For acute medical and surgical pain in children
Introduction
Aim
Definition of Terms
Assessment
Pain Assessment Tools
Physiological Indicators
Key Considerations
Special Considerations
Companion Documents
Links
Education
Evidence Table
Introduction
Pain assessment is crucial if pain management is to be effective. Nurses are in a unique position to assess pain as they have the most contact with the child and their family in hospital. Pain is the most common symptom children experience in hospital. Acute pain (noiciception) is associated with tissue damage and an inflammatory response, it is self limiting of short duration and does not involve neural tissue.
Pain is multidimensional therefore assessment must include the intensity, location, duration and description, the impact on activity and the factors that may influence the child’s perception of pain (bio psychosocial phenomenon) The influences that may alter pain perception and coping strategies include social history/issues, cultural and religious beliefs, past pain experiences and the first pain experience. In addition family response to their child in pain can have a negative or positive influence.
Aim
The guideline specifically seeks to provide nurses with information regarding
- Indications for pain assessment
- Type of tools used for pain assessment
- Documentation of pain assessment
Definition
of Terms
Pain:
- “Pain is whatever the experiencing person says it is, existing whenever the experiencing person says it does” (McCaffery, 1989)
- “Pain is an unpleasant sensory and emotional experience, associated with, or resembling that associated with, actual or potential tissue damage” (IASP 2020)
Pain assessment: is a multidimensional observational assessment of a patients’ experience of pain.
Pain measurement tools: are instruments designed to measure pain.
Assessment
Pain assessment is a broad concept involving clinical judgment based on observation of the type, significance and context of the individual’s pain experience.
There are challenges in assessing paediatric pain, none more so than in the pre-verbal and developmentally disabled child. Therefore physiological and behavioural tools are used in place of the self-report of pain. However in children with developmental disabilities there can be incorrect assumptions and there is a risk of under-treating pain. It is important to take behavioral cues identified by parents and caregivers to improve pain assessment in these children.
Pain assessment in infants and children is also challenging due to the subjectivity and multidimensional nature of pain. The dependence on others to assess pain, limited language, comprehension and perception of pain expressed contextually. In some children it can be difficult to distinguish between pain, anxiety and distress.
Assessment and documenting pain is needed in order to improve management of pain. When assessing a child’s level of pain careful consideration needs to be given to their:
- cognitive ability
- environment (hospital)
- anxiety
- cause of pain (eg: post-operative)
Pain measurement quantifies pain intensity and enables the nurse to determine the efficacy of interventions aimed at reducing pain.
A pain assessment should be conducted during a patient’s admission. (link to
Nursing Assessment nursing clinical guideline)
Points to consider:
- pain history
- location of pain
- intensity of pain
- cognitive development and understanding of pain
When to assess pain?
- Pain scores should be documented for all children at least once per shift in Flow Sheet: (
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Observation_and_Continuous_Monitoring/)
- Children with pain should have pain scores documented more frequently.
- Children who are receiving oral analgesia should have pain scores documented at least 4 hourly during waking hours.
- Children on complex analgesia such as intravenous opioid and/ or ketamine, epidurals or regional analgesia should have hourly pain and sedation scores documented.
- Assess and document pain before and after analgesia, and document effect.
- Assess and document pain on activity such as physiotherapy.
Pain
Assessment Tools
Tools used for pain assessment at RCH have been selected on their validity, reliability and usability and are recognized by pain specialists to be clinically effective in assessing acute pain. All share a common numeric and recorded as values 0-10 and documented on the clinical observation chart as the 5th vital sign.
The importance of using the same numeric value (0-10) is that the number relates to the same pain intensity in each tool.
Three ways of measuring pain:
- Self report - what the child says ( the gold standard)
- Behavioural –how the child behaves
- Physiological –clinical observations
Pain Assessment Tools used at RCH
There are three main tools used for the
neonate, infant and child 3-18 years these tools reflect a combination of self-report
and behavioural assessment.
1.
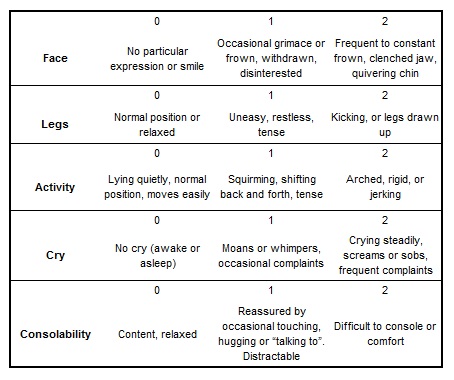
FLACC - The acronym FLACC stands for Face,Legs, Activity, Cry and Consolability.
