Note: This guideline is currently under review.
Introduction
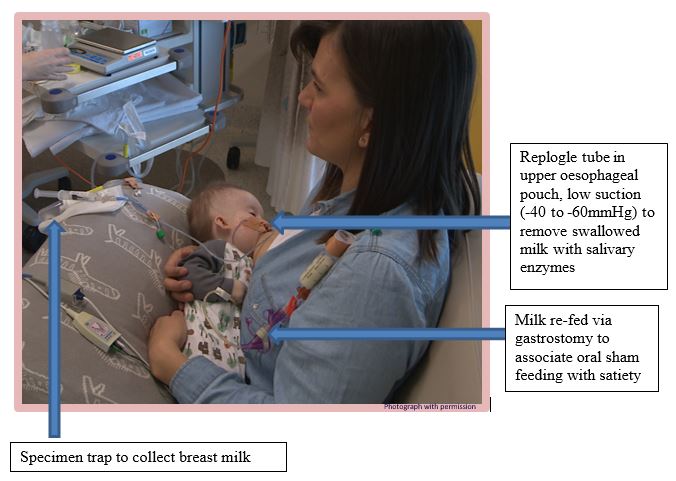
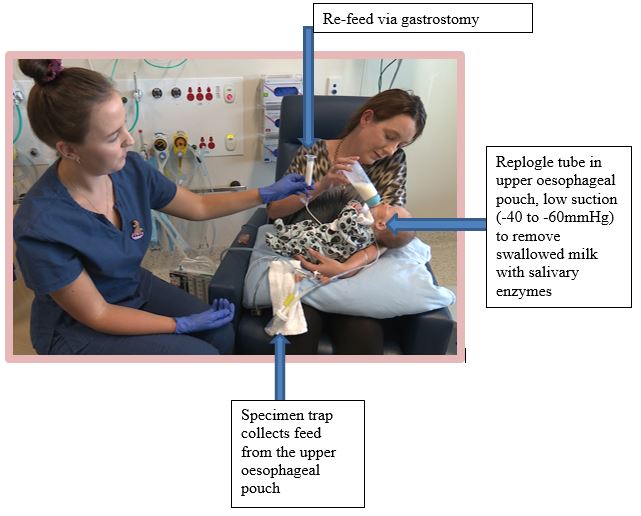
Sham feeding is used to enable the infant to learn to feed orally either by breast or bottle prior to repair of long-gap oesophageal atresia.
A sham feed is a feed given to an infant with unrepaired long-gap oesophageal atresia, with a Replogle tube in the upper oesophageal pouch connected to suction, which drains the milk to prevent aspiration.
The feed is removed from the oesophageal pouch by suction and re-fed to the infant via the gastrostomy tube to associate oral feeding with satiety, with the milk entering the stomach at the same time.
Sham feeding principles
- Breast or bottle feed (maternal preference) to develop suck/swallow ability
- Replogle tube in upper oesophageal pouch, low suction (-40 to -60mmHg) to remove swallowed milk with salivary enzymes
- Milk re-fed via gastrostomy to associate oral feeding with satiety
Rationale for sham feeding
- Neonatal suck/swallow develops in a narrow time window
- Inability to feed orally leads to failure to develop this skill
- Oral aversion and feeding tube dependence are well described in infants with repaired long-gap OA
- Sham feeding has been reported to reduce time to full oral feeding post definitive repair of long-gap OA
Aim
To enable
infants with unrepaired long-gap oesophageal atresia to learn to feed orally.
Definition of terms
Oesophageal atresia (OA): A congenital anomaly in which the oesophagus
ends in a blind upper pouch. Most
neonates with OA also have an abnormal connection between the trachea and
oesophagus; this is called a tracheo-oesophageal fistula (TOF).
Long-gap oesophageal atresia:
Infants with:
- Pure OA
- OA with proximal TOF
- Other variants of OA/TOF with a large gap where an oesophageal anastomosis is unable to be performed immediately.
Infants with long-gap OA are often managed with a delayed oesophageal repair, a growth induction procedure (traction suture techniques) or oesophageal replacement surgery.
Replogle tube: A double lumen tube which
is placed into the oesophageal pouch and connected to continuous low pressure
suction (-20 to -35 cmH20), allowing the pouch to be kept clear of
saliva and secretions which can spill into the lungs.
