Table of contents will be automatically generated here...
Face masks
Ideally, facemasks should be clear to allow you to see:
-
The child's colour, and
-
The possible presence of vomit.
-
Some masks conform to the anatomy of the child's face and make providing a good seal relatively easy. These masks also have a relatively low dead space.
-
Circular soft plastic masks also give an excellent seal and are available across a range of sizes - from those designed to fit small neonates through to masks for large adults. Try to store a wide variety of sizes.
-
The correct size mask is one which fits over the mouth and nose but does not press on the eyes.
A guide to sizes of Laerdel silicone face masks 00 and 0/1 - Neonate - infant 2 - infant - small children 3 - small - large children 4 - Adult 5 - Large adult:

Jaw thrust
Jaw thrust manoeuvre:

-
Jaw thrust is achieved by placing two or three fingers under the angle of the mandible bilaterally, and lifting the jaw upwards, ensuring the maintenance of in-line immobilisation.
-
Jaw thrust acts to lift the tongue off the back of the pharynx and so clear the airway.
-
This technique may be easier if the rescuer's elbows are resting on the bed or surface the child is lying on.
Oropharyngeal Airway Insertion (OPA)
-
An OPA is indicated if the jaw thrust manoeuvre has failed to correct airway obstruction.
-
An OPA acts by establishing an opening between the tongue and the posterior pharyngeal wall and can make a difficult airway much easier to manage.
-
OPAs may not be tolerated by semi-conscious patients
Guedel airways:

Equipment required
-
Lubrication
-
Tongue depressor
-
Appropriate sized OPA
Sizing
Oropharyngeal airway sizing:

-
Measure from the centre of the incisors to the angle of the mandible, when laid on the face concave side up.
Procedure
-
Pre-lubricate with either the patient's own saliva or a small amount of lubricating jelly.
-
Insertion: >8 years: like an adult: concave side up; pass to the back of the hard palate, then rotate 180o to concave side down
- <8 years: insert under direct vision, concave side down, using a tongue depressor
Outcome:
-
Correction of obstruction
-
Improved ventilation
-
If ventilation is still insufficient, the patient may require more advanced airway procedures, such as intubation
Endotracheal tube intubation
Indications
Failure to obtain an airway by simple airway opening maneuvers (eg: OPA insertion)
Airway protection (eg: from blood, broken teeth, vomitus)
To provide a secure airway for transport
To control ventilation in the unconscious/head injured patient
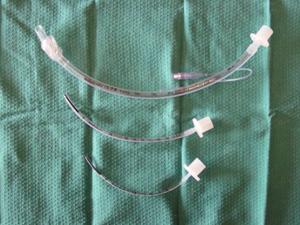
Endotracheal tubes
-
Uncuffed tubes are preferable in children up to eight years of age, to avoid oedema at the cricoid ring.
-
Finding the right-sized tube is important, to avoid large leaks around the tube.
-
Nasotracheal intubation whilst more secure is contra-indicated in patients with possible base of skull fracture
Sizing:
Diameter Neonate - 3.0 mm 0-6 months -3.5mm 6-12 months -4.0 mm Then use (Age in years / 4) + 4 = size of endotracheal tube (ET) mm
Length of insertion at lips:
Visualise the tube passing through vocal cords avoiding endobronchial intubation:
Endotracheal tubes:
|
Newborn
|
|
|
10 cm
|
|
1 yr
|
|
|
11cm
|
|
2 yr
|
|
|
12 cm
|
|
3 yr
|
|
|
13 cm
|
|
4 yr
|
|
|
14 cm
|
|
6 yr
|
|
|
15 cm
|
|
8 yr
|
|
|
16 cm
|
|
10 yr
|
|
|
17 cm<
|
|
12 yr
|
|
|
18 cm
|
Formula for length (at lips) of oral tube is Age/2 + 12
Laryngoscope:
Curved or straight blades can be used although the straight blade laryngoscope is recommended in young children, because:
-
It is designed to lift the epiglottis, which is comparitavely large and floppy in children, under the tip of the blade, allowing a better view of the vocal cords;
Preparation for endotracheal intubation:
-
An assistant, who is familiar with intubation equipment, is essential.
-
Endotracheal tube: Calculate the appropriate size:Age/4 + 4 mm = internal diameter (ID)
Have tubes of the appropriate size, plus tubes 0.5 mm ID smaller and 0.5 mm ID larger than that size, available on the child's bed.
-
Introducer: for ET tubes 4.5 mm ID and smaller, a lightly lubricated stilette inserted almost to the tip of the tube, makes intubation easier.
-
Oral: Always use oral - never nasal - intubation in a child with a head injury, because of the risk of meningitis, and of entering the cranial cavity if there is an undiagnosed fracture of the skull base.
-
Laryngoscopes: Have 2 available. Check the light is bright enough.
-
Suction: -Check it is working. -Use a Yankauer suction catheter. -Place it next to the child's head.
-
Drugs: Draw up and label [see below] -
-
IV cannula + 3-way tap on extension tubing: all patent and visible
-
Have your assistant ready to:
-
Apply Cricoid pressure -Use direct pressure on the cricoid - thumb & index finger both side, and press directly down.
-
Start as the first drug is injected.
-
Don't stop pressure until the ET tube is in place and secure.
-
Give Drugs:
-
Hypnotic first, then flush.
-
Muscle relaxant, then flush.
-
Hand you Equipment: In the correct order?
Rapid sequence induction of anaesthesia:
Used whenever the stomach may not be
empty (i.e. in every injured child)
1. Pre-oxygenate the child:
-
High flow O2;
-
Tightly fitting mask;
-
Three minutes if possible.
2. Drugs: Always used unless the child is flaccid and unresponsive.
-
1st Hypnotic such as thiopentone (3-5mg/kg), midazolam (0.5 mg/ kg) or propofol (2-4 mg/kg);
-
2nd Muscle relaxant such as suxamethonium (1 mg/kg) or rocuronium (1mg/kg).
-
Remember, rocuronium is a relatively long acting muscle relaxant and should not be used if intubation is expected to be difficult.
-
Hypnotic doses should be at the lower end of the range in hypovolaemic patients.
3. Intubate the trachea as soon as relaxed;
Avoid unnecessary bag and
mask ventilation prior to intubation as this may inflate the
stomach, increasing the risk of aspiration.
Laryngoscope: hold in your left hand. Be gentle.
< 1 year: Straight blade (Miller or Robertshaw).
-
Pass the tip over the tongue past the tip of the epiglottis.
-
Lift the epiglottis to see the vocal cords

