Introduction
Drainage of fluid, or evacuation of air, from the pericardial and pleural spaces after cardiothoracic surgery is necessary to prevent effusions, tamponade or pneumothoraces and to also detect hemorrhage. Therefore negative pressure drains are placed in the mediastinum and pleural cavities. The type of drain inserted are closed systems and include: the AtriumTM underwater sealed drain (UWSD) (Atrium Ocean, Atrium Medical, Hudson, USA), the Redon RedivacTM drain (PFM Redon system, Mepro, Koln Germany), the Jackson-PrattTM drain (Cardinal Health, Waukegan, Illinois) and/or the ConvaTec MinivacTM drain (ConvaTec, NewZealand).
NB: Passive drainage systems with an attached collection bag (such as a urine or bile bag) is not used following cardiothoracic surgery.
Aim
To provide a description of the types of drains available and to describe the safe and competent nursing management of Redivacᵀᴹ and Jackson-Prattᵀᴹ drains in the post-operative cardiac surgical patient. Management of UWSD can be found in the following link:
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
Definition of Terms
- Cardiac surgical procedures: Please refer to the cardiology intranet site
- Mediastinum: The region between the pleural sacs, containing the heart and all of the thoracic viscera except the lungs
- Pleural Cavity: The potential space between the two pleurae (visceral and parietal) of the lungs
- Pleural Effusion: Increased fluid in the pleural space
- Pericardial Space: The space between the layers of the pericardium that contains fluid that lubricates the membrane surfaces of the heart and allows easy heart movement
- Sternotomy: Surgical procedure in which a vertical inline incision is made along the sternum, after which the sternum itself is divided to provide access to the heart
- Thoracotomy: Incision into the chest wall either made on the side or under the arm to gain access to the heart for certain cardiac procedures.
- Tamponade: Is an acute effusion caused by the accumulation of fluid in the pericardial space, resulting in reduced ventricular filling and subsequent hemodynamic compromise
The following terms are defined in the
Chest Drain Management Clinical Guideline
- Chylothorax
- Haemothorax
- Pneumothorax
- Tension Pneumothorax
- Pleural effusion
Types of Drains inserted in the pleural and mediastinal space
The type and location of drain insertion should be clearly identified in the LDA section of the patients EMR.
Children with multiple drains following cardiac surgery will have each drain labelled appropriately in terms of the location of drain insertion, i.e either “left pleural”, “right pleural” or “mediastinal” space.
Atriumᵀᴹ Underwater Seal Drain (UWSD) (Atrium Ocean, Atrium Medical, Hudson, USA) (Figure 1)
This is considered a conventional drainage system that is attached to low-pressure wall suction to maintain a negative pressure between -5cm H2O and -20cmH2O (1.96kPa); unless stated otherwise suction should be applied at all times (see chest drain management CPG).
The tubing is soft silicone, however semi-rigid tubing can be attached to the silicone tubing and inserted into the patient. The drainage system allows collection of fluid up to 2L.
UWSD is preferred if a significant drop in mean arterial pressure is a concern which can occur after surgery of single ventricle anomalies.
Pigtail tubing maybe attached to an UWSD if pneumothorax or pleural effusion develops after cardiac surgery.
These drainage systems are preferred in situations where there may be an ongoing air leak (eg: open chest/delayed sternal closure) or when accurate measurement of losses are required or large volumes of drainage are expected.

Figure 1. Atriumᵀᴹ Underwater Seal Drain (UWSD)
Redon Redivacᵀᴹ Drain (PFM Redon system, Mepro, Koln Germany) (Figure 2)
- This drainage system maintains a consistent high negative pressure of up to 90KPa without the need for wall suction.
- The tubing is semi-rigid and two canister sizes are available which allows a drain capacity of either 200ml or 600ml.
- This high vacuum drain has been found to result in lower incidence of residual pleural and mediastinal effusions requiring drainage, are easier to care for, allow for earlier mobilization of patients and are most cost effective than conventional UWSD.
- Redivac drains are inserted in the pleural space, superficial mediastinum, or following delayed sternal closure to minimise risk of infection. NB: Redivac drains will not be used following delayed sternal closure in some single ventricle anomalies, as it can lead to a significant drop in mean arterial pressure and consequently high negative pressure in the chest.
