Introduction
Nursing documentation is essential for clinical communication. Documentation provides an accurate reflection of nursing assessments, changes in clinical state, care provided and pertinent patient information to support the multidisciplinary team to deliver individualised care. Documentation provides evidence of care and is
an important professional and medico legal requirement of nursing practice.
Aim
To provide a structured and standardised approach to nursing documentation for inpatients. This will ensure consistent clinical communication processes across the RCH.
Definition of Terms
- EMR: electronic medical record
- EMR Review: process of working through the EMR activities to collect pertinent patient details.
- The Hub: presents a timeline view of the orders, events, and requirements for each patient the nurse is assigned to and facilitates efficient documentation.
- Real time: nursing documentation entered in a timely manner throughout the shift.
- Required documentation: minimum documentation required to reflect safe patient care. On admission and at the commencement of each shift, all ‘required documentation’ must be completed to comply with the
National Safety & Quality Health Service Standards. There is an expectation that shift required documentation is completed within 3 hours of shift start time.
Process
Nursing documentation is aligned with the ‘nursing process’ and reflects the principles of assessment, planning, implementation and evaluation. It is continuous and nursing documentation should reflect this.
Fig 1. Nursing Process
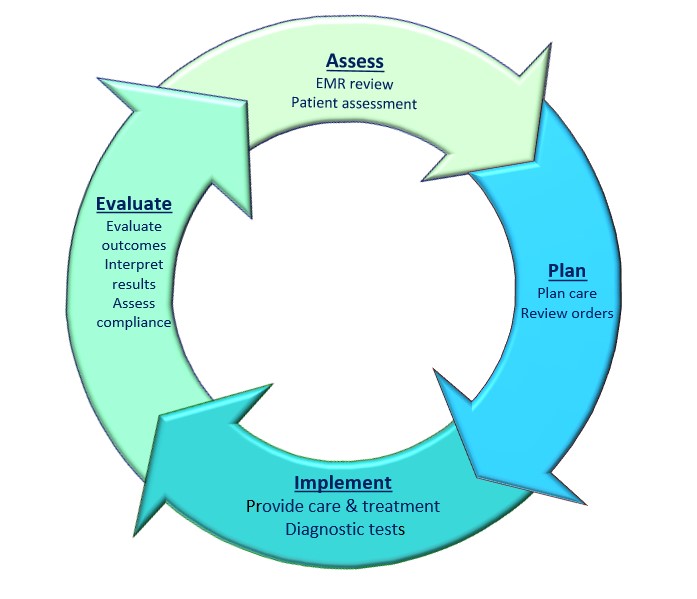
Please note nursing process theory referenced includes an additional phase ‘diagnosis’ which includes identification of problems, risk factors and data analysis, for the purpose of the Nursing Documentation guideline ‘diagnosis’ could occur at any phase and should be documented in real time.
Reference
Fig 1: Nursing Theory, the Nursing Process
The Nursing Process - Nursing Theory (nursing-theory.org) accessed
2/2/2023
Assess
At the beginning of each shift, a ‘primary assessment’ is completed as outlined in the
Nursing Assessment Guideline. The information for this assessment is gathered from bedside handover, patient introductions, required documentation (safety checks and risk assessments, clinical observations) and an EMR review and is documented in relevant the ‘Flowsheets’.
Review of the EMR gives an overview of the patient. To complete an EMR review, enter the patients’ medical record and work through the key activities in order. The Patient storyboard has a significant information which can be viewed by hovering over sections. The tabs across can
be customised to meet the specific needs of your patient group (EMR learning resources). It is recommended that each ward standardises the layout based on their patient population.