> 1 year: Curved blade (MacIntosh 2 or 3):
-
Pass the tip over the tongue into the vallecula (space between tongue and epiglottis).
-
Lift the handle towards the ceiling at the far end of the room to bring the vocal cords into view.
-
Don't lever against the teeth.
-
Don't jam the lip between blade and teeth

4. Insert the endotracheal tube.
-
Calculate how far. [(Age/2) + 12] cm at the teeth.
-
Immobilise the tube at the lips.
-
Auscultate both axillae and epigastrium to confirm the tube position.
-
Secure with cotton tape around the neck, or Elastoplast on the face.
5.Insert an orogastric tube on free drainage.
Never use a nasogastric or nasotracheal tube in a child with a head injury (because of risk of meningitis, or of entry of cranial cavity in undiagnosed fracture of the skull base).
6. Check AP chest Xray: The ET tube tip should lie at the level of the medial end of the clavicles. If not, re-position the tube and re-tape.
7. Suction the ET tube carefully each hour - more often, if needed.
8. Humidify the inspired gases using a condenser humidifier (Swedish nose) between the ET tube and the self-inflating bag.
9. Splint the child's arms if necessary (child should be sedated)
Needle cricothyroidotomy
If the airway is completely inadequate, consider:
-
Surgical cricothyroidotomy (> 12 years)
-
Needle cricothyroidotomy (any age; may be used to gain time during surgical cricothyroidotomy)
Rationale for needle cyricothyroidotomy
-
Patent airway not possible by other means.
-
Preferable to surgical airway in children under 12 years of age.
-
Useful for obstruction in the larynx or above; not if the obstruction is in the trachea or bronchi.
-
It improves oxygenation slightly, buying 10-15 minutes' time for help to arrive and for a definitive airway to be established.
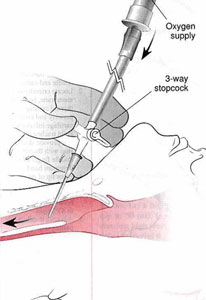
Preparation for needle cricothyroidotomy
-
Continue bag/mask ventilation with O2
-
Prepare equipment:
-
IV cannula: largest available (10 - 16 SWG), with 5 ml syringe;
-
Oxygen tubing + 3-way tap. (If there is no 3-way tap available, cut a 3mm hole in the side of the O2 tubing and, if necessary, cut the O2 tubing to fit over the hub of the cannula.)
-
Place a rolled towel under the child's shoulders.
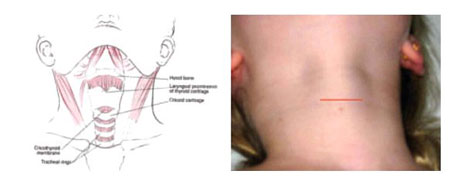
Surface markings
Feel your own cricothyroid membrane: this is the horizontal gap between the thyroid cartilage (Adam's apple) above, and the horizontal cricoid cartilage below.
Surface markings:
-
Stand on the child's left and locate the same structures.
-
Immobilise the trachea between your left finger and thumb.
-
Insert the cannula through the cricothyroid membrane, then 45o downwards towards the feet. STAY IN
THE MIDLINE!
-
Aspirate continuously as soon as the needle is through the skin.
-
When you can aspirate air, the needle is in the trachea. Immobilise the syringe (don't pull it back) and slide the cannula down the needle into the trachea.
-
Tape the cannula in place.
-
Attach the O2 tubing to the cannula.
-
Run O2 at 1 litre/min per year of age.
450 angle:
-
Occlude the side hole of the 3-way tap, or the hole in the O2 tubing, for 1 sec, then release for 4 sec to allow expiration.
Complications to be aware of
-
Asphyxia
-
Aspiration
-
Cellulitis
-
Oesophageal perforation
-
Haemorrhage
-
Haematoma
-
Posterior tracheal wall perforation
-
Subcutaneous and/or mediastinal emphysema
-
Thyroid perforation
-
Inadequate ventilation leading to hypoxia and death