- Redivac drain canisters may be changed to UWSD collecting system in particular circumstances such as significant air leak and/or excessive drainage.

- Figure 2. Redon Redivacᵀᴹ Drain
Jackson-Prattᵀᴹ Drain (Cardinal Health, Waukegan, Illinois) (Figure 3)
- This drainage system maintains low negative pressure without the need for wall suction. The soft canister is squeezed to create suction.
- The tubing inserted into the patient is flat or round and soft, two canister sizes are available which allows a drain capacity of either 100ml or 400ml.
- Jackson-Pratt drains, if used, are inserted in the mediastinal space in the cardiac transplant patients.
- The Jackson-Pratt drain maybe changed to a redivac drain as per surgeon’s preference

Figure 3. Jackson-Prattᵀᴹ Drain
Minivacᵀᴹ Drain (ConvaTec, NewZealand) (Figure 4)
- This drainage system maintains low negative pressure without the need for wall suction.
- The concertina drain is squeezed to create suction
- Minivac drains maybe inserted in the superficial mediastinum in neonates or following delayed sternal closure to minimise risk of infection. The decision for the drain to be redivac or minivac in the mediastinum is as per surgeon’s preference.

Figure 4. Minivacᵀᴹ Drain
Patient Group
• The patient group will have undergone cardiac or thoracic surgery and will have had a median sternotomy or thoracotomy wound incision. Patients attending cardiac preadmission clinic will receive the Cardiac Surgery Information Guide For parents, carers and families which provides information of the post-operative course, including chest drain management; ward staff should check such information has been received.
Management
Start of shift checks
- Patient assessment
- Chest drain assessment
Patient assessment
Patient monitoring
- Patients in Rosella returning from cardiac theatre should be on continuous cardiac monitoring
- HR, SaO2, BP, RR
- A systems approach to assessment is undertaken hourly or more frequently if necessary and documented accordingly
- Patients transferred to the wards undergo a full primary assessment and are assessed 1-4 hourly as indicated by patient condition.
Pain and Patient Positioning
- Chest drains are painful as the parietal pleura is very sensitive. Patients require regular pain relief for comfort and to allow them to ambulate and participate in physiotherapy.
- Post – operative cardiac patient’s with a chest drain insitu will have a narcotic infusion continued on transfer from Rosella to Koala ward.
- In addition to assessing patient’s rating of pain, it should also include assessing positions that are comfortable for the child, and ensuring the drains are well secured during movement.
- Parents should be encouraged to participate in their child’s activities of daily living such as hygiene and comfort needs (eg: nappy changes and cuddling) but emphasis should be placed on monitoring to ensure the drain is well secured.
- Patients who are ambulant post operatively will have fewer complications and shorter length of stay.
- Patients on strict bed rest should have regular position changes to promote drainage and prevent pressure areas.
Drain Insertion Site
- Observe for signs of infection, inflammation or pressure sores and document findings
- Ensure drains are anchored appropriately so as to minimise pressure areas and pulling of drains. Anchoring of drains can be found in the Chest Drain Management Clinical Guideline
- Check dressing is clean and intact. Drain dressings should be changed:
- Routinely every 3 days
- When dressing is no longer intact, wet or soiled
- Daily if drain sites are infected
- Observe sutures remain intact and secure.
- Redivacs are less likely to be utilised in a long term drainage situation but observe for the erosion of sutures over time.
Chest Drain Assessment
Safety Equipment
- Two chest drain clamps per drain should be available to use in an emergency such as an accidental disconnection.
- NB: Drains should not be routinely clamped for transport.
Vacuum
- The presence of vacuum suction should be assessed hourly.
- Ensure all connections between drainage tube and suction unit are tight and secure.
Vacuum on the Redivac system
- The system consists of a solid clear plastic canister, with a green plastic concertina on top to monitor the presence of vacuum pressure. If vacuum pressure is present in the system the concertina is tightly compressed. When suction is lost the concertina is extended.