Tracheo-oesophageal fistula: abnormal connection between the trachea and oesophagus
Traction suture techniques: Involves growth induction of the oesophagus to enable delayed primary oesophageal reconstruction in patients with long-gap oesophageal atresia. Sutures are placed internally on the upper oesophageal pouch and lower end of the oesophagus under tension. Sutures may also be placed on the upper and lower ends of the oesophagus and brought out onto the neonate’s lateral chest wall under tension (e.g. as in the Foker process).
Indications for sham feeding
Infants with long-gap OA awaiting a delayed primary repair by
oesophageal anastomosis, or oesophageal replacement surgery, or those infants
with traction sutures in-situ that are stable postoperatively (and the infant’s
surgeon has requested commencement of sham feeding).
Infant
is stable postoperatively following insertion of a gastrostomy tube and tolerating
more than 100mL/kg/day of bolus enteral feeds via gastrostomy
Important note: The RN prior to caring for a neonate/infant
with unrepaired OA must have successfully completed competencies on:
- Replogle
tube management
- Sham
feeding
Assessment
Assessment of suitability of infant for sham feeding:
- Infants should be more than 35 weeks corrected age, stable, requiring no
respiratory support and able to coordinate sucking, swallowing and breathing
- Infants should be stable on continuous low pressure Replogle tube
suction of the upper oesophageal pouch
- Replogle tube Fg10 ideally positioned in oesophageal pouch via nare
- Sham feeding should only be commenced with consent from the infant’s
Surgeon and Neonatologist
- A proximal TOF should have been excluded prior to commencing sham feeds
in infants with long-gap OA
- Infants with OA and proximal TOF should have recovered from the initial
TOF repair prior to commencing sham feeds
- The Oesophageal Atresia Nurse should be present for the first sham feed
and for all sham feeds in the first 5 days after commencement
Special Circumstances
- Occasionally the infant’s surgeon may request for an infant with traction
(growth induction) sutures in-situ to have sham feeding commenced. Sham feeding in this situation should be
discussed with the Neonatal Consultant and the Oesophageal Atresia Nurse prior
to commencing.
Initial Assessment
- The
infant requires:
- continuous
cardio-respiratory and oxygen saturation monitoring
- assessment
of cardio-respiratory status, with oxygen saturation, heart rate and
respiratory rate within normal limits
- Perform hand hygiene and ensure appropriate personal protective equipment (PPE)
- Ensure
correct position of the Replogle tube in the oesophageal pouch by ensuring
it is secured/taped at the correct length.
- Ensure patency of the Replogle tube prior to
commencing a sham feed
- Gently aspirate the suction lumen of the Replogle
tube, then flush with 2mL sodium chloride 0.9%
- Gently aspirate the 2mL sodium chloride 0.9% back from
the oesophageal pouch
Ongoing Assessment
1. Ongoing assessment of cardio-respiratory status during and post sham feed
- The infant requires continuous cardio-respiratory and
oxygen saturation monitoring
- Observation
for respiratory compromise including:
- Respiratory distress
- Apnea
- Desaturation with oxygen saturation below 90%
- Bradycardia
- Stridor
- Use of accessory respiratory muscles
2. Assessment of feeding including:
- coordination of sucking, swallowing and breathing
- management of feed volume with no coughing, choking or aspiration episodes
If the infant has any signs of respiratory
distress/compromise or difficulty with the sham feed, or coughing or choking
episodes, the sham feed should be ceased immediately. Then the infant should be
reassessed by the Oesophageal Atresia Nurse or Surgical Registrar for safety
regarding sham feeding before another sham feed is attempted by nursing staff.
If the infant shows any signs of oral aversion, or
difficulty coordinating suck, swallow & breathing with sham feeds please
cease the sham feed and contact the Oesophageal Atresia Nurse. Then do not recommence sham feeding until
further assessment by the Oesophageal Atresia Nurse or Surgical Registrar.
If there is any
pink or blood stained aspirate, cease the sham feed immediately and check the
suction pressure is not higher than -60mmHg.
- Flush
the Replogle tube gently with 2mL sodium chloride 0.9% to assess for
continued active bleeding and patency of Replogle tube.
- Contact
the neonatal and surgical teams (and the Oesophageal Atresia Nurse if
available), and withhold sham feeds until consent is given by the surgical team
to continue with sham feeds.
Document any
problems with sham feeding in the EMR (Progress Notes).