The EMR review should include (*indicates essential);
- *Patient storyboard - age, treating team, FYIs, infections, allergies, isolations, LOS, weight
- *IP Summary - Medical problem list, treatment team, orders to be acknowledged
- *ViCTOR Graph - observations trends, zone breaches
- *Notes - e.g. admission, ward round, any other useful details (mark all as not new)
- *Results Review - recent and pending results (time mark)
- *MAR - overdue medications, discontinued, adjust due times for medications
- Fluid Balance- input/output and balance
- Avatar- review lines/drains/airways/wounds, including, location, size, date inserted
- *Orders:
- review all active, continuous, PRN and scheduled, discontinue expired,
- nursing orders create and manage as required for patient care
- Flowsheets - document specific information, ‘last filed’ will show most recent entries, review and manage unnecessary rows e.g. ‘complete’
- The Hub
Patient details are documented in the relevant flowsheets and must include the minimum ‘required documentation’. To ensure required documentation for each patient is complete, use the links from the Hub or other sections of EMR (EMR learning resources).
Plan
With the information gathered from the start of shift assessment, the plan of care can be developed in collaboration with the patient and family/carers to ensure clear expectations of care.
The Hub is a shift planning tool and provides a timeline view of the plan of care including, ongoing assessments, diagnostic tests, appointments, scheduled medications, procedures and tasks. The orders will populate the hub and nurses can document directly
from the hub into Flowsheets in real-time. Orders are visible by the multidisciplinary team.
Management of orders is crucial to the set up and useability of the hub. It must be ‘cleaned up’ before handover takes place - too many outstanding orders is a risk to patient safety.
For more information on how to place and manage orders, click on the
following tip sheet:
Nursing Hub.
Additional tasks can be added to the hub by nurses as reminders. All patient documentation can be entered into Flowsheets (observations, fluid balance, LDA assessment) throughout the shift.
Nursing staff can also document patient care in narrators or navigators as appropriate i.e. ATD navigators.
Clinical information that is not recorded within flowsheets, narrators or navigators and any changes to the plan of care is documented as a real time progress note.
This may include:
- Abnormal assessment, e.g. Uncontrolled pain, tachycardic, increased WOB, poor
perfusion, hypotensive, febrile etc.
- Change in clinical state, e.g. Deterioration, improvements, neurological status,
desaturation, etc.
- Adverse findings or events, e.g. IV painful, inflamed or leaking requiring removal,
vomiting, rash, incontinence, fall, pressure injury; wound infection, drain
losses, electrolyte imbalance, +/-fluid balance etc.
- Patient outcomes after interventions e.g. Dressing changes, pain management,
mobilisation, hygiene, overall improvements, responses to care etc.
- Family centred care e.g. Parent level of understanding, participation in care,
child-family interactions, welfare issues, visiting arrangements etc.
- Social issues e.g. Accommodation, travel, financial, legal etc.
Implement and evaluate
Progress note entries should not simply list tasks or events but provide information about what occurred, consider why and include details of the impact, outcome and plan for the patient and family.
All entries should be accurate and relevant to the individual patient - non-specific information such as ‘ongoing management’ is not useful.
Duplication should be avoided - statements about information recorded in other activities on the EMR are not useful, for example, ‘medications given as per MAR’.
Professional nursing language should be used for all entries - abbreviations should be used minimally and must be consistent with RCH standards, for example, ‘emotional support was provided to child family’ could be documented instead of ‘TLC was given’. See Medical Acronyms and abbreviations list.
Real time notes should be signed off after the first entry and subsequent entries are entered as addendums.
Example of
real time progress note entry:
09:40
NURSING. Billie is describing increasing pain in left leg. FLACC 7/10. Paracetamol given; heat pack applied with some effect. Education given to Mum at the bedside on utilising heat pack in conjunction with regular analgesia. Continue pain score
with observations. (Progress Note, sign at the end)
10:15
NURSING. Episode of urinary incontinence. Billie quite embarrassed. Urine bottle given. (Addendum)
14:30
NURSING. Routine bloods for IV therapy taken, lab called- high K+ (? Haemolysed). Medical staff notified, repeat bloods in 6/24. Encourage oral fluids and diet, if tolerated. IV can be removed. (Addendum)
Companion Documents
Evidence Table
The evidence table for this guideline can be viewed here. -- Coming soon
Please remember to read the
disclaimer.
The revision of this nursing guideline was coordinated by Stacey Richards, CNC, Nursing Research and approved by the Nursing Clinical Effectiveness Committee. Updated February 2023.