- Provided the suction is “on” then there is continuous suction which is facilitating drainage despite the unit and tubing being above or below the patient’s chest level. The higher the negative pressure the greater the vacuum and so it is acceptable for the drain to be above the chest. However, for safety the unit and tubing should be equal to or below the patient’s chest.
- The black lines on the redivac drain tubing are radiolucent, meaning x-ray can confirm position. Therefore the black lines on the tubing should not be visible outside the patient.
Vacuum on the Jackson-Pratt system
- The system consists of a soft clear canister which can be compressed to create suction.
- The white silicon tube that is placed internally is radiolucent, allowing x-ray to confirm position, and should not be visible outside the patient.
Drainage
- Ensure slide clamps on drain tubing are open to allow for drainage.
- Care should be taken to ensure there are no kinks or obstruction of
the tubing that may inhibit drainage. Avoid unnecessary loops in tubing.
- Document hourly the amount of fluid in the drainage chamber on the
EMR fluid balance chart.
- Calculate
and document total hourly output if multiple drains.
- Calculate
and document cumulative total output
- Notify medical staff if there is sudden increase in the amount of
drainage
- Greater
then 5ml/kg in 1hr
- Greater
then 3ml/kg consistently for 3 hours.
- Blocked drains are a major concern and Redivac and Jackson-Pratt
drains have a smaller internal diameter than a UWSD.
- Notify
medical staff if a drain with ongoing losses suddenly stops draining.
- Monitor colour/type of drainage. If there is a change, eg:
haemoserous to bright red, or serous to creamy, notify medical staff.
Specimen Collection
- The Redivac
and Jackson-Pratt drainage tubing cannot be accessed with a needle, it is not
self-sealing.
- To
collect a sample from a Redivac the whole canister must be changed and sent to
the lab (see below)
- To
collect a sample from a Jackson-Pratt a leur lock syringe can be attached to
the port to aspirate a sample (see below)
Changing the redivac chamber
- The
Redivac chamber needs changing when the chamber is ≥¾ full, when
the vacuum is not maintained, if a drain sample is needed (for example; to
assess for chylothorax) , or if the sterility of the system has been
compromised (i.e accidental disconnection)
- This procedure should be performed using a surgical aseptic
technique.
- Equipment:
- Eye protection
- New Redivac chamber
- Dressing pack
- Sterile gloves
- 2% Chlorhexidine in
70% alcohol
- Procedure:
- Prepare patient
- Don eye protection to
protect eyes from possible body fluid exposure
- Perform
hand hygiene
- Open dressing pack by
using corners to protect aseptic field
- Peel open sterile
equipment and drop onto sterile field, including new Redivac chamber, ensure chamber
is clamped and green concertina is compressed.
- Close the clamps on
the old bottle and on the drain tubing. This ensures no air can escape back
into the patient.
- Perform hand hygiene
- Don Sterile Gloves
- Disinfect key part connections
(attached to old bottle) using gauze soaked in 2% Chlorhexidine in 70% alcohol
and allow to dry for 30 seconds, dispose of used gauze into waste
- Remove drain tubing
from old bottle
- Connect tubing to new
bottle
- Release clamp on new
bottle
- Release clamp slowly
on drain tubing
- Check for suction and
free flow
- Discard old bottle,
or as ordered send to pathology for specimen
- Dispose of waste,
remove gloves and perform hand hygiene
- Document change of chamber
on EMR Fluid Balance Chart.
Taking a sample from a Jackson-Pratt Drain
- This procedure should be using a standard aseptic technique.
- Equipment:
- Eye protection
- One drain clamp
- Clean tray
- 10mL leur lock syringe
- Non-sterile gloves
- Sterile gauze
- 2% Chlorhexidine in 70% alcohol
- 70% Alcohol
- Procedure:
- Don eye protection to protect eyes from possible body fluid exposure
- Clean tray with 70% alcohol
- Perform hand hygiene
- Open leur lock syringe and gauze onto tray, leave the equipment in the clear packaging (micro aseptic field)
- Pour 2% chlorhexidine in 70% alcohol over gauze
- Clamp Jackson-Pratt tubing
- Perform hand hygiene and don non-sterile gloves
- Clean the port of the canister with the gauze soaked in chlorhexidine and allow to dry for 30 seconds
- Once port is dry attach 10mL leur lock syringe and aspirate sample
- Squeeze the canister and close the port
- Release the clamp
- Dispose of waste, remove gloves and perform hand hygiene, clean tray.