Equipment
- New
specimen trap (40mL) for each sham feed
- 20
mL oral syringe
- 10
mL syringe
- 10
mL ampoules of sodium chloride 0.9%
- New
enteral feed set for each sham feed – only if re-feeding via pump set
Technique
1. The Oesophageal Atresia Nurse should be present for the first sham feed & all sham feeding attempts in first 5 days after commencement of sham feeding.
2. Sham feeding may be by breast or bottle (maternal preference). Review orders for sham feeding prior to commencing or administering a sham feed (EMR: NICU Feeding Regime: Sham Feeding).
3. Perform hand hygiene and ensure appropriate PPE.
4. Ensure oxygen saturation probe and cardio-respiratory monitor on with limits set (HR 100-200 and oxygen saturation 90-100%).
5. Disconnect Replogle tube from Atrium UWSD Unit. Ensure Replogle tube is in correct position (correct length) in the oesophageal pouch and patent.
a) Gently aspirate the suction lumen of the Replogle tube with a 10mL syringe
b) then flush with 2mL sodium chloride 0.9% and gently aspirate the 2mL sodium chloride 0.9% back from the oesophageal pouch
c) This flush may need to be repeated (as above) to ensure patency of the Replogle tube.
Record all flushes and Replogle tube drainage in LDA for Replogle tube.
6. Attach a new specimen trap to the Replogle tube and suction tubing. This is to collect the milk feeds.
7. When ready to commence the sham feed, ensure wall suction set to -40 to -60mmHg. Individual recommendation for suction pressure will be ordered by Oesophageal Atresia Nurse.
a. Ensure suction does not go higher than -60mmHg during a sham feed.
b. Observe frequently during the sham feed for fluctuations in the wall suction, and alter the dial to maintain -40 to -60mmHg.
Breastfeed:
- Oesophageal
Atresia Nurse to be present for first sham feed and all sham feed attempts in
the first 5 days after commencement.
- Oesophageal
Atresia Nurse, Clinical Nurse Educator or Clinical Support Nurse to be present
for initial breast feeding attempts in the first 1-2 weeks of sham feeding
- Breastfeeding
may start when suck/swallow/breathing is well coordinated.
- During
breastfeeding infant should be positioned head up with infant’s trunk at least
45 degrees upright.
- Mother
to offer breastfeed. Initial breastfeeds to be offered after mother has
expressed.
- Initially
to offer only 1 breast
- If
breastfeeding well and volumes tolerated over first 2 days, mother can then
offer breastfeed without expressing first; increasing sham feeding as tolerated
to offering both breasts at each feed (when infant on 150mL/kg/day bolus
gastrostomy feeds)
- When
an appropriate volume is taken or the infant is no longer interested in
breastfeeding or the specimen trap is nearly full, re-feed the breast milk
taken by sham feeding into the infant’s gastrostomy by slow gravity feeding.
- empty
the specimen trap of breast milk into an appropriately sized enteral feeding
syringe attached to gastrostomy tube
- and
administer the feed via gravity
- this
prevents waste of salivary enzymes
- This
is the preferred method of re-feeding the sham feed. The breast milk can also be re-fed via the
feeding pump into the gastrostomy only if necessary (with the pump programmed
to deliver the feed over approximately 30 minutes)
- If
re-feeding feed via feeding pump, discard enteral feeding set after each sham
feed
Please note:This
breast milk needs to be re-fed at the same time as the feed; it cannot be kept
for a later feed.
- Give
the gastrostomy feed at the same time as the sham feed; this gives the infant
the sensation of satiety while the stomach is filling with feed during sham feeding
- Burp
infant, as this gets the infant used to burping which will be necessary post
repair of oesophageal atresia
- Following
completion of the sham feed:
- Aspirate the suction lumen of the Replogle tube,
- then flush the Replogle tube with 2mL sodium chloride
0.9% slowly,
- and gently aspirate the 2mL sodium chloride 0.9% back
from the oesophageal pouch to
clear the Replogle tube
- Repeat
flushes (as above) until return is clear
- Disconnect
and discard the specimen trap
- Reconnect
Replogle tube to the Atrium UWSD Unit (suction set between -20 to -35cmH2O,
as set prior to sham feed) to the Replogle tube
- Ensure
wall suction is reset at -80 mmHg
- Record
sham feed in EMR Flow Sheets as a comment in Enteral Feeding section (enter
breastfeed and volume taken by sham) to provide a reference for how sham feeding
is progressing
- Once
tolerating sham feeds well, aim to grade infant up over a number of weeks to
3-4 sham feeds per day
![]()
Bottle feed:
Family Centred Care
It is the responsibility of the clinician caring for the infant receiving sham feeding to ensure that the parents understand the rationale for the intervention, as well as potential complications.