Behavioural
- 2 months-8 years and also used up to 18 years for children with cognitive impairment and/or developmental disability (always elicit support from parents or carers to help with pain assessment)
- It may be difficult to assess children with cognitive impairment and/or are non-verbal. Ask the parent or carer to help you explain their child’s pain behaviour.
How to use FLACC
Each category (Face, Legs etc) is scored on a 0-2 scale, which results in a total pain score between 0 and 10. The person assessing the child should observe them briefly and then score each category according to the description supplied.
FLACC has a high degree of usefulness for cognitively impaired and many critically ill children
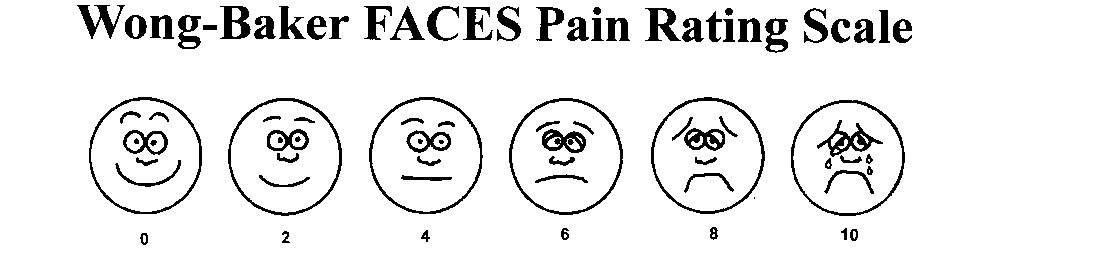
2. Wong-Baker
faces pain scale 3-18yo
Self report
How to use?
Explain to the person that each face is for a person who feels happy because he has no pain (hurt) or sad because he has some or a lot of pain. Face 0 is very happy because he doesn't hurt at all. Face 2 hurts just a little bit. Face 4 hurts a little more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don't have to be crying to feel this bad. Ask the person to choose the face that best describes how he is feeling.
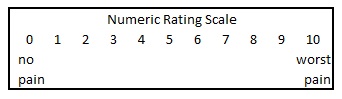
3. Visual
Analogue scale 8-years and older
Self report
How to use?
Ask the child using numbers from 0 = no pain through to 10 being the worst pain
Physiological
indicators
- heart rate may
increase
- respiratory rate and
pattern may shift from normal ie: increase, decrease or change pattern
- blood pressure may
increase
- oxygen saturation may
decrease
Physiological indicators in isolation cannot be used as a measurement for pain. A tool that incorporates physical, behavioural and self report is preferred when possible.
Key considerations
- assess pain using a developmentally and
cognitively appropriate pain tool
- reassess pain after interventions given
to reduce pain (eg. Analgesia) have had time to work
- assess pain at rest and on movement
- investigate higher pain scores from
expectation
- document pain scores
- use parent/guardian pain behaviour
knowledge for children with cognitive impairment.
Special
Considerations
Multi language Wong Baker and Numeric tools are available if needed
https://www.briggshealthcare.com/Wong-Baker-Faces-Pain-Rating-Scale-8-Languages
Modified PAT Tool is used in the Neonatal Intensive Care Unit
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Neonatal_Pain_Assessment/
Comfort B is used for Ventilated paediatric patients assessing both pain and sedation
http://www.rch.org.au/picu_intranet/guidelines/Nursing_management_of_the_patient_with_invasive_mechanical_ventilation_in_PICU/
Companion Documents
Further
information on pain management principles and assessing pain in children can be
found here:
Links
Education
- Supported through the Anaesthesia and pain management web site
- Competencies
- Presentation to ward nurses
- Presentation to RCH nursing programs
- Pain tools supplied to all staff
Evidence Table
The evidence table for this guideline can be viewed by clicking here.
Please remember to
read the disclaimer.
The development of this nursing guideline was coordinated by Sueann Penrose, CNC, Children's Pain Management Service, and approved by the Nursing Clinical Effectiveness Committee. Updated August 2022.