Troubleshooting
Loss of high vacuum suction on redivac drain
- If the vacuum is lost, the drain will not function. Loss of vacuum results from
inappropriate connection along the drain tube or between tube and chamber.
Depending on the cause of loss of suction the drain tube plus chamber or just
the chamber will need to be replaced.
Converting a redivac to an underwater seal drain (UWSD):
- It may be necessary to convert the redivac
drainage bottle to an UWSD. Incidents where this may be necessary include
increased drainage, large pneumothorax causing
continuous loss of suction and/or unsuccessful attempts at re-establishing
vacuum.
- Consultation with the
cardiac surgical team must be made prior to converting to an UWSD.
- This procedure should
be performed using a surgical aseptic technique
- Equipment:
- Clean trolley
- Eye protection
- Two drain clamps
- Clear Tube Adaptor –
small/large (Code: TA410PP-S)
- UWSD
- Sterile towel
- Sterile dressing pack
- Sterile scissors or
scalpel
- Sterile Gloves
- 2% Chlorhexidine in
70% alcohol
- 70% Alcohol
- Cable ties and cable gun
- Procedure:
- Don eye
protection to protect eyes from possible body fluid exposure
- Clean
dressing trolley with 70% Alcohol
- Perform
hand hygiene
- Onto
the trolley open the UWSD and spread open blue wrapping by using the corners so
it can act as an aseptic field
- Open sterile dressing
pack onto this blue wrapping with UWSD to one side
- Peel open sterile
scissors or scalpel and drop onto aseptic field
- Peel open sterile
towel and drop onto aseptic field
- Clamp Redivac drain
tubing close to patient but below any existing tube connections (the tube
inserted into the patient may also be connected to tubing with the redivac
bottle, leave these two tubes connected and clamp below connection)
- Perform hand hygiene
and don sterile gloves
- Perform procedure
ensuring all key parts are protected
- Place sterile towel
under redivac tubing (Figure 5)
- With 2% Chlorhexidine
in 70% Alcohol disinfect the area 5cm above and below the site you will cut
- Cut the Redivac tubing
using scissors or scalpel.
- This tubing with
redivac drain will be thrown away or sent to pathology as ordered for sample
collection
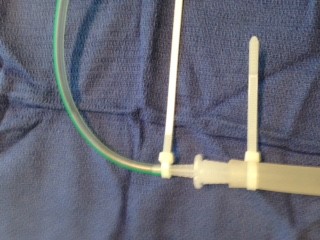
- Insert the thin end
of Clear Tube Adaptor into tubing as far as possible (this is a tight fit) (Figure
6)
- There is a connector
attached to the UWSD – cut this off
- Insert the other end
of the Clear Tube Adaptor into the tube of the UWSD (Figure 7)
- With cable ties and
cable gun (Figure 8a), cable tie over connections (Figure 8b)
- Ensure suction is on
UWSD as per order, then remove drain clamps from tubing.