Companion Documents
- Aseptic technique
- Emergency Procedures
- Replogle tube management
- Intermittent oesophageal pouch suction guideline
- Sham feeding in oesophageal atresia at Victoria General Hospital, Vancouver– DVD
Links
http://oara.org.au/
http://www.tofs.org.uk/home.aspx
References
Alberti D, Boroni G, Corasaniti L & Torri F. (2011). “Esophageal atresia: pre and post-operative management.’ Journal of Maternal-Fetal and Neonatal Medicine, 24 S(1): 4-6.
Bairdain, S., Hamilton, T.E., Smithers, C.J., Manfredi, M., Ngo, P., & Gallagher, D., Zurakowski, D., Foker, J.E., & Jennings, R.W. (2015). Foker process for the correction of long gap esophageal atresia: Primary treatment versus secondary treatment after prior esophageal surgery. Journal of Pediatric Surgery, 50(6): 933-937. doi: 10.1016/j.jpedsurg.2015.03.010
Desrosiers, C, Thiboutot, L, Faure, C & Aspirot, A. (2016). Sham feeding in children with long gap esophageal atresia: A controlled study. 4th International Conference on Esophageal Atresia, Sydney, September.
Foker, J. E.; Kendall Krosch, T.C.; Catton, K., Munro, F.; Khan, K.M. (2009). Long-gap esophageal atresia treated by growth induction: the biological potential and early follow-up results. Seminars in Pediatric Surgery, 18(1): 23-29.
Golonka, NR, & Hayashi, AH. (2008). ‘Early “sham” feeding of neonates promotes oral feeding after delayed primary repair of major congenital esophageal anomalies.” The American Journal of Surgery, 195: 659-662.
Hawley, A.D, Armstrong, R.K, Brooks, J-A, E, Pellicano, A, Nightingale, M.G, Crameri, J, & Teague, W.J. (2019). Sham feeding promotes oral feeding success in long-gap esophageal atresia, even with traction sutures in situ. Diseases of the Esophagus, 32 (supplement 1): 22
Retrieved November, 11, 2019 from https://academic.oup.com/dote/article/32/Supplement_1/doz047.64/5518460
Hawley, A, McLeod, EJ & Hunt, RW. (2011). Tube feeding dependence in infants with repaired oesophageal atresia and distal trachea-oesophageal fistula. Journal of Paediatrics and Child Health, 47 (S1), April, pp. 86.
Lemoine, C., Faure, C., Villeneuve, A., Barrington, K., Desrosiers, C., Thiboutot, L., Beaunoyer, M., & Aspirot, A. (2014). Feasibility and safety of sham feeding in Long Gap Esophageal Atresia. 3rd International Conference on Esophageal Atresia, Rotterdam (October, 2014). Retrieved May 5, 2016 from www.we-are-eat.org/wp-content/uploads/2014/10/181.pdf
Lemoine, C, Faure, C, Villeneuve, A, Barrington, K, Desrosiers, C, Thiboutot, L & Aspirot, A. (2016). P-21: Feasibility and safety of sham feeding in long gap esophageal atresia. Diseases of the Esophagus, Volume 29, Issue 3, 1 April 2016, Page 294, https://doi.org/10.1093/dote/29.3.294b
Sri Paran T, Decaluwe D, Corbally M, Puri P. (2007). ‘Long-term results of delayed primary anastomosis for pure OA: a 27 –year follow-up.’ Pediatric Surgery International, 23 (7): 647-651.
Vancouver Island Health Authority – Special Care Nursery Unit Manual. (2010). ‘Guidelines for sham feeding infants with esophageal atresia.’
Weems, M. (2018). Pilot study on sham feeding in post-operative gastrointestinal surgery infants. ClinicalTrials.gov Identifier: NCT03350022. NIH. U.S National Library of Medicine. ClinicalTrials.gov. Retrieved 11th November, 2019 from
https://clinicaltrials.gov/ct2/show/NCT03350022
Evidence Table
Sham feeding for infants with unrepaired long-gap oesophageal atresia Evidence Table.
Please remember to read the disclaimer
The
development of this nursing guideline was coordinated by Alisa Hawley, Lactation Consultant (IBCLC) / Oesophageal Atresia Nurse, Koala Ward and approved by the Nursing Clinical Effectiveness Committee. Updated November 2020.