)
- Contrast
study gives definitive diagnosis (Figure 8)
Figure 6 - diagphragmatic rupture, unable to visualise left diaphragm

Figure 7 - diagphragmatic injury, nasogastric tip visible in left hemithorax
Figure 8 - diaphragmatic injury, contrast within stomach visible in left hemithorax

Contrast study or CT will give definitive diagnosis.
Treatment
- High
flow oxygen
- Analgesia
- NGT
placement
- Surgical
referral
Traumatic Asphyxiation (“run
over” injury)
- Very
rare
- Caused
by severe, prolonged compression of the chest
- Results
in obstruction of venous return leading to extravasation of blood into tissues
Diagnosis
- Petechiae
of upper chest, neck, arms and face
- Bulging
eyes
- Subconjunctival
haemorrhages
- Massive
subcutaneous oedema
- Respiratory
distress
- Tachypnoea
- Hypoxia
- Decreased
chest movement
- Decreased
air entry
- Underlying
vascular injury – assess for pulses, bruits, haematomas, intracranial
haemorrhage
- Underlying
nerve injury – assess for motor and sensory deficits
Treatment
- High
flow oxygen
- Intubation
and ventilator support
- Analgesia
- Management
must be directed to underlying injuries
- Referral
to thoracic surgeon
IMAGING
Chest X-ray
- Good
screening tool
- Limited
in trauma assessment as images are taken with patient supine and therefore more
difficult to appreciate certain injuries ie. Pneumothorax, Hamothorax
- Consider
cross-table film to better assess for these injuries
- Useful
guide for selective CT imaging
- Normal
chest x-ray essentially excludes significant thoracic injury requiring
intervention2,3,4
CT Chest
- Not
routine in paediatric trauma
- Selective
use in cases with abnormal chest x-ray or high clinical suspicion
- Radiation
exposure is approximately 6x that of plain radiography and increases lifetime
risk of malignancy to 1/500 and risk of fatal malignancy up to 1/12002,3
- Injuries
picked up on chest CT with normal x-ray most commonly rib fractures or
pneumothorax, usually not of clinical significance and not requiring
intervention2,3,4.
- Therefore
radiation risk versus clinical benefit too high2,4
Chest Ultrasound
- Can be
useful in detection of pneumothorax and haemothorax that may not be evident on
supine chest x-ray4 .
- More
sensitive in diagnosing pneumothorax than plain chest x-ray in the hands of an
experienced clinician
- FAST and
EFAST not validated in the paediatric population
Resuscitative thoracotomy
- Resuscitative thoracotomy in the Emergency Department, in traumatic cardiac arrest, is controversial in
paediatrics. However it is an accepted procedure in adult trauma management.
- Given
the rarity of severe chest trauma in children the literature of resuscitative thoracotomy, in the paediatric population, is scarce
- Studies
investigating efficacy of emergency department thoracotomies in children have
demonstrated some success in older children, primarily teenagers, with
penetrating chest trauma who have detectable signs of life at the scene of
trauma5,6,7,8
- There
have only been 2 patients documented in the literature who have survived ED
thoracotomy following blunt chest trauma, these were in 1988 & 19896,7
- There
has been no survival documented in the literature of children under 9 years of
age who underwent emergency department thorocotomy6,7
- However
given that the alternative is death, most studies suggest that in selected cases
ie. older children who fit the above criteria (penetrating chest trauma with
signs of life at the scene) resuscitative thoracotomy be considered5,8 (This is reliant on sufficient training and expertise existing, as well as the ongoing capability to provide thoracic surgical expertise to the patient).
- A recent consensus based guideline developed by the PERUKI group has been developed9. This looked at traumatic paediatric cardiac arrest that was not due to hypoxia (e.g. drowning, asphyxiation or imapact apnoea), and recommended the provision of specific lifesaving interventions over the use of chest compressions and defibrillation. The lifesaving interventions recommended are:
- external haemorrhage control,
- adequate oxygenation and ventilation,
- bilateral thoracostomies,
- rapid volume replacement with warmed blood and blood products and,
- application of a pelvic binder
Summary
- A lack of external signs does not preclude
major underlying thoracic injury
- Chest injuries rarely occur in isolation,
usually being associated with injury to other systems, most commonly head or
abdomen
- Physiological differences of the paediatric
chest must be taken into consideration – especially during the primary and
secondary survey
- Treatment in the absence of major
cardiovascular or tracheobronchial injury will be guided by oxygenation. In many cases, the use of adequate analgesia
and supplemental oxygen may be all that is needed
- The insertion of intercostal catheters should
be considered in the following cases10
- Where there is an intrapleural collection
causing compromise
- Where there is a significant chest injury and
the patient is to be placed on positive pressure ventilation
- Where the patient is to be transported by air
ambulance
References
- Samarasekera
SP, Mikocka-Walus A, Butt W, Cameron P.
Epidemiology of major paediatric chest trauma. J of
Paediatrics and Child Health. 2009; 45: 676-680
- Holscher
CM, Faulk LW, Moore EE et al. Chest
computed tomography imaging for blunt pediatric trauma: not worth the radiation
risk. J of Surgical Research.
2013; 184: 352-357
- Yanchar
NL, Woo K, Brennan M, et al. Chest x-ray
as a screening tool for blunt thoracic trauma in children. J
Trauma Acute Care Surg. 2013; 75: 613-619
- Moore
MA, Wallace EC, Westra SJ. Chest Trauma
in Children: Current Imaging Guidelines
and Techniques. Radiol Clin N Am. 2011; 49: 949-968
- Easter
JS, Vinton DT, Haukoos JS. Emergent
pediatric thoracotomy following traumatic arrest. Resuscitation. 2012; 83:
1521-1524
- Allen CJ,
Valle EJ, Thorson CM, et al. Pediatric
emergency department thoracotomy: A
large case series and systematic review.
J of Pediatric Surgery. 2015; 50:
177-181
- Flynn-O’Brien
KT, Stewart BT, Fallat ME, et al.
Mortality after emergency department thoracotomy for pediatric blunt
trauma: Analysis of the National Trauma
Data Bank 2007-2012. J of Pediatric Surgery. 2016; 51:
163-167
- Moore
HB, Moore EE, Bensard DD. Pediatric
Emergency Department Thoracotomy: A
40-Year Review. J of Pediatric Surgery.
2016; 51: 315-318
- Vasallo, J., Nutbeam, T., Rickard, AC. et al. Paediatric traumatic cardiac arrest: the development of an algorithm to guide recognition, management and decisions to terminate resuscitation. Emer Med J. 2018; 35:669-674
- Strutt
J, Kharbanda A. Pediatric Chest Tubes
And Pigtails: An Evidence-Based Approach
To The Management Of Pleural Space Diseases.
Pediatric Emergency Medicine
Practice. 2015; 12: 1-24