- Refer to the
following guideline to manage UWSD: http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
Figure 5
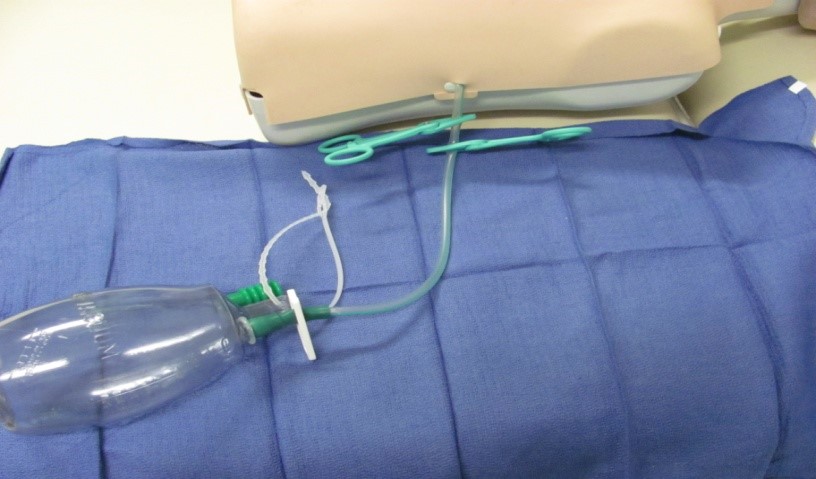
Figure 6

Figure 7

Figure 8a

Figure 8b
Removal of redivac drain
- Medical
documentation is required in EPIC by the cardiac team for the removal of a
chest drain
- Prior
to removal of the drain, clamp tubing as the drain must not be removed under
suction
- Consider
pain management and procedural sedation
- Perform
hand hygiene
- Removal
of Redivac and post-procedure care follows the same as the removal of UWSD:http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
- Inspect end of drain to order to ensure
entire drainage tube has been removed. Jagged or torn appearance could be
signs of the tube fracturing.
- If
this is a concern contact the cardiac surgical fellow and treating team, a
chest x-ray should be performed immediately once ordered by the surgical
fellow, the patient should be kept nil by mouth in anticipation for
surgical removal of the tube that has been left in the patient, keep the
whole redivac unit in the patient’s room until surgical review and collection for
quality review.
- A VHIMS must be
completed by the nurse delegated to remove the drain.
- For further
information on managing missing or non intact drains refer to the
following link:
https://www.rch.org.au/policy/policies/Surgical_Wounds__Procedure_for_Missing_or_Non_Intact_Drains/ - Staff involved in
reinserting the drain on the ward or surgical staff involved in removing
the retained drain tube please see the following guideline: http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_Drain_Management/
Further complications and troubleshooting
Special Considerations
- A VHIMS report should be made for any adverse events such as accidental disconnection or piece of tubing left in during removal of drain
Documentation
- The presence of vacuum suction should be assessed hourly and
documented on the EMR fluid balance chart
- Document hourly in the fluid balance chart the amount of fluid in
each drainage chamber
- Each shift observe key sites for signs of infection, inflammation
or pressure sores and document finding in EMR-> LDA
- Document change of drain site dressings
- Document change of chamber on fluid balance chart
- Document when purse-string drain sutures need to come out post
drain removal to prevent risk of embedded suture or infection, usually sutures
are removed 5 days post drain removal.
Links
Evidence Table
Evidence Table:
Pleural and Mediastinal Drain Management after Cardiothoracic Surgery
References
- Berg,
H; Brands WG; Van Geldorp TR;
Kluytmans-VandenBergh FQ; Kluytmans JA. (2000). Comparison between closed drainage techniques for the
treatment of postoperative mediastinitis. The
Annals of Thoracic Surgery. 70; 924-929.
- Durai,
R, and Philip, C. (2010). Surgical Vacuum Drains: Types, uses and
complications. AORN. 91 (2); 266-271.
- Meyerson,
J.M (2016). A Brief History of Two Common Surgical Drains. Annals of Plastic Surgery, 77 (1); 4-5.
- Newcomb,
A; Alphonso N; Norgaard M; Cochrane A; Karl T; Brizard C. (2005) High-vacuum
drains rival conventional underwater-seal drains after pediatric heart surgery.
European Journal of Cardiothoracic Surgery. 27:395-400
- Paddle,
A; Elahi, M and Newcomb, A (2010). Retained foreign body following pleural
drainage with a small-bore catheter. General
Thoracic Cardiovascular Surgery, 58: 42-44.
- Salvatore,
A; Mignosa, C; Gitto, P; Santo Trimachi, E; Ciccarello, G; Salvo, D; Trimarchi,
G (2006). A method for chest drainage after pediatric cardiac surgery: A
prospective randomized trial. The Journal
of Thoracic and Cardiovascular Surgery, 131(6): 1306-1309
- Pfm medical Redon Drains – Low Vacuum and
High Vacuum Drainage. www.pfmmedical.com
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Annabelle Santos, CSN, Koala, and approved by the Nursing Clinical Effectiveness Committee. Updated October